How To Leverage Placebo Effect For Yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Placebo Effect: Making Things Work Since… Well, A Very Long Time Ago
The placebo effect is a well-known, well-evidenced factor that is very relevant when it comes to the testing and implementation of medical treatments:
NIH | National Center for Biotechnology Information | Placebo Effect
Some things that make placebo effect stronger include:
- Larger pills instead of small ones: because there’s got to be more going on in there, right?
- Thematically-colored pills: e.g. red for stimulant effects, blue for relaxing effects
- Things that seem expensive: e.g. a well-made large heavy machine, over a cheap-looking flimsy plastic device. Similarly, medication from a small glass jar with a childproof lock, rather than popped out from a cheap blister-pack.
- Things that seem rational: if there’s an explanation for how it works that you understand and find rational, or at least you believe you understand and find rational ← this works in advertising, too; if there’s a “because”, it lands better almost regardless of what follows the word “because”
- Things delivered confidently by a professional: this is similar to the “argument from authority” fallacy (whereby a proposed authority will be more likely trusted, even if this is not their area of expertise at all, e.g. celebrity endorsements), but in the case of placebo trials, this often looks like a well-dressed middle-aged or older man with an expensive haircut calling for a young confident-looking aide in a lab coat to administer the medicine, and is received better than a slightly frazzled academic saying “and, uh, this one’s yours” while handing you a pill.
- Things with ritual attached: this can be related to the above (the more pomp and circumstance is given to the administration of the treatment, the better), but it can also be as simple as an instruction on an at-home-trial medication saying “take 20 minutes before bed”. Because, if it weren’t important, they wouldn’t bother to specify that, right? So it must be important!
And now for a quick personality test
Did you see the above as a list of dastardly tricks to watch out for, or did you see the above as a list of things that can make your actual medication more effective?
It’s arguably both, of course, but the latter more optimistic view is a lot more useful than the former more pessimistic one.
Since placebo effect works at least somewhat even when you know about it, there is nothing to stop you from leveraging it for your own benefit when taking medication or doing health-related things.
Next time you take your meds or supplements or similar, pause for a moment for each one to remember what it is and what it will be doing for you. This is a lot like the principles (which are physiological as well as psychological) of mindful eating, by the way:
How To Get More Nutrition From The Same Food
Placebo makes some surprising things evidence-based
We’ve addressed placebo effect sometimes as part of an assessment of a given alternative therapy, often in our “Mythbusting Friday” edition of 10almonds.
- In some cases, placebo is adjuvant to the therapy, i.e. it is one of multiple mechanisms of action (example: chiropractic or acupuncture)
- In some cases, placebo is the only known mechanism of action (example: homeopathy)
- In some cases, even placebo can’t help (example: ear candling)
One other fascinating and far-reaching (in a potentially good way) thing that placebo makes evidence-based is: prayer
…which is particularly interesting for something that is fundamentally faith-based, i.e. the opposite of evidence-based.
Now, we’re a health science publication, not a theological publication, so we’ll consider actual divine intervention to be beyond the scope of mechanisms of action we can examine, but there’s been a lot of research done into the extent to which prayer is beneficial as a therapy, what things it may be beneficial for, and what factors affect whether it helps:
Prayer and healing: A medical and scientific perspective on randomized controlled trials
👆 full paper here, and it is very worthwhile reading if you have time, whether or not you are religious personally
Placebo works best when there’s a clear possibility for psychosomatic effect
We’ve mentioned before, and we’ll mention again:
- psychosomatic effect does not mean: “imagining it”
- psychosomatic effect means: “your brain regulates almost everything else in your body, directly or indirectly, including your autonomic functions, and especially notably when it comes to illness, your immune responses”
So, a placebo might well heal your rash or even shrink a tumor, but it probably won’t regrow a missing limb, for instance.
And, this is important: it’s not about how credible/miraculous the outcome will be!
Rather, it is because we have existing pre-programmed internal bodily processes for healing rashes and shrinking tumors, that just need to be activated—whereas we don’t have existing pre-programmed internal bodily processes for regrowing a missing limb, so that’s not something our brain can just tell our body to do.
So for this reason, in terms of what placebo can and can’t do:
- Get rid of cancer? Yes, sometimes—because the body has a process for doing that; enjoy your remission
- Fix a broken nail? No—because the body has no process for doing that; you’ll just have to cut it and wait for it to grow again
With that in mind, what will you use the not-so-mystical powers of placebo for? What ever you go for… Enjoy, and take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Prepare for Your First Therapy Session
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Everyone (who ever has therapy, anyway) has a first therapy session. So, how to make best use of that, and get things going most effectively? Dr. Tori Olds has advice:
Things to prepare
Questions that you should consider, and prepare answers to beforehand, include:
- Why are you here? Not in any deep philosophical sense, but, what brought you to therapy?
- What would you like to focus on? Chances are, you are paying a hefty hourly rate—so having considered this will allow you to get your money’s worth.
- How will you know when you’ve met your goal? Note that this is really two questions in one, because first you need to identify your goal, and then you need to expand on it. If you woke up tomorrow and all your psychological problems were solved, how would you know? What would be different? What does it look like?
If you have a little time between now and your first session, journaling can help a lot.
Remember also that a first therapy session can also be like a mutual interview, to decide whether it’s a good match. Not every therapist is good at their job, and not every therapist will be good for you specifically. Sometimes, a therapist may be a mismatch through no fault of their own. Considering what those reasons might be can also be a good thing to think about in advance, to help find the best therapist for you in fewer tries!
For most on these ideas, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
The Gift Of Aging − by Dr. Elizabeth Eckstrom & Marcy Houle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is, as you may gather from the title, a book about getting the most out of growing older, and doing it well.
Not all of it is positive though; some of it really is about avoiding, mitigating, or coping with the negatives that tend to come with aging.
The book is full of many (38) small self-contained chapters, so it’s well-suited to reading bit-by-bit, if so inclined. Essentially, it’s a collection of essays by the two authors, arranged into categories:
- Caring for your mind
- Caring for your body
- Caring for yourself and your family
- Caring for your soul
The first two sections are mostly self-explanatory; the third is largely about estate-planning of various kinds. The fourth is highly subjective, and/but not particularly religious, by the way. It’s largely an add-on to the “caring for your mind” mental health section, but now more specifically dealing with heavy topics such as the emotional side of mortality (as opposed to the previous section’s practical considerations of same), loss, and grief.
The style is the very low end of pop-science; facts (probably true ones; nothing seemed very contentious objectively) are stated with no sources, and there is no medical jargon that’s anything more complicated than you might find on a leaflet in a doctor’s waiting room.
Bottom line: this is a very opinion-filled book, so it’s worth reading with that in mind (i.e. their opinions may differ wildly from yours in some cases), but it’s largely informed opinions, so worth at least considering even in those cases. If nothing else, this book is certainly thought-provoking.
Click here to check out The Gift Of Aging, and enjoy the gift of aging!
Share This Post
-
Blueberries vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blueberries to banana, we picked the banana.
Why?
Surprise, that which is more expensive is not always commensurately more healthy! A lot of the price difference between bananas and blueberries comes down to:
- ease of transport (unripe bananas can be transported quite easily without too much risk of bruising; unripe blueberries can’t even be usefully picked)
- shelf-life (unripe bananas will take their time to ripen; the already-ripe blueberries will often go bad very quickly)
For this reason, frozen blueberries are a great option for budget-friendly berries. But, onto the comparisons:
In terms of macros, bananas have slightly more protein, carbs, and fiber, and the slightly lower glycemic index. Really, both are good, but by the numbers, bananas win.
When it comes to vitamins, blueberries have more of vitamins B1, C, E, and K, while bananas have more of vitamins A, B2, B3, B5, B6, B9, and choline. Another win for bananas, though of course we could quibble which vitamins are most likely to be not found in sufficient abundance in the rest of one’s diet, but as it is, we just compared the nutrients head-to-head without trying to guess the rest of someone’s diet.
In the category of minerals, blueberries have more calcium and manganese, while bananas have more copper, magnesium, phosphorus, potassium, and selenium. Another win for bananas.
As for polyphenols, this is where blueberries shine, with a lot more than bananas (difficult to calculate exactly due to variations, but, in the order of hundreds of times more). A win for blueberries this time.
Adding up the section gives us an overall win for bananas, but by all means enjoy either or both; perhaps even together!
Want to learn more?
You might like to read:
Blueberry & Banana Collagen Baked Oats ← You will love this recipe! And… Good news for vegans/vegetarians: while we include an optional tablespoon of collagen powder in this recipe, the whole recipe is already geared around collagen synthesis, so it’s very collagen-boosting even with just the plants, providing collagen’s building blocks of protein, zinc, and vitamins C and D (your miraculous body will use these to assemble the collagen inside you).
Enjoy!
Share This Post
Related Posts
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Cold Truth About Respiratory Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Pathogens That Came In From The Cold
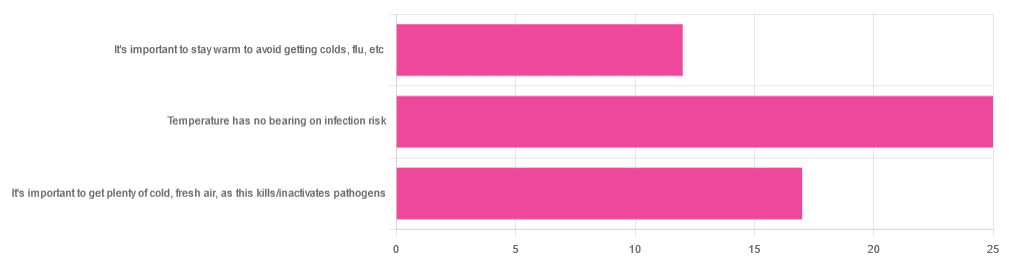
Yesterday, we asked you about your climate-themed policy for avoiding respiratory infections, and got the above-depicted, below-described, set of answers:
- About 46% of respondents said “Temperature has no bearing on infection risk”
- About 31% of respondents said “It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens”
- About 22% of respondents said “It’s important to stay warm to avoid getting colds, flu, etc”
Some gave rationales, including…
For “stay warm”:
❝Childhood lessons❞
For “get cold, fresh air”:
❝I just feel that it’s healthy to get fresh air daily. Whether it kills germs, I don’t know❞
For “temperature has no bearing”:
❝If climate issue affected respiratory infections, would people in the tropics suffer more than those in colder climates? Pollutants may affect respiratory infections, but I doubt just temperature would do so.❞
So, what does the science say?
It’s important to stay warm to avoid getting colds, flu, etc: True or False?
False, simply. Cold weather does increase the infection risk, but for reasons that a hat and scarf won’t protect you from. More on this later, but for now, let’s lay to rest the idea that bodily chilling will promote infection by cold, flu, etc.
In a small-ish but statistically significant study (n=180), it was found that…
❝There was no evidence that chilling caused any acute change in symptom scores❞
Read more: Acute cooling of the feet and the onset of common cold symptoms
Note: they do mention in their conclusion that chilling the feet “causes the onset of cold symptoms in about 10% of subjects who are chilled”, but the data does not support that conclusion, and the only clear indicator is that people who are more prone to colds generally, were more prone to getting a cold after a cold water footbath.
In other words, people who were more prone to colds remained more prone to colds, just the same.
It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens: True or False?
Broadly False, though most pathogens do have an optimal operating temperature that (for obvious reasons) is around normal human body temperature.
However, given that they don’t generally have to survive outside of a host body for long to get passed on, the fact that the pathogens may be a little sluggish in the great outdoors will not change the fact that they will be delighted by the climate in your respiratory tract as soon as you get back into the warm.
With regard to the cold air not being a reliable killer/inactivator of pathogens, we call to the witness stand…
Polar Bear Dies From Bird Flu As H5N1 Spreads Across Globe
(it was found near Utqiagvik, one of the northernmost communities in Alaska)
Because pathogens like human body temperature, raising the body temperature is a way to kill/inactivate them: True or False?
True! Unfortunately, it’s also a way to kill us. Because we, too, cannot survive for long above our normal body temperature.
So, for example, bundling up warmly and cranking up the heating won’t necessarily help, because:
- if the temperature is comfortable for you, it’s comfortable for the pathogen
- if the temperature is dangerous to the pathogen, it’s dangerous to you too
This is why the fever response evolved, and/but why many people with fevers die anyway. It’s the body’s way of playing chicken with the pathogen, challenging “guess which of us can survive this for longer!”
Temperature has no bearing on infection risk: True or False?
True and/or False, circumstantially. This one’s a little complex, but let’s break it down to the essentials.
- Temperature has no direct effect, for the reasons we outlined above
- Temperature is often related to humidity, which does have an effect
- Temperature does tend to influence human behavior (more time spent in open spaces with good ventilation vs more time spent in closed quarters with poor ventilation and/or recycled air), which has an obvious effect on transmission rates
The first one we covered, and the third one is self-evident, so let’s look at the second one:
Temperature is often related to humidity, which does have an effect
When the environmental temperature is warmer, water droplets in the air will tend to be bigger, and thus drop to the ground much more quickly.
When the environmental temperature is colder, water droplets in the air will tend to be smaller, and thus stay in the air for longer (along with any pathogens those water droplets may be carrying).
Some papers on the impact of this:
- Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections
- A Decrease in Temperature and Humidity Precedes Human Rhinovirus Infections in a Cold Climate
So whatever temperature you like to keep your environment, humidity is a protective factor against respiratory infections, and dry air is a risk factor.
So, for example:
- If the weather doesn’t suit having good ventilation, a humidifier is a good option
- Being in an airplane is one of the worst places to be for this, outside of a hospital
Don’t have a humidifier? Here’s an example product on Amazon, but by all means shop around.
A crock pot with hot water in and the lid off is also a very workable workaround too
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Death by Food Pyramid – by Denise Minger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one is less about “here’s the perfect way of eating” or even “these specific foods are ontologically evil”, but more about teaching science literacy.
The author explores various health trends from the 70s until time of writing (the book was published in 2014), what rationales originally prompted them, and what social phenomena either helped them to persist, or caused them to get dropped quite quickly.
Of course, even in the case of fads that are societally dropped quite quickly, on an individual level there will always be someone just learning about it for the first time, reading some older material, and thinking “that sounds like just the miracle life-changer I need!”
What she teaches the reader to do is largely what we do a lot of here at 10almonds—examine the claims, go to the actual source material (studies! Not just books about studies!), and see whether the study conclusions actually support the claim, to start with, and then further examine to see if there’s some way (or sometimes, a plurality of ways) in which the study itself is methodologically flawed.
Which does happen sometimes, do actually watch out for that!
The style is quite personal and entertaining for the most part, and yet even moving sometimes (the title is not hyperbole; deaths will be discussed). As one might expect of a book teaching science literacy, it’s very easy to read, with copious footnotes (well, actually they are at the back of the book doubling up as a bibliography, but they are linked-to throughout) for those who wish to delve deeper—something the author, of course, encourages.
Bottom line: if you’d like to be able to sort the real science from the hype yourself, then this book can set you on the right track!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: