Rethinking Diabetes – by Gary Taubes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed this author’s “The Case Against Sugar” and “Why We Get Fat And What To Do About It“. There’s an obvious theme, and this book caps it off nicely:
By looking at the history of diabetes treatment (types 1 and 2) in the past hundred years, and analysing the patterns over time, we can see how:
- diabetics have been misled a lot over time by healthcare providers
- we can learn from those mistakes going forwards
Happily, he does this without crystal-balling the future or expecting diet to fix, for example, a pancreas that can’t produce insulin. But what he does do is focus on the “can” items rather than the “can’t” items.
In the category of criticism, one of the strategies he argues for is basically the keto diet, which is indeed just fine for diabetes but often not great for the heart in the long-term (it depends on various factors, including genes). However, even if you choose not to implement that, there is plenty more to try out in this book.
Bottom line: whether you have diabetes, love someone who does, or just plain like to be on top of your glycemic health, this book is full of important insights and opportunities to improve things progressively along the way.
Click here to check out Rethinking Diabetes, and rethink diabetes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Turns out the viral ‘Sleepy Girl Mocktail’ is backed by science. Should you try it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us wish we could get a better night’s sleep. Wouldn’t it be great if it was as easy as a mocktail before bed?
That’s what the latest viral trend might have us believe. The “Sleepy Girl Mocktail” is a mix of tart cherry juice, powdered magnesium supplement and soda water. TikTok videos featuring the concoction have garnered hundreds of thousands of views. But, what does the science say? Do these ingredients actually help us sleep?
Tart cherry juice
There is research to show including tart cherry juice in your diet improves overall sleep. Clinical trials show tart cherry juice increases sleep quality and quantity, as well as a lessening insomnia symptoms (compared to a placebo). This could be due to the presence of melatonin, a sleep-promoting hormone, in cherries.
Tart cherry varieties such as Jerte Valley or Montmorency have the highest concentration of melatonin (approximately 0.135 micrograms of melatonin per 100g of cherry juice). Over the counter melatonin supplements can range from 0.5 milligram to over 100 milligrams, with research suggesting those beginning to take melatonin start with a dose of 0.5–2 milligrams to see an improvement in sleep.
Melatonin naturally occurs in our bodies. Our body clock promotes the release of melatonin in the evening to help us sleep, specifically in the two hours before our natural bedtime.
If we want to increase our melatonin intake with external sources, such as cherries, then we should be timing our intake with our natural increase in melatonin. Supplementing melatonin too close to bed will mean we may not get the sleep-promoting benefits in time to get off to sleep easily. Taking melatonin too late may even harm our long-term sleep health by sending the message to our body clock to delay the release of melatonin until later in the evening.
Magnesium – but how much?
Magnesium also works to promote melatonin, and magnesium supplements have been shown to improve sleep outcomes.
However, results vary depending on the amount of magnesium people take. And we don’t yet have the answers on the best dose of magnesium for sleep benefits.
We do know magnesium plays a vital role in energy production and bone development, making it an important daily nutrient for our diets. Foods rich in magnesium include wheat cereal or bread, almonds, cashews, pumpkin seeds, spinach, artichokes, green beans, soy milk and dark chocolate.
Bubbly water
Soda water serves as the base of the drink, rather than a pathway to better sleep. And bubbly water may make the mix more palatable. It is important to keep in mind that drinking fluids close to bedtime can be disruptive to our sleep as it might lead to waking during the night to urinate.
Healthy sleep recommendations include avoiding water intake in the two hours before bed. Having carbonated beverages too close to bed can also trigger digestive symptoms such as bloating, gassiness and reflux during the night.
Bottoms up?
Overall, there is evidence to support trying out the Sleepy Girl Mocktail to see if it improves sleep, however there are some key things to remember:
timing: to get the benefits of this drink, avoid having it too close to bed. Aim to have it two hours before your usual bedtime and avoid fluids after this time
consistency: no drink is going to be an immediate cure for poor sleep. However, this recipe could help promote sleep if used strategically (at the right time) and consistently as part of a balanced diet. It may also introduce a calming evening routine that helps your brain relax and signals it’s time for bed
- maximum magnesium: be mindful of the amount of magnesium you are consuming. While there are many health benefits to magnesium, the recommended daily maximum amounts are 420mg for adult males and 320mg for adult females. Exceeding the maximum can lead to low blood pressure, respiratory distress, stomach problems, muscle weakness and mood problems
sugar: in some of the TikTok recipes sugar (as flavoured sodas, syrups or lollies) is added to the drink. While this may help hide the taste of the tart cherry juice, the consumption of sugar too close to bed may make it more difficult to get to sleep. And sugar in the evening raises blood sugar levels at a time when our body is not primed to be processing sugar. Long term, this can increase our risk of diabetes
sleep environment: follow good sleep hygiene practices including keeping a consistent bedtime and wake time, a wind-down routine before bed, avoiding electronic device use like phones or laptops in bed, and avoiding bright light in the evening. Bright light works to suppress our melatonin levels in the evening and make us more alert.
What about other drinks?
Other common evening beverages include herbal tisanes or teas, hot chocolate, or warm milk.
Milk can be especially beneficial for sleep, as it contains the amino acid tryptophan, which can promote melatonin production. Again, it is important to also consider the timing of these drinks and to avoid any caffeine in tea and too much chocolate too close to bedtime, as this can make us more alert rather than sleepy.
Getting enough sleep is crucial to our health and wellbeing. If you have tried multiple strategies to improve your sleep and things are not getting better, it may be time to seek professional advice, such as from a GP.
Charlotte Gupta, Postdoctoral research fellow, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Why are my muscles sore after exercise? Hint: it’s nothing to do with lactic acid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As many of us hit the gym or go for a run to recover from the silly season, you might notice a bit of extra muscle soreness.
This is especially true if it has been a while between workouts.
A common misunderstanding is that such soreness is due to lactic acid build-up in the muscles.
Research, however, shows lactic acid has nothing to do with it. The truth is far more interesting, but also a bit more complex.
It’s not lactic acid
We’ve known for decades that lactic acid has nothing to do with muscle soreness after exercise.
In fact, as one of us (Robert Andrew Robergs) has long argued, cells produce lactate, not lactic acid. This process actually opposes not causes the build-up of acid in the muscles and bloodstream.
Unfortunately, historical inertia means people still use the term “lactic acid” in relation to exercise.
Lactate doesn’t cause major problems for the muscles you use when you exercise. You’d probably be worse off without it due to other benefits to your working muscles.
Lactate isn’t the reason you’re sore a few days after upping your weights or exercising after a long break.
So, if it’s not lactic acid and it’s not lactate, what is causing all that muscle soreness?
Muscle pain during and after exercise
When you exercise, a lot of chemical reactions occur in your muscle cells. All these chemical reactions accumulate products and by-products which cause water to enter into the cells.
That causes the pressure inside and between muscle cells to increase.
This pressure, combined with the movement of molecules from the muscle cells can stimulate nerve endings and cause discomfort during exercise.
The pain and discomfort you sometimes feel hours to days after an unfamiliar type or amount of exercise has a different list of causes.
If you exercise beyond your usual level or routine, you can cause microscopic damage to your muscles and their connections to tendons.
Such damage causes the release of ions and other molecules from the muscles, causing localised swelling and stimulation of nerve endings.
This is sometimes known as “delayed onset muscle soreness” or DOMS.
While the damage occurs during the exercise, the resulting response to the injury builds over the next one to two days (longer if the damage is severe). This can sometimes cause pain and difficulty with normal movement.
The upshot
Research is clear; the discomfort from delayed onset muscle soreness has nothing to do with lactate or lactic acid.
The good news, though, is that your muscles adapt rapidly to the activity that would initially cause delayed onset muscle soreness.
So, assuming you don’t wait too long (more than roughly two weeks) before being active again, the next time you do the same activity there will be much less damage and discomfort.
If you have an exercise goal (such as doing a particular hike or completing a half-marathon), ensure it is realistic and that you can work up to it by training over several months.
Such training will gradually build the muscle adaptations necessary to prevent delayed onset muscle soreness. And being less wrecked by exercise makes it more enjoyable and more easy to stick to a routine or habit.
Finally, remove “lactic acid” from your exercise vocabulary. Its supposed role in muscle soreness is a myth that’s hung around far too long already.
Robert Andrew Robergs, Associate Professor – Exercise Physiology, Queensland University of Technology and Samuel L. Torrens, PhD Candidate, Queensland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
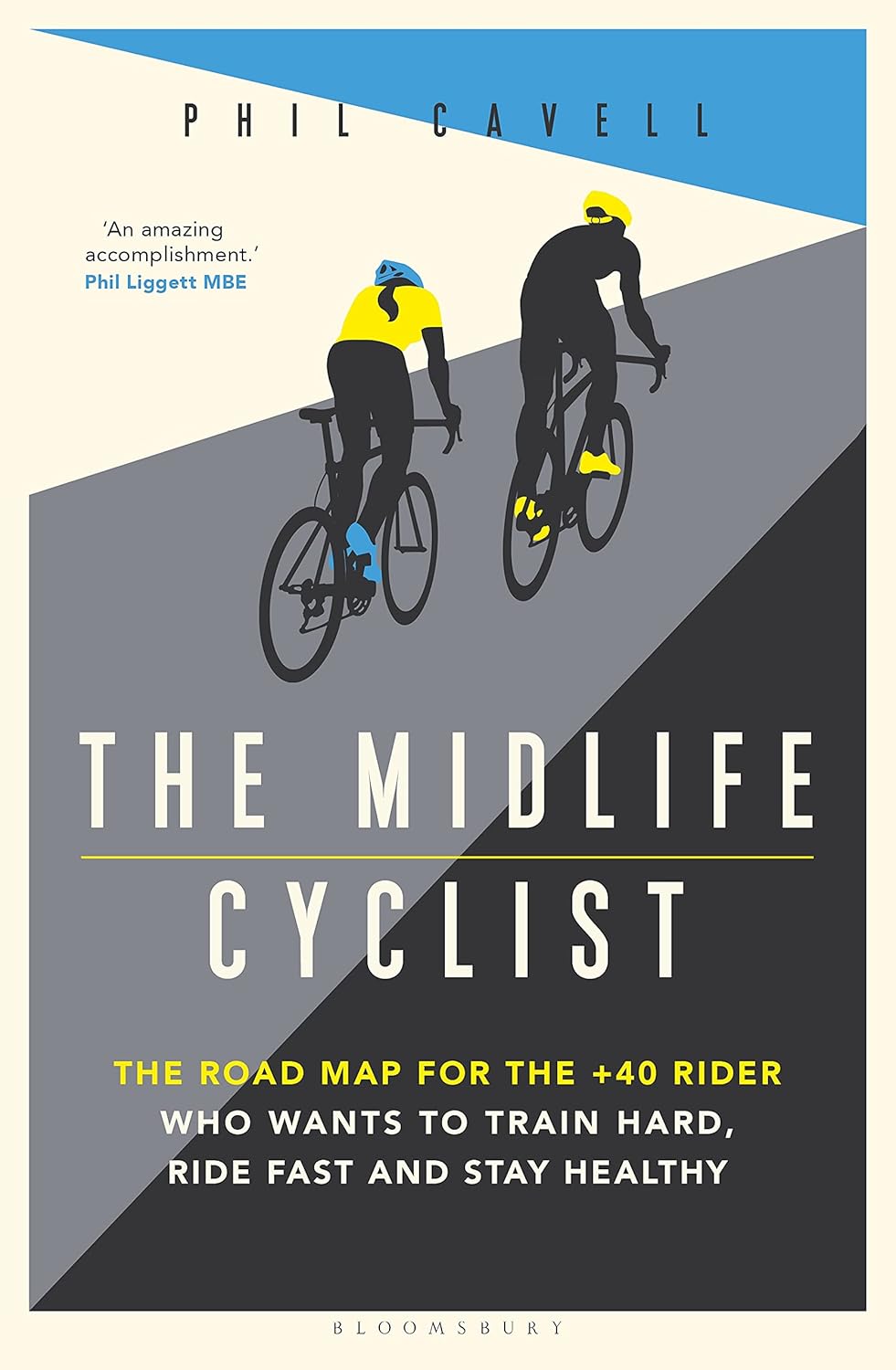
The Midlife Cyclist – by Phil Cavell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether stationary cycling in your living room, or competing in the Tour de France, there’s a lot more to cycling than “push the pedals”—if you want to get good benefits and avoid injury, in any case.
This book explores the benefits of different kinds of cycling, the biomechanics of various body positions, and the physiology of different kinds of performance, and the impact these things have on everything from your joints to your heart to your telomeres.
The style is very much conversational, with science included, and a readiness to acknowledge in cases where the author is guessing or going with a hunch, rather than something being well-evidenced. This kind of honesty is always good to see, and it doesn’t detract from where the science is available and clear.
One downside for some readers will be that while Cavell does endeavour to cover sex differences in various aspects of how they relate to the anatomy and physiology (mostly: the physiology) of cycling, the book is written from a male perspective and the author clearly understands that side of things better. For other readers, of course, this will be a plus.
Bottom line: if you enjoy cycling, or you’re thinking of taking it up but it seems a bit daunting because what if you do it wrong and need a knee replacement in a few years or what if you hurt your spine or something, then this is the book to set your mind at ease, and put you on the right track.
Click here to check out The Midlife Cyclist, and enjoy the cycle of life!
Share This Post
Related Posts
-
The Liver Cure – by Dr. Russell Blaylock
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about How To Unfatty A Fatty Liver, but there’s a lot more that can be said in a book that we couldn’t fit into our article.
In this book, Dr. Blaylock looks at the causes and symptoms of liver disease, the mechanisms behind such, and how we can adjust our dietary habits (and other things) to do better for ourselves.
While the book’s primary focus is on diet, he does also look at medications (especially: those that hinder liver health, which are many, including simple/common stuff like Tylenol and similar), and the effects of different lifestyle choices, including ones that aren’t diet-related.
Because most people’s knowledge of liver disease starts and ends at “don’t drink yourself to death”, this book is an important tome of knowledge for actually keeping this critical organ in good order—especially since symptoms of liver disease can initially be subtle, and slow to show, often escaping notice until it’s already far, far worse than it could have been.
Many people find out by experiencing liver failure.
The writing style is… A little repetitive for this reviewer’s preference, but it does make sure that you won’t miss things. Also, when it comes to supplements, he repeatedly recommends a particular company, and it’s not clear whether he has a financial interest there. But the actual medical information is good and important and comprehensive.
Bottom line: if you’d like to keep your liver in good health, this is a book that will help you to do just that.
Click here to check out The Liver Cure, and keep yours working well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resistance band Training – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those who’d like a full gym workout at home, without splashing out thousands on a home gym, resistance bands provide a lot of value. But how much value, really?
As James Atkinson demonstrates, there’s more exercise available than one might think.
Did you know that you can use the same band to strengthen your triceps as well as your biceps, for instance? and the same goes for your quadriceps and biceps femoris. And core strength? You bet.
The style here is not a sales pitch (though he does, at the end, offer extra resources if desired), but rather, instructional, and this book is in and of itself already a complete guide. With clear instructions and equally clear illustrations, you don’t need to spend a dime more (unless you don’t own a resistance band, in which case then yes, you will need one of those).
Bottom line: if you’d like to give your body the workout it deserves, this book is a potent resource.
Click here to check out Resistance Band Training, and get training!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
New study suggests weight loss drugs like Ozempic could help with knee pain. Here’s why there may be a link
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The drug semaglutide, commonly known by the brand names Ozempic or Wegovy, was originally developed to help people with type 2 diabetes manage their blood sugar levels.
However, researchers have discovered it may help with other health issues, too. Clinical trials show semaglutide can be effective for weight loss, and hundreds of thousands of people around the world are using it for this purpose.
Evidence has also shown the drug can help manage heart failure and chronic kidney disease in people with obesity and type 2 diabetes.
Now, a study published in the New England Journal of Medicine has suggested semaglutide can improve knee pain in people with obesity and osteoarthritis. So what did this study find, and how could semaglutide and osteoarthritis pain be linked?
Pormezz/Shutterstock Osteoarthritis and obesity
Osteoarthritis is a common joint disease, affecting 2.1 million Australians. Most people with osteoarthritis have pain and find it difficult to perform common daily activities such as walking. The knee is the joint most commonly affected by osteoarthritis.
Being overweight or obese is a major risk factor for osteoarthritis in the knee. The link between the two conditions is complex. It involves a combination of increased load on the knee, metabolic factors such as high cholesterol and high blood sugar, and inflammation.
For example, elevated blood sugar levels increase the production of inflammatory molecules in the body, which can damage the cartilage in the knee, and lead to the development of osteoarthritis.
Weight loss is strongly recommended to reduce the pain of knee osteoarthritis in people who are overweight or obese. International and Australian guidelines suggest losing as little as 5% of body weight can help.
But losing weight with just diet and exercise can be difficult for many people. One study from the United Kingdom found the annual probability of people with obesity losing 5% or more of their body weight was less than one in ten.
Semaglutide has recently entered the market as a potential alternative route to weight loss. It comes from a class of drugs known as GLP-1 receptor agonists and works by increasing a person’s sense of fullness.
Semaglutide for osteoarthritis?
The rationale for the recent study was that while we know weight loss alleviates symptoms of knee osteoarthritis, the effect of GLP-1 receptor agonists was yet to be explored. So the researchers set out to understand what effect semaglutide might have on knee osteoarthritis pain, alongside body weight.
They randomly allocated 407 people with obesity and moderate osteoarthritis into one of two groups. One group received semaglutide once a week, while the other group received a placebo. Both groups were treated for 68 weeks and received counselling on diet and physical activity. At the end of the treatment phase, researchers measured changes in knee pain, function, and body weight.
As expected, those taking semaglutide lost more weight than those in the placebo group. People on semaglutide lost around 13% of their body weight on average, while those taking the placebo lost around 3% on average. More than 70% of people in the semaglutide group lost at least 10% of their body weight compared to just over 9% of people in the placebo group.
Osteoarthritis of the knee is the most common type of osteoarthritis. SKT Studio/Shutterstock The study found semaglutide reduced knee pain significantly more than the placebo. Participants who took semaglutide reported an additional 14-point reduction in pain on a 0–100 scale compared to the placebo group.
This is much greater than the pain reduction in another recent study among people with obesity and knee osteoarthritis. This study investigated the effects of a diet and exercise program compared to an attention control (where participants are provided with information about nutrition and physical activity). The results here saw only a 3-point difference between the intervention group and the control group on the same scale.
The amount of pain relief reported in the semaglutide trial is also larger than that reported with commonly used pain medicines such as anti-inflammatories, opioids and antidepressants.
Semaglutide also improved knee function compared to the placebo. For example, people who took semaglutide could walk about 42 meters further than those on the placebo in a six-minute walking test.
How could semaglutide reduce knee pain?
It’s not fully clear how semaglutide helps with knee pain from osteoarthritis. One explanation may be that when a person loses weight, there’s less stress on the joints, which reduces pain.
But recent studies have also suggested semaglutide and other GLP-1 receptor agonists might have anti-inflammatory properties, and could even protect against cartilage wear and tear.
While the results of this new study are promising, it’s too soon to regard semaglutide as a “miracle drug” for knee osteoarthritis. And as this study was funded by the drug company that makes semaglutide, it will be important to have independent studies in the future, to confirm the findings, or not.
The study also had strict criteria, excluding some groups, such as those taking opioids for knee pain. One in seven Australians seeing a GP for their knee osteoarthritis are prescribed opioids. Most participants in the trial were white (61%) and women (82%). This means the study may not fully represent the average person with knee osteoarthritis and obesity.
It’s also important to consider semaglutide can have a range of side effects, including gastrointestinal symptoms and fatigue.
There are some concerns that semaglutide could reduce muscle mass and bone density, though we’re still learning more about this.
Further, it can be difficult to access.
I have knee osteoarthritis, what should I do?
Osteoarthritis is a disease caused by multiple factors, and it’s important to take a multifaceted approach to managing it. Weight loss is an important component for those who are overweight or obese, but so are other aspects of self-management. This might include physical activity, pacing strategies, and other positive lifestyle changes such as improving sleep, healthy eating, and so on.
Giovanni E. Ferreira, NHMRC Emerging Leader Research Fellow, Institute of Musculoskeletal Health, University of Sydney and Christina Abdel Shaheed, Associate Professor, School of Public Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: