Pinch of Nom – by Kate Allinson & Kay Allinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Home-style recipes”, because guess where most readers live!
And: slimming, because trimming the waistline a little is a goal for many after holiday indulgences.
The key idea here is healthy recipes that “don’t taste like diet food”—often by just switching out a couple of key ingredients, to give a significantly improved nutritional profile while remaining just as tasty, especially when flavors are enhanced with clever spicing and seasoning.
The food is simple to prepare, while being “special” enough that it could be used very credibly for entertaining too. For that matter, a strength of the book is its potential for use as a creative springboard, if you’re so inclined—there are lots of good ideas in here.
The recipes themselves are all you’d expect them to be, and presented clearly in an easy-to-follow manner.
Bottom line: if you’ve ever wanted to cook healthily but you need dinner on the table in the very near future and are stuck for ideas, this book is exactly what you need.
Click here to check out Pinch of Nom, and liven up your healthy cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s Missing from Medicine – by Dr. Saray Stancic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”, Dr. Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the treatments presented.
Taking an evidence-based lifestyle medicine approach, she was able to not only manage her illness sufficiently to resume her normal activities, but even when so far as to run a marathon, and today boasts a symptom-free, active life.
The subtitular six lifestyle changes are not too shocking, and include a plants-centric diet, good exercise, good sleep, stress management, avoidance of substance abuses, and a fostering of social connections, but the value here is in what she has to say about each, especially the ones that aren’t so self-explanatory and/or can even cause harm if done incorrectly (such as exercise, for example).
The style is on the academic end of pop-science, of the kind that has frequent data tables, lots of statistics, and an extensive bibliography, but is still very readable.
Bottom line: if you are faced with a chronic disease, or even just an increased risk of some chronic disease, or simply like to not take chances, then this is a high-value book for you.
Click here to check out What’s Missing From Medicine, and enjoy chronic good health!
Share This Post
-
Unlimited Memory – by Kevin Horsley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Premise: there are easily learnable techniques to rapidly (and greatly) improve one’s memory. We’ve touched on some of these methods before at 10almonds, but being a newsletter rather than a book, we’ve not been able to go as deeply into it as Horsley!
Your memory is far, far, far more powerful than you might realize, and this book will help unlock that. To illustrate…
Some of the book is given over to what are for most purposes “party tricks”, such as remembering pi to 10,000 places. Those things are fun, even if not as practical in today’s world of rarely needing to even know the actual digits of a phone number. However, they do also serve as a good example of just how much of “super memory” isn’t a matter of hard work, so much as being better organized about it.
Most of the book is focused on practical methods to improve the useful aspects of memory—including common mistakes!
If the book has any flaw it’s that the first chapter or so is spent persuading the reader of things we presumably already believe, given that we bought the book. For example, that remembering things is a learnable skill and that memory is functionally limitless. However, we still advise to not skip those chapters as they do contain some useful reframes as well.
Bottom line: if you read this book you will be astonished by how much you just learned—because you’ll be able to recall whole sections in detail! And then you can go apply that whatever areas of your life you wanted to when you bought the book.
Share This Post
-
Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
Stop Checking Your Likes – by Susie Moore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You might think this one’s advice is summed up sufficiently by the title, that there’s no need for a book! But…
There’s a lot more to this than “stop comparing the worst out-takes of your life to someone else’s highlight reel”, and there’s a lot more to this than “just unplug”.
Instead, Susie Moore discusses the serious underlying real emotional considerations of the need for approval (and even just acceptance) by our community, as well the fear of missing out.
It’s not just about how social media is designed to hijack various parts of our brain, or how The Alogorithm™ is out to personally drag your soul through Hell for a few more clicks; it’s also about the human element that would exist even without that. Who remembers MySpace? No algorithm in those days, but oh the drama potential for those “top 8 friends” places. And if you think that kind of problem is just for young people 20 years ago, you have mercifully missed the drama that older generations can get into on Facebook.
Along with the litany of evil, though, Moore also gives practical advice on how to overcome those things, how to “see the world through comedy-colored glasses”, how to ask “what’s missing, really?”, and how to make your social media experience work for you, rather than it merely using you as fuel. ← link is to our own related article!
Bottom line: if social media sucks a lot of your time, there may be more to it than just “social media sucks in general”, and there are ways to meet your emotional needs without playing by corporations’ rules to do so.
Click here to check out Stop Checking Your Likes, and breathe easy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Parenting a perfectionist? Here’s how you can respond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some children show signs of perfectionism from early on. Young children might become frustrated and rip up their drawing if it’s not quite right. Older children might avoid or refuse to do homework because they’re afraid to make a mistake.
Perfectionism can lead to children feeling overwhelmed, angry and frustrated, or sad and withdrawn.
And yet perfectionism isn’t considered all bad in our society. Being called a “perfectionist” can be a compliment – code for being a great worker or student, someone who strives to do their best and makes sure all jobs are done well.
These seemingly polarised views reflect the complex nature of perfectionism.
Annie Spratt/Unsplash What is perfectionism?
Researchers often separate perfectionism into two parts:
- perfectionistic strivings: being determined to meet goals and achieve highly
- perfectionistic concerns: worry about being able to meet high standards, and self-criticism about performance.
While perfectionistic strivings can be positive and lead to high achievement, perfectionistic concerns can lead to a higher chance of children developing eating disorders or anxiety and depression, and having lower academic achievement.
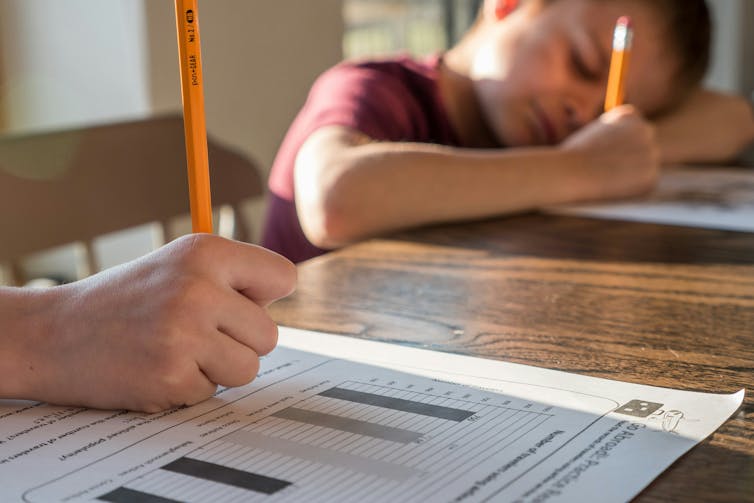
Perfectionistic concerns can result in lower academic achievement. Jessica Lewis/Unsplash Children and adolescents may experience perfectionism in relation to school work, sport, performance in art or music, or in relation to their own body.
Signs of perfectionistic concerns in children and adolescents may include:
- children being highly critical of themselves
- their reactions to mistakes seeming to be an overreaction
- intense preoccupation and worry over their standards and goals and/or procrastination
- significant change in performance, for example, lower academic results
- irritability and negative emotions, stress and feelings of worthlessness
- social problems with peers and friends, such as bullying and alienating themselves from peers.
A range of genetic, biological and environmental factors influence perfectionism in children. And as a parent, our role is important. While research evidence suggests we can’t successfully increase positive perfectionistic strivings in our children, harsh or controlling parenting can increase negative perfectionistic concerns in children.
Parents who are perfectionistic themselves can also model this to their children.
So, how can we walk the line between supporting our child’s interests and helping them to achieve their potential, without pressuring them and increasing the risk of negative outcomes?
Give them space to grow
A great metaphor is the gardener versus the carpenter described by psychology professor Alison Gopnik.
Instead of trying to build and shape our children by controlling them and their environment (like a carpenter), parents can embrace the spirit of the gardener – providing lots of space for children to grow in their own direction, and nourishing them with love, respect and trust.
Parents don’t need to control their child and their environment. Noah Silliman/Unsplash We can’t control who they become, so it’s better to sit back, enjoy the ride, and look forward to watching the person they grow into.
However, there is still plenty we can do as parents if our child is showing signs of perfectionism. We can role model to our children how to set realistic goals and be flexible when things change or go wrong, help our children manage stress and negative emotions, and create healthy balance in our family daily routine.
Set realistic goals
People with perfectionistic tendencies will often set unattainable goals. We can support the development of flexibility and realistic goal setting by asking curious questions, for example, “what would you need to do to get one small step closer to this goal?” Identifying upper and lower limits for goals is also helpful.
If your child is fixed on a high score at school, for example, set that as the “upper limit” and then support them to identify a “lower limit” they would find acceptable, even if they are less happy with the outcome.
This strategy may take time and practice to widen the gap between the two, but is useful to create flexibility over time.
If a goal is performance-based and the outcome cannot be guaranteed (for example, a sporting competition), encourage your child to set a personal goal they have more control over.
Parents can help children set goals they can achieve. liz99/Unsplash We can also have conversations about perfectionism from early on, and explain that everyone makes mistakes. In fact, it’s great to model this to our children – talking about our own mistakes and feelings, to show them that we ourselves are not perfect.
Talk aloud practices can help children to see that we “walk the walk”. For example, if you burn dinner you could reflect:
I’m disappointed because I put time and effort into that and it didn’t turn out as I expected. But we all make mistakes. I don’t get things right every time.
Manage stress and negative emotions
Some children and adolescents have a natural tendency towards perfectionism. Rather than trying to control their behaviour, we can provide gentle, loving support.
When our child or adolescent becomes frustrated, angry, sad or overwhelmed, we support them best by helping them to name, express and validate all of their emotions.
Parents may fear that acknowledging their child’s negative emotions will make the emotions worse, but the opposite is true.
Creating healthy balance
The building blocks of healthy child development are strong loving family relationships, good nutrition, creative play and plenty of physical activity, sleep and rest.
Perfectionism is associated with rigidity, and thinking that there is only one correct way to succeed. We can instead encourage flexibility and creativity in children.
Children’s brains grow through play. There is strong research evidence showing that creative, child-led play is associated with higher emotion regulation skills, and a range of cognitive skills, including problem-solving, memory, planning, flexibility and decision-making.
Play helps children’s brains grow. Mi Pham/Unsplash Play isn’t just for young children either – there’s evidence that explorative, creative play of any kind also benefits adolescents and adults.
There is also evidence that getting active outdoors in nature can promote children’s coping skills, emotion regulation and cognitive development.
Elizabeth Westrupp, Associate Professor in Psychology, Deakin University; Gabriella King, Associate Research Fellow, Deakin University, and Jade Sheen, Associate Professor, School of Psychology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Lupus Solution – by Dr. Tiffany Caplan & Dr. Brent Caplan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lupus is not fun, and this book sets out to make it easier.
Starting off by explaining the basics of autoimmunity and how lupus works, the authors go on the address the triggers of lupus and how to avoid them—which if you’ve been suffering from lupus for a while, you probably know this part already, but it’s as well to give them a look over just in case you missed something.
The real value of the book though comes in the 8 chapters of the section “Tools & Therapies” which are mostly lifestyle adjustments though there are additionally some pharmaceutical approaches that can also help, and they are explained too. And no, it’s not just “reduce inflammation” (but yes, also that); rather, a whole array of things are examined that often aren’t thought of as related to lupus, but in fact can have a big impact.
The style is to-the-point and informational, and formatted for ease of reading. It doesn’t convey more hard science than necessary, but it does have a fair bibliography at the back.
It’s a short book, weighing in at 182 pages. If you want something more comprehensive, check out our review of The Lupus Encyclopedia, which is 848 pages of information-dense text and diagrams.
Bottom line: if you have lupus and would like fewer symptoms, this book can help you with that quite a bit without getting so technical as the aforementioned encyclopedia.
Click here to check out The Lupus Solution, and live more comfortably!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: