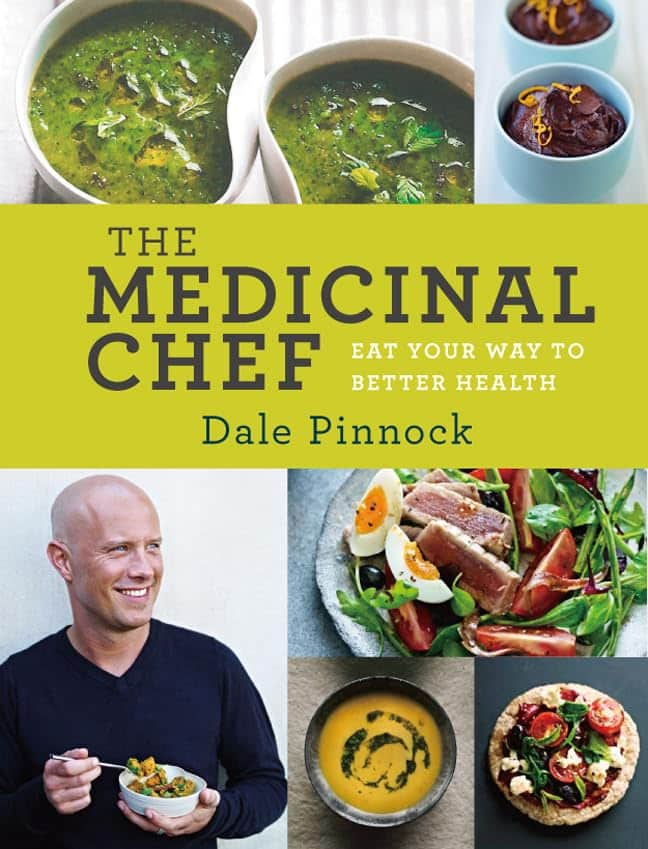
The Medicinal Chef – by Dale Pinnock
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The philosophy here is very much like our own—to borrow from Hippocrates: “let food be thy medicine”. Obviously please do also let medicine be thy medicine if you need it, but the point is that food is a very good starting place for combatting a lot of disease.
To this end, instead of labelling the recipes with such things as “V”, “Ve”, “GF” and suchlike, it assumes we can tell those things from the ingredients lists, and instead labels things per what they are especially good for:
- S: skin
- J: joints & bones
- R: respiratory system
- I: immune system
- M: metabolic health
- N: nervous system and mental health
- H: heart and circulation
- D: digestive system
- U: reproductive & urinary systems
As for the recipes themselves… They’re a lot like the recipes we share here at 10almonds in their healthiness, skill level, and balance of easy-to-find ingredients with the occasional “order it online” items that punch above their weight. In fact, we’ll probably modify some of the recipes for sharing here.
Bottom line: if you’re looking for genuinely healthy recipes that are neither too basic nor too arcane, this book has about 80 of them.
Click here to check out The Medicinal Chef: Healthy Every Day, and be healthy every day!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From eye exams to blood tests and surgery: how doctors use light to diagnose disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
You’re not feeling well. You’ve had a pounding headache all week, dizzy spells and have vomited up your past few meals.
You visit your GP to get some answers and sit while they shine a light in your eyes, order a blood test and request some medical imaging.
Everything your GP just did relies on light. These are just some of the optical technologies that have had an enormous impact in how we diagnose disease.
megaflopp/Shutterstock 1. On-the-spot tests
Point-of-care diagnostics allow doctors to test patients on the spot and get answers in minutes, rather than sending samples to a lab for analysis.
The “flashlight” your GP uses to view the inside of your eye (known as an ophthalmoscope) is a great example. This allows doctors to detect abnormal blood flow in the eye, deformations of the cornea (the outermost clear layer of the eye), or swollen optical discs (a round section at the back of the eye where the nerve link to the brain begins). Swollen discs are a sign of elevated pressure inside your head (or in the worst case, a brain tumour) that could be causing your headaches.
The invention of lasers and LEDs has enabled many other miniaturised technologies to be provided at the bedside or clinic rather than in the lab.
Pulse oximetry is a famous example, where a clip attached to your finger reports how well your blood is oxygenated. It does this by measuring the different responses of oxygenated and de-oxygenated blood to different colours of light.
Pulse oximetry is used at hospitals (and sometimes at home) to monitor your respiratory and heart health. In hospitals, it is also a valuable tool for detecting heart defects in babies.
See that clip on the patient’s finger? That’s a pulse oximeter, which relies on light to monitor respiratory and heart health. CGN089/Shutterstock 2. Looking at molecules
Now, back to that blood test. Analysing a small amount of your blood can diagnose many different diseases.
A machine called an automated “full blood count analyser” tests for general markers of your health. This machine directs focused beams of light through blood samples held in small glass tubes. It counts the number of blood cells, determines their specific type, and reports the level of haemoglobin (the protein in red blood cells that distributes oxygen around your body). In minutes, this machine can provide a snapshot of your overall health.
For more specific disease markers, blood serum is separated from the heavier cells by spinning in a rotating instrument called a centrifuge. The serum is then exposed to special chemical stains and enzyme assays that change colour depending on whether specific molecules, which may be the sign of a disease, are present.
These colour changes can’t be detected with the naked eye. However, a light beam from an instrument called a spectrometer can detect tiny amounts of these substances in the blood and determine if the biomarkers for diseases are present, and at what levels.
Light shines through the blood sample and tells us whether biomarkers for disease are present. angellodeco/Shutterstock 3. Medical imaging
Let’s re-visit those medical images your GP ordered. The development of fibre-optic technology, made famous for transforming high-speed digital communications (such as the NBN), allows light to get inside the body. The result? High-resolution optical imaging.
A common example is an endoscope, where fibres with a tiny camera on the end are inserted into the body’s natural openings (such as your mouth or anus) to examine your gut or respiratory tracts.
Surgeons can insert the same technology through tiny cuts to view the inside of the body on a video screen during laparoscopic surgery (also known as keyhole surgery) to diagnose and treat disease.
Doctors can insert this flexible fibre-optic tube with a camera on the end into your body. Eduard Valentinov/Shutterstock How about the future?
Progress in nanotechnology and a better understanding of the interactions of light with our tissues are leading to new light-based tools to help diagnose disease. These include:
- nanomaterials (materials on an extremely small scale, many thousands of times smaller than the width of a human hair). These are being used in next-generation sensors and new diagnostic tests
- wearable optical biosensors the size of your fingernail can be included in devices such as watches, contact lenses or finger wraps. These devices allow non-invasive measurements of sweat, tears and saliva, in real time
- AI tools to analyse how blood serum scatters infrared light. This has allowed researchers to build a comprehensive database of scatter patterns to detect any cancer
- a type of non-invasive imaging called optical coherence tomography for more detailed imaging of the eye, heart and skin
- fibre optic technology to deliver a tiny microscope into the body on the tip of a needle.
So the next time you’re at the GP and they perform (or order) some tests, chances are that at least one of those tests depend on light to help diagnose disease.
Matthew Griffith, Associate Professor and ARC Future Fellow and Director, UniSA Microscopy and Microanalysis Facilities, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Hazelnuts vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to cashews, we picked the hazelnuts.
Why?
It’s close! This one’s interesting…
In terms of macros, hazelnuts have more fiber and fats, while cashews have more protein and carbs. All in all, all good stuff all around; maybe a win for one or the other depending on your priorities. We’d pick hazelnuts here, but your preference may vary.
When it comes to vitamins, hazelnuts have more of vitamins A, B1, B2, B3, B5, B6, B9, C, and E, while cashews have more vitamin K. An easy win for hazelnuts here, and the margins weren’t close.
In the category of minerals, hazelnuts have more calcium, manganese, and potassium, while cashews have more copper, iron, magnesium, phosphorus, selenium, and zinc. This is a win for cashews, but it’s worth noting that cup for cup, both of these nuts provide more than the daily requirement of most of those minerals. This means that in practical terms, it doesn’t matter too much that (for example), while cashews provide 732% of the daily requirement for copper, hazelnuts “only” provide 575%. So while this category remains a victory for cashews, it’s something of a “on paper” thing for the most part.
Adding up the sections (ambivalent + clear win for hazelnuts + nominal win for cashews) means that in total today we’re calling it in favour of hazelnuts… But as ever, enjoy both, because both are good and so is diversity!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
-
Surgery won’t fix my chronic back pain, so what will?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s ABC Four Corners episode Pain Factory highlighted that our health system is failing Australians with chronic pain. Patients are receiving costly, ineffective and risky care instead of effective, low-risk treatments for chronic pain.
The challenge is considering how we might reimagine health-care delivery so the effective and safe treatments for chronic pain are available to millions of Australians who suffer from chronic pain.
One in five Australians aged 45 and over have chronic pain (pain lasting three or more months). This costs an estimated A$139 billion a year, including $12 billion in direct health-care costs.
The most common complaint among people with chronic pain is low back pain. So what treatments do – and don’t – work?
Opioids and invasive procedures
Treatments offered to people with chronic pain include strong pain medicines such as opioids and invasive procedures such as spinal cord stimulators or spinal fusion surgery. Unfortunately, these treatments have little if any benefit and are associated with a risk of significant harm.
Spinal fusion surgery and spinal cord stimulators are also extremely costly procedures, costing tens of thousands of dollars each to the health system as well as incurring costs to the individual.
Addressing the contributors to pain
Recommendations from the latest Australian and World Health Organization clinical guidelines for low back pain focus on alternatives to drug and surgical treatments such as:
- education
- advice
- structured exercise programs
- physical, psychological or multidisciplinary interventions that address the physical or psychological contributors to ongoing pain.
Pain education is central. Monkey Business Images/Shutterstock Two recent Australian trials support these recommendations and have found that interventions that address each person’s physical and psychological contributors to pain produce large and sustained improvements in pain and function in people with chronic low back pain.
The interventions have minimal side effects and are cost-effective.
In the RESOLVE trial, the intervention consists of pain education and graded sensory and movement “retraining” aimed to help people understand that it’s safe to move.
In the RESTORE trial, the intervention (cognitive functional therapy) involves assisting the person to understand the range of physical and psychological contributing factors related to their condition. It guides patients to relearn how to move and to build confidence in their back, without over-protecting it.
Why isn’t everyone with chronic pain getting this care?
While these trials provide new hope for people with chronic low back pain, and effective alternatives to spinal surgery and opioids, a barrier for implementation is the out-of-pocket costs. The interventions take up to 12 sessions, lasting up to 26 weeks. One physiotherapy session can cost $90–$150.
In contrast, Medicare provides rebates for just five allied health visits (such as physiotherapists or exercise physiologists) for eligible patients per year, to be used for all chronic conditions.
Private health insurers also limit access to reimbursement for these services by typically only covering a proportion of the cost and providing a cap on annual benefits. So even those with private health insurance would usually have substantial out-of-pocket costs.
Access to trained clinicians is another barrier. This problem is particularly evident in regional and rural Australia, where access to allied health services, pain specialists and multidisciplinary pain clinics is limited.
Higher costs and lack of access are associated with the increased use of available and subsidised treatments, such as pain medicines, even if they are ineffective and harmful. The rate of opioid use, for example, is higher in regional Australia and in areas of socioeconomic disadvantage than metropolitan centres and affluent areas.
So what can we do about it?
We need to reform Australia’s health system, private and public, to improve access to effective treatments for chronic pain, while removing access to ineffective, costly and high-risk treatments.
Better training of the clinical workforce, and using technology such as telehealth and artificial intelligence to train clinicians or deliver treatment may also improve access to effective treatments. A recent Australian trial, for example, found telehealth delivered via video conferencing was as effective as in-person physiotherapy consultations for improving pain and function in people with chronic knee pain.
Advocacy and improving the public’s understanding of effective treatments for chronic pain may also be helpful. Our hope is that coordinated efforts will promote the uptake of effective treatments and improve the care of patients with chronic pain.
Christine Lin, Professor, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Fiona Blyth, Professor, University of Sydney; James Mcauley, Professor of Psychology, UNSW Sydney, and Mark Hancock, Professor of Physiotherapy, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Is Unnoticed Environmental Mold Harming Your Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Environmental mold can be a lot more than just the famously toxic black mold that sometimes makes the headlines, and many kinds you might not notice, but it can colonizes your sinuses and gut just the same:
Breaking the mold
Around 25% of homes in North America are estimated to have mold, though the actual number is likely to be higher, affecting both older and new homes. For that matter, mold can grow in unexpected areas, like inside air conditioning units, even in dry regions.
If mold just sat where it is minding its own business, it might not be so bad, but instead they release their spores, which are de facto airborne mycotoxins, which can colonize places like the sinuses or gut, causing significant health issues.
Not everyone in the same household is affected the same way by mold due to genetic differences and varying pre-existing health conditions. But as a general rule of thumb, mold inflames the brain, nerves, gut, and skin, and can negatively impact the vagal nerve, which is linked to the gut-brain connection. Mycotoxins also damage mitochondria, leading to symptoms like fatigue, brain fog, and cognitive issues. To complicate matters further, mold illness can mimic other conditions like anxiety, chronic fatigue, fibromyalgia, IBS, and more, making it difficult to diagnose.
Testing is possible, though they all have limitations, e.g:
- Home testing: testing the home for mold spores and mycotoxins is crucial for effective treatment; professional mold remediation companies are a good idea (to do a thorough job of cleaning, without also breathing in half the mold while cleaning it).
- Mold allergy testing: mold allergy testing (IgE testing or skin tests) is often used, but it doesn’t diagnose mold-related illnesses linked to severe symptoms like fatigue or neurodegeneration.
- Serum antibody testing: tests for immune reactions (IgG) to mycotoxins may not always show positive results if the immune system is weakened by long-term exposure.
- Urine mycotoxin testing: urine tests can detect mycotoxins in the body, though are likely to be more expensive, being probably not covered by public health in Canada or insurance in the US.
- Organic acid testing: this urine test can indicate mold colonization in areas like the sinuses or gut. Again, cost/availability may vary, though.
For more information on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is thirst a good predictor of dehydration?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Water is essential for daily functioning and health, and we can only survive a few days without it. Yet we constantly lose water through sweat, urination and even evaporation when we breathe.
This is why we have evolved a way to regulate and maintain water in our bodies. Like other animals, our survival relies on a strong biological drive that tells us to find and drink water to balance fluid loss.
This is thirst – a sensation of dryness in the mouth signalling we need to have a drink. This basic physiological mechanism is controlled mainly by part of the brain’s “control centre”, called the hypothalamus. The hypothalamus receives signals from various regions of the body and in return, releases hormones that act as a messenger to signal the thirst sensation.
KieferPix/Shutterstock What is dehydration?
Staying hydrated (having enough water in our bodies) is important for several reasons, including:
- regulating body temperature through sweat and respiration
- lubricating joints and eyes
- preventing infections
- digesting and absorbing nutrients
- flushing out waste (via the kidneys)
- preventing constipation
- brain function (including memory and concentration)
- mood and energy levels
- physical performance and recovery from exercise
- skin health.
Dehydration occurs when our body doesn’t have enough water. Even slight drops in fluid levels have noticeable consequences, such as headaches, feeling dizzy, lethargy and struggling to concentrate.
Chronic dehydration can pose more serious health risks, including urinary tract infections, constipation and kidney stones.
What does the evidence say?
Despite thirst being one of the most basic biological drivers for good hydration, science suggests our feelings of thirst and subsequent fluid intake don’t always correlate with hydration levels.
For example, a recent study explored the impact of thirst on fluid intake and hydration status. Participants attended a lab in the morning and then later in the afternoon to provide markers of hydration status (such as urine, blood samples and body weight). The relationship between levels of thirst in the morning and afternoon hydration status was negligible.
Further, thirst may be driven by environmental factors, such as access to water. For example, one study looked at whether ample access to water in a lab influenced how much people drank and how hydrated they were. The link between how thirsty they felt and how hydrated they were was weak, suggesting the availability of water influenced their fluid intake more than thirst.
Exercise can also change our thirst mechanism, though studies are limited at this stage.
Being thirsty doesn’t necessarily mean we’re dehydrated. puhhha/Shutterstock Interestingly, research shows women experience thirst more strongly than men, regardless of hydration status. To understand gender differences in thirst, researchers infused men and women with fluids and then measured their thirst and how hydrated they were. They found women generally reported thirst at a lower level of fluid loss. Women have also been found to respond more to feeling thirsty by drinking more water.
Other ways to tell if you need to drink some water
While acknowledging some people will need to drink more or less, for many people, eight cups (or two litres) a day is a good amount of water to aim for.
But beyond thirst, there are many other ways to tell whether you might need to drink more water.
1. urine colour: pale yellow urine typically indicates good hydration, while darker, concentrated urine suggests dehydration
2. frequency of going to the toilet: urinating regularly (around four to six times a day) indicates good hydration. Infrequent urination can signal dehydration
3. skin turgor test: gently pinching the skin (for example, on the back of the hand) and observing how quickly the skin returns to its normal position can help assess hydration. Slow return may indicate dehydration
If skin stays elevated after pinching it may be a sign of dehydration. SusaZoom/Shutterstock 4. mouth and lips: a dry mouth or cracked lips can be early signs of dehydration
5. headaches and fatigue: frequent headaches, dizziness, or unexplained fatigue can be signs of inadequate hydration
6. sweating: in physically active people, monitoring how much they sweat during activity can help estimate fluid loss and hydration needs. Higher levels of sweat may predispose a person to dehydration if they are unable to replace the fluid lost through water intake
These indicators, used together, provide a more comprehensive picture of hydration without solely depending on the sensation of thirst.
Of course, if you do feel thirsty, it’s still a good idea to drink some water.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Kiara Too, PhD candidate, School of Human Movement and Nutrition Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Complex PTSD – by Pete Walker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about Complex PTSD, but there’s a lot more to be said than we can fit into an article or two.
Pete Walker, a licensed marriage and family therapist, does an excellent job and pulls no punches, starting from the book’s dedication and carrying the hard-hitting seriousness all the way through to the Appendices.
To this end, it absolutely may not be an easy book to read at times (emotionally speaking), especially if you have C-PTSD. On the other hand, you may also find it a very validating 300-odd pages of “Yes, he is telling my life story in words, now this makes sense!”
That said, it’s mostly not an anecdotes-based book and nor is it just a feelsy ride; it’s also a textbook and a how-to manual. It’s a textbook of how and why things come about the way they do, and a manual of how to effectively manage C-PTSD, and find peace. There’s no silver bullet here, but there is a very comprehensive guide, and chapters full of tools to use (and no, not the same CBT things you’ve probably read a hundred times, this is C-PTSD-specific stuff).
Bottom line: this is the C-PTSD book; if you buy only one book on the topic, make it this one.
Click here to check out Complex PTSD: From Surviving To Thriving, and indeed thrive!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: