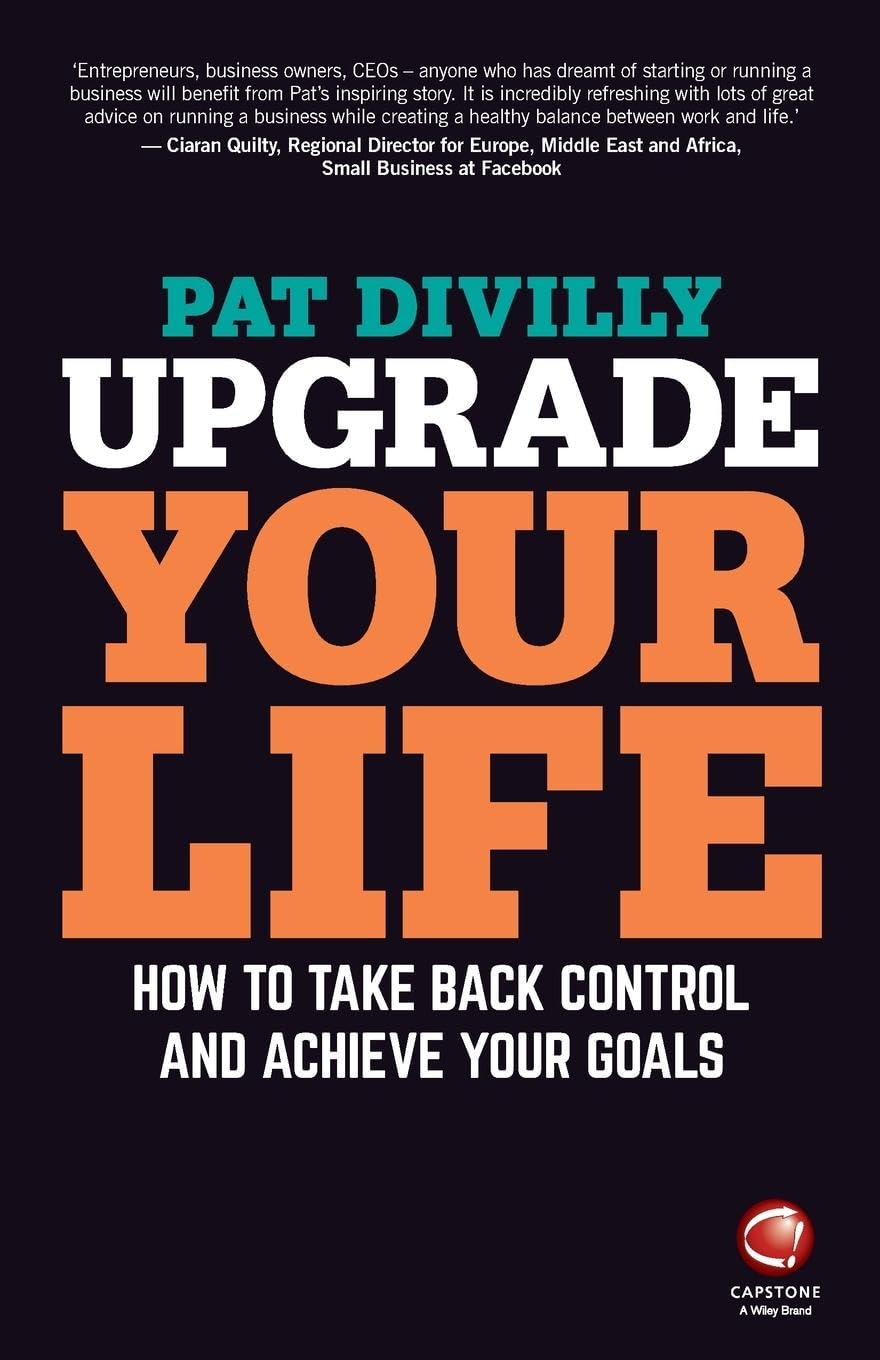
Upgrade Your Life – by Pat Divilly
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pat Divilly takes us through the steps to establish what it is we want out of life, adopt daily habits of success, build our self-esteem and confidence, and pursue what’s actually fulfilling, whatever that is for us as individuals.
The general layout of the book is: first, figuring out where you genuinely want to go (not just where people expect you to want to go!), and then seeing about what things you can change, first small and then larger, to get there.
The scope of the book covers work life and personal life, and treats them both as something where you can optimize how things work for you, and those around you. All in all, unless your life is literally perfect in every way imaginable, there’s probably something in this book that will help you to, indeed, “upgrade your life”. And who wouldn’t want that?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rebounding Into The Best Of Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Trampoline” is a brand-name that’s been popularized as a generic name, and “rebounding”, the name used in this video, is the same thing as “trampolining”. With that in mind, let us bounce swiftly onwards:
Surprising benefits
It’s easy to think “isn’t that cheating?” to the point that such “cheating” could be useless, since surely the device is doing most of the work?
The thing is, while indeed it’s doing a lot of the work for you, your muscles are still doing a lot—mostly stabilization work, which is of course a critical thing for our muscles to be able to do. While it’s rare that we need to do a somersault in everyday life, it’s common that we have to keep ourselves from falling over, after all.
It also represents a kind of gentle resistance exercise, and as such, improves bone density—something first discovered during NASA research for astronauts. Other related benefits pertain to the body’s ability to deal with acceleration and deceleration; it also benefits the lymphatic system, which unlike the blood’s circulatory system, has no pump of its own. Rebounding does also benefit the cardiovascular system, though, as now the heart gets confused (in the healthy way, a little like it gets confused with high-intensity interval training).
Those are the main evidence-based benefits; anecdotally (but credibly, since these things can be said of most exercise) it’s also claimed that it benefits posture, improves sleep and mood, promotes weight loss and better digestion, reduces bloating, improves skin (the latter being due to improved circulation), and alleviates arthritis (most moderate exercise improves immune response, and thus reduces chronic inflammation, so again, this is reasonable, even if anecdotal).
For more details on all of these and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Exercise Less, Move More
- How To Do HIIT (Without Wrecking Your Body)
- Resistance Is Useful! (Especially As We Get Older)
- HIIT, But Make It HIRT
- The Lymphatic System Against Cancer & More
Take care!
Share This Post
-
Aging with Grace – by Dr. David Snowdon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a book about Christianity. Don’t worry, we didn’t suddenly change the theme of 10almonds.
Rather, what this book is: a book about a famous large (n=678) study into the biology of aging, that took a population sample of women who had many factors already controlled-for, e.g. they ate the same food, had the same schedule, did the same activities, etc—for many years on end. In other words, a convent of nuns.
This allowed for a lot more to be learned about other factors that influence aging, such as:
- Heredity / genetics in general
- Speaking more than one language
- Supplementing with vitamins or not
- Key adverse events (e.g. stroke)
- Key chronic conditions (e.g. depression)
The book does also cover (as one might expect) the role that community and faith can play in healthy longevity, but since the subjects were 678 communally-dwelling people of faith (thus: no control group of faithless loners), this aspect is discussed only in anecdote, or in reference to other studies.
The author of this book, by the way, was the lead researcher of the study, and he is a well-recognised expert in the field of Alzheimer’s in particular (and Alzheimer’s does feature quite a bit throughout).
The writing style is largely narrative, and/but with a lot of clinical detail and specific data; this is by no means a wishy-washy book.
Bottom line: if you’d like to know what nuns were doing in the 1980s to disproportionally live into three-figure ages, then this book will answer those questions.
Click here to check out Aging with Grace, and indeed age with grace!
Share This Post
-
The surprising ways ‘swimming off’ a hangover can be risky, even if alcohol has left your system
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s the morning after a big night and you’re feeling the effects of too much alcohol.
So it can be tempting to “refresh” and take the edge off a hangover with a swim at the beach, or a dip in the cool waters of your local river or pool.
But you might want to think twice.
The day after heavy drinking can affect your body, energy levels and perception of risk in many ways. This means you’re more likely to drown or make careless decisions – even without high levels of alcohol in your blood.
Wanderlust Media/Shutterstock Alcohol + water + summer = drowning
Alcohol is one of the main reasons why someone’s more likely to die due to drowning. And Australians consume a lot of it, including around the water.
The risk of drowning, and injury, including incidents involving alcohol, dramatically increases over the summer festive period – in particular on public holidays and long weekends.
Among people aged 18 and over who drowned in rivers where alcohol was involved, we found some 40% had a blood alcohol concentration of at least 0.20%. That’s four times the upper legal limit of 0.05% when driving a car on a full licence.
When we breathalysed people at four Australian rivers, we found higher levels of blood alcohol with higher temperatures, and particularly on public holidays.
At the beach, intoxication due to alcohol and/or drugs is involved in 23% of drowning deaths with an average blood alcohol concentration of 0.19%.
How about if you’re hungover?
Getting alcohol out of your body is a relatively slow process. On average, alcohol is metabolised at a rate of 0.015% per hour. So if someone stops drinking at 2am with a blood alcohol concentration of 0.20%, their alcohol levels don’t drop to zero until 4pm the next day.
Although hangovers can vary from person to person, typical symptoms include headache, muscle aches, fatigue, weakness, thirst, nausea, stomach pain, vertigo, irritability, sensitivity to light and sound, anxiety, sweating and increased blood pressure.
As well as feeling a bit dusty, the day after an evening of heavy drinking, you’re not so good at identifying risks and reacting to them.
In a pool, this might mean not noticing it’s too shallow to dive safely. In natural waterways, this might mean not noticing a strong river current or a rip current at the beach. Or someone might notice these hazards but swim or dive in anyway.
You don’t have to have alcohol in your blood to be affected. Fatigue can set in, leading you to make careless decisions. tismaja/Shutterstock In one study, we found that after a four-day Australian music festival where people drank heavily, even people who were sober (no longer had alcohol in their blood) were still affected.
Compared to baseline tests in the lab we ran three weeks before the festival, people who were sober the day after the festival had faster reaction times in a test to gauge their attention. But they made more mistakes. This suggests hangovers coupled with fatigue lead to quicker but more careless behaviour.
In and around water this could be the difference between life and death.
Positive blood alcohol readings, including of alcohol from the night before, are commonly implicated in drowning deaths as a result of risky behaviours such as jumping into the water, both at a river and along the coast. Jumping can cause physical injury or render you unconscious, leading to drowning.
Alcohol, including the day after drinking, can also make drowning more likely for a number of other reasons. It also reduces people’s coordination and reaction times.
What else is going on?
Alcohol makes the blood vessels near your skin open up (dilate). So more blood flows into them, making you feel hot. This means you may stay in colder water for longer, increasing your risk of hypothermia.
Alcohol can even make CPR (cardiopulmonary resuscitation) less effective, should you need to be resuscitated.
Normally, your body controls levels of certain minerals (or electrolytes) in the blood. But electrolyte imbalance is common after heavy drinking, including the day after. It’s the reason why hangover symptoms such as muscle pain can lead to cramps in your arms or legs. This can become dangerous when being in or on the water.
Low blood sugar levels the day after drinking is also common. This can lead to people becoming exhausted more quickly when doing physical activities, including swimming.
Other hazards include cold water, high waves and deep water, all of which your body may not be capable of dealing with if you’re feeling the effects of a big night.
What can we do about it?
Authorities regularly warn about the dangers of alcohol intoxication and being near the water. Young people and men are often targeted because these are the groups more likely to drown where alcohol is involved.
Beaches may have alcohol-free zones. Rivers rarely have the same rules, despite similar dangers. https://www.youtube.com/embed/5Salt-kkGUo?wmode=transparent&start=0 Royal Life Saving urges men to ‘make the right call’ and avoid alcohol around the water.
How to stay safe around water if you’re drinking
So take care this summer and stay out of the water if you’re not feeling your best:
- do your swimming before your drinking
- look out for your mates, especially ones who may have had a few too many or are hungover
- avoid getting back into the water after you’ve drunk alcohol or if you’re not feeling your best the next day.
Amy Peden, NHMRC Research Fellow, School of Population Health & co-founder UNSW Beach Safety Research Group, UNSW Sydney; Emmanuel Kuntsche, Director of the Centre for Alcohol Policy Research, La Trobe University, and Jasmin C. Lawes, Adjunct Senior Lecturer, UNSW Beach Safety Research Group, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hearing loss is twice as common in Australia’s lowest income groups, our research shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Around one in six Australians has some form of hearing loss, ranging from mild to complete hearing loss. That figure is expected to grow to one in four by 2050, due in a large part to the country’s ageing population.
Hearing loss affects communication and social engagement and limits educational and employment opportunities. Effective treatment for hearing loss is available in the form of communication training (for example, lipreading and auditory training), hearing aids and other devices.
But the uptake of treatment is low. In Australia, publicly subsidised hearing care is available predominantly only to children, young people and retirement-age people on a pension. Adults of working age are mostly not eligible for hearing health care under the government’s Hearing Services Program.
Our recent study published in the journal Ear and Hearing showed, for the first time, that working-age Australians from lower socioeconomic backgrounds are at much greater risk of hearing loss than those from higher socioeconomic backgrounds.
We believe the lack of socially subsidised hearing care for adults of working age results in poor detection and care for hearing loss among people from disadvantaged backgrounds. This in turn exacerbates social inequalities.
Population data shows hearing inequality
We analysed a large data set called the Household, Income and Labour Dynamics in Australia (HILDA) survey that collects information on various aspects of people’s lives, including health and hearing loss.
Using a HILDA sub-sample of 10,719 working-age Australians, we evaluated whether self-reported hearing loss was more common among people from lower socioeconomic backgrounds than for those from higher socioeconomic backgrounds between 2008 and 2018.
Relying on self-reported hearing data instead of information from hearing tests is one limitation of our paper. However, self-reported hearing tends to underestimate actual rates of hearing impairment, so the hearing loss rates we reported are likely an underestimate.
We also wanted to find out whether people from lower socioeconomic backgrounds were more likely to develop hearing loss in the long run.
Hearing care is publicly subsidised for children.
mady70/ShutterstockWe found people in the lowest income groups were more than twice as likely to have hearing loss than those in the highest income groups. Further, hearing loss was 1.5 times as common among people living in the most deprived neighbourhoods than in the most affluent areas.
For people reporting no hearing loss at the beginning of the study, after 11 years of follow up, those from a more deprived socioeconomic background were much more likely to develop hearing loss. For example, a lack of post secondary education was associated with a more than 1.5 times increased risk of developing hearing loss compared to those who achieved a bachelor’s degree or above.
Overall, men were more likely to have hearing loss than women. As seen in the figure below, this gap is largest for people of low socioeconomic status.
Why are disadvantaged groups more likely to experience hearing loss?
There are several possible reasons hearing loss is more common among people from low socioeconomic backgrounds. Noise exposure is one of the biggest risks for hearing loss and people from low socioeconomic backgrounds may be more likely to be exposed to damaging levels of noise in jobs in mining, construction, manufacturing, and agriculture.
Lifestyle factors which may be more prevalent in lower socioeconomic communities such as smoking, unhealthy diet, and a lack of regular exercise are also related to the risk of hearing loss.
Finally, people with lower incomes may face challenges in accessing timely hearing care, alongside competing health needs, which could lead to missed identification of treatable ear disease.
Why does this disparity in hearing loss matter?
We like to think of Australia as an egalitarian society – the land of the fair go. But nearly half of people in Australia with hearing loss are of working age and mostly ineligible for publicly funded hearing services.
Hearing aids with a private hearing care provider cost from around A$1,000 up to more than $4,000 for higher-end devices. Most people need two hearing aids.
Hearing loss might be more common in low income groups because they’re exposed to more noise at work.
Dmitry Kalinovsky/ShutterstockLack of access to affordable hearing care for working-age adults on low incomes comes with an economic as well as a social cost.
Previous economic analysis estimated hearing loss was responsible for financial costs of around $20 billion in 2019–20 in Australia. The largest component of these costs was productivity losses (unemployment, under-employment and Jobseeker social security payment costs) among working-age adults.
Providing affordable hearing care for all Australians
Lack of affordable hearing care for working-age adults from lower socioeconomic backgrounds may significantly exacerbate the impact of hearing loss among deprived communities and worsen social inequalities.
Recently, the federal government has been considering extending publicly subsidised hearing services to lower income working age Australians. We believe reforming the current government Hearing Services Program and expanding eligibility to this group could not only promote a more inclusive, fairer and healthier society but may also yield overall cost savings by reducing lost productivity.
All Australians should have access to affordable hearing care to have sufficient functional hearing to achieve their potential in life. That’s the land of the fair go.
Mohammad Nure Alam, PhD Candidate in Economics, Macquarie University; Kompal Sinha, Associate Professor, Department of Economics, Macquarie University, and Piers Dawes, Professor, School of Health and Rehabilitation Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Never Too Old?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Age Limits On Exercise?
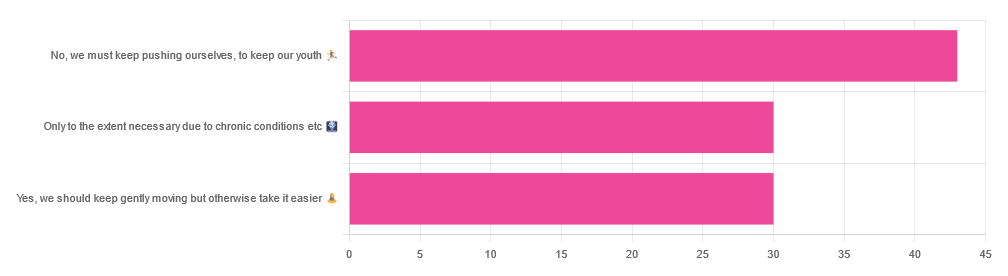
In Tuesday’s newsletter, we asked you your opinion on whether we should exercise less as we get older, and got the above-depicted, below-described, set of responses:
- About 42% said “No, we must keep pushing ourselves, to keep our youth“
- About 29% said “Only to the extent necessary due to chronic conditions etc”
- About 29% said “Yes, we should keep gently moving but otherwise take it easier”
One subscriber who voted for “No, we must keep pushing ourselves, to keep our youth“ wrote to add:
❝I’m 71 and I push myself. I’m not as fast or strong as I used to be but, I feel great when I push myself instead of going through the motions. I listen to my body!❞
~ 10almonds subscriber
One subscriber who voted for “Only to the extent necessary due to chronic conditions etc” wrote to add:
❝It’s never too late to get stronger. Important to keep your strength and balance. I am a Silver Sneakers instructor and I see first hand how helpful regular exercise is for seniors.❞
~ 10almonds subscriber
One subscriber who voted to say “Yes, we should keep gently moving but otherwise take it easier” wrote to add:
❝Keep moving but be considerate and respectful of your aging body. It’s a time to find balance in life and not put yourself into a positon to damage youself by competing with decades younger folks (unless you want to) – it will take much longer to bounce back.❞
~ 10almonds subscriber
These will be important, because we’ll come back to them at the end.
So what does the science say?
Endurance exercise is for young people only: True or False?
False! With proper training, age is no barrier to serious endurance exercise.
Here’s a study that looked at marathon-runners of various ages, and found that…
- the majority of middle-aged and elderly athletes have training histories of less than seven years of running
- there are virtually no relevant running time differences (p<0.01) per age in marathon finishers from 20 to 55 years
- after 55 years, running times did increase on average, but not consistently (i.e. there were still older runners with comparable times to the younger age bracket)
The researchers took this as evidence of aging being indeed a biological process that can be sped up or slowed down by various lifestyle factors.
See also:
Age & Aging: What Can (And Can’t) We Do About It?
this covers the many aspects of biological aging (it’s not one number, but many!) and how our various different biological ages are often not in sync with each other, and how we can optimize each of them that can be optimized
Resistance training is for young people only: True or False?
False! In fact, it’s not only possible for older people, but is also associated with a reduction in all-cause mortality.
Specifically, those who reported strength-training at least once per week enjoyed longer lives than those who did not.
You may be thinking “is this just the horse-riding thing again, where correlation is not causation and it’s just that healthier people (for other reasons) were able to do strength-training more, rather than the other way around?“
…which is a good think to think of, so well-spotted if you were thinking that!
But in this case no; the benefits remained when other things were controlled for:
❝Adjusted for demographic variables, health behaviors and health conditions, a statistically significant effect on mortality remained.
Although the effects on cardiac and cancer mortality were no longer statistically significant, the data still pointed to a benefit.
Importantly, after the physical activity level was controlled for, people who reported strength exercises appeared to see a greater mortality benefit than those who reported physical activity alone.❞
See the study: Is strength training associated with mortality benefits? A 15 year cohort study of US older adults
And a pop-sci article about it: Strength training helps older adults live longer
Closing thoughts
As it happens… All three of the subscribers we quoted all had excellent points!
Because in this case it’s less a matter of “should”, and more a selection of options:
- We (most of us, at least) can gain/regain/maintain the kind of strength and fitness associated with much younger people, and we need not be afraid of exercising accordingly (assuming having worked up to such, not just going straight from couch to marathon, say).
- We must nevertheless be mindful of chronic conditions or even passing illnesses/injuries, but that goes for people of any age
- We also can’t argue against a “safety first” cautious approach to exercise. After all, sure, maybe we can run marathons at any age, but that doesn’t mean we have to. And sure, maybe we can train to lift heavy weights, but if we’re content to be able to carry the groceries or perhaps take our partner’s weight in the dance hall (or the bedroom!), then (if we’re also at least maintaining our bones and muscles at a healthy level) that’s good enough already.
Which prompts the question, what do you want to be able to do, now and years from now? What’s important to you?
For inspiration, check out: Train For The Event Of Your Life!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: