Peace Is Every Step – by Thích Nhất Hạnh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mindfulness is one of the few practices to make its way from religion (in this case, Buddhism) into hard science. We’ve written before about its many evidence-based benefits, and many national health information outlets recommend it. So, what does this book have to add?
Thích Nhất Hạnh spent most of his 95 years devoted to the practice and teaching of mindfulness and compassion. In this book, the focus is on bringing mindfulness off the meditation mat and into general life.
After all, what if we could extend that “unflappability” into situations that pressure and antagonize us? That would be some superpower!
The author offers techniques to do just that, simple exercises to transform negative emotions, and to make us more likely to remember to do so.
After all, “in the heat of the moment” is rarely when many of us are at our best, this book gives way to allow those moments themselves to serve as immediate triggers to be our best.
The title “Peace Is Every Step” is not a random collection of words; the goal of this book is to enable to reader to indeed carry peace with us as we go.
Not just “peace is always available to us”, but if we do it right: “we have now arranged for our own peace to automatically step in and help us when we need it most”.
Bottom line: if you’d like to practice mindfulness, or practice it more consistently, this book offers some powerful tools.
Click here to check out Peace Is Every Step, and carry yours with you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
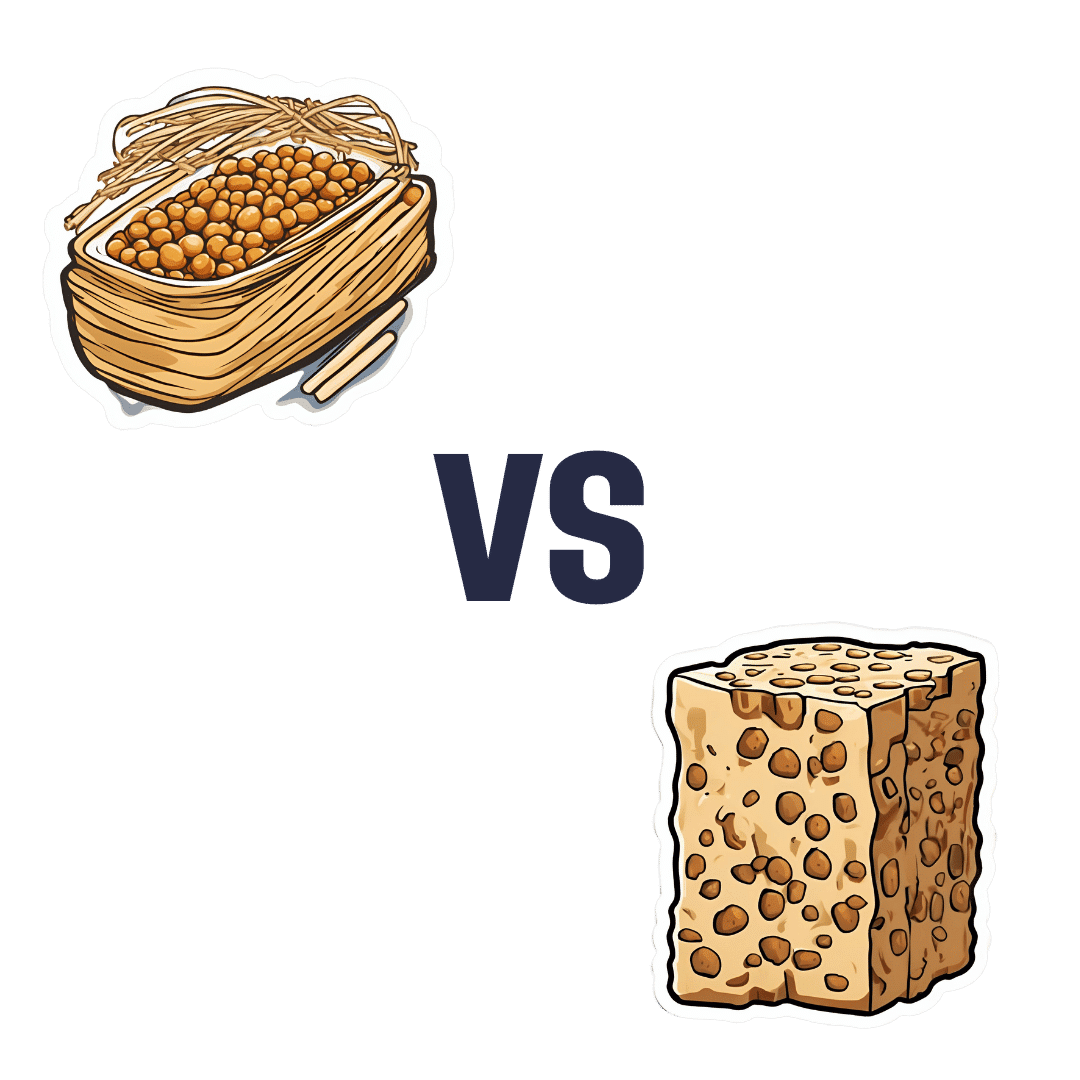
Natto vs Tempeh – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nattō to tempeh, we picked the nattō.
Why?
Both are great, but in the battle of fermented soybeans vs fermented soybeans with extra steps, it turns out that the simplest option is the best, even if tempeh was a close runner-up:
In terms of macros, nattō has more carbs and fiber for the same protein and fat; we’ll call this category a tie or a marginal win for nattō.
In the category of vitamins, nattō has more of vitamins B1, C, E, K, and choline, while tempeh has more of vitamins B2, B3, B6, and B9. A clearer, yet still modest, win for nattō.
Minerals, however, are what really set them apart: nattō has more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc, while tempeh has more phosphorus. An overwhelming win for nattō this time.
In short: enjoy either or both, but nattō is the more nutritionally dense option!
Want to learn more?
You might like:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nattō is featured as part of the diet 😎
Enjoy!
Share This Post
-
Don’t Do *This* If You’re Over 50 (And Want Better Sleep)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, sleep specialist, explains:
Don’t make these mistakes
Dr. Breus recommends avoiding…
- Misusing magnesium: magnesium is a helpful sleep aid but must be carefully monitored. Recommended doses are 250mg for women and 300–350 mg for men, with slight adjustments for hot climates or active lifestyles. Overdosing can cause stomach issues, diarrhea, and dehydration, disrupting sleep. He recommends starting with magnesium glycinate for fewer stomach issues, and later mix with magnesium citrate. Always check supplements to avoid excessive magnesium intake.
- Misusing melatonin: melatonin production declines after age 55–60, making low-dose supplementation (0.5–1 mg) beneficial. He recommends, however, avoiding high doses (3–10mg), and he recommends to take it 90 minutes before bedtime. Melatonin interacts with some medications (including some meds for blood pressure or depression), so consult a pharmacist before use to avoid risks like serotonin syndrome.
- Going to bed too early: going to bed too early disrupts circadian rhythms and reduces sleep drive, causing earlier waking. Now, being an “early bird” is a generally healthy thing, but if you’re already getting up at 5am, say, you probably want your schedule to not continue to creep further forwards until you become nocturnal. Set a consistent wake-up time and count 7.5 hours backward (plus a set time to fall asleep, e.g. 20 minutes, but you’ll know what it is for you) to determine bedtime.
- Excessive caffeine consumption: from the heading, it may seem like a no-brainer, but older adults metabolize caffeine 33% slower on average, prolonging its effects. Dr. Breus recommends to reduce intake with “caffeine fading,” switching to half-caffeinated coffee for a while and then considering transitioning to decaf. He also suggests enjoying increasingly lower-caffeine teas, like black tea in the morning, matcha in the afternoon, and herbal tea at night to reduce caffeine’s impact on sleep.
- Falling foul of serotonin: avoid taking 5-HTP supplements with SSRI antidepressants like Prozac or Zoloft due to the risk of serotonin syndrome.
- Consider checking for physical problems: if you regularly wake up tired and/or groggy (despite having ostensibly had enough sleep, and there not being a pharmaceutical explanation for your grogginess), consider screening for sleep apnea. Home sleep tests are a convenient way to identify and treat this common but often undiagnosed condition.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How to Fall Asleep Faster: CBT-Insomnia Treatment
Take care!
Share This Post
-
Tight Hamstrings? Here’s A Test To Know If It’s Actually Your Sciatic Nerve
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tight hamstrings are often not actually due to hamstring issues, but rather, are often being limited by the sciatic nerve. This video offers a home test to determine if the sciatic nerve is causing mobility problems (and how to improve it, if so):
The Connection
Try this test:
- Sit down with a slumped posture.
- Extend one leg with the ankle flexed.
- Note any stretching or pulling sensation behind the knee or in the calf.
- Bring your head down to your chest
If this increases the sensation, it likely indicates sciatic nerve involvement.
If only the hamstrings are tight, head movement won’t change the stretch sensation.
This is because the nervous system is a continuous structure, so head movement can affect nerve tension throughout the body. While this can cause problems, it can also be integral in the solution. Here are two ways:
- Flossing method: sit with “poor” slumped posture, extend the knee, keep the ankle flexed, and lift the head to relieve nerve tension. This movement helps the sciatic nerve slide without stretching it.
- Even easier method: lie on your back, grab behind the knee, and extend the leg while extending the neck. This position avoids compression in the gluteal area, making it suitable for severely compromised nerves. Perform the movement without significant stretching or pain.
In both cases: move gently to avoid straining the nerve, which can worsen muscle tension. Do 10 repetitions per leg, multiple times a day; after a week, increase to 20 reps.
A word of caution: speak with your doctor before trying these exercises if you have underlying neurological diseases, cut or infected nerves, or other severe conditions.
For more on all of this, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Exercises for Sciatica Pain Relief
Take care!
Share This Post
Related Posts
-
The Aesthetic Brain – by Dr. Anjan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Anjan Chatterjee (not to be mistaken for Dr. Rangan Chatterjee, whose books we have also sometimes reviewed before) is a neurologist.
A lot about aesthetics is easy enough to understand. We like physical features in humans that suggest a healthy mate, and we like lush and/or colorful plants that reassure us that we will have plenty to eat.
But what about a beautiful building, or a charcoal drawing of some captivatingly eldritch horror? And what, neurologically speaking, is the difference between a bowl of fruit and a painting of a bowl of fruit? And what, if anything, does appreciation of such do for us?
In this very readable pop-science book, we learn about these things and many more, from the perspective of an experienced neurologist who explains things simply but with plenty of science.
Bottom line: if you’d like to understand how and why your brain does more things than just process tasks necessary for survival, this book will give you plenty of insight.
Click here to check out The Aesthetic Brain, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Just One Thing – by Dr. Michael Mosley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a collection of easy-to-implement changes that have good science behind them to show how they can benefit us. Some things are obvious (e.g: drink water); others, less so (e.g: sing, to reduce inflammation).
The book is divided thematically into times of the day, though in many cases it’s not a hard rule that a thing needs to be done at a certain time. Others are, like a cold shower in the morning and hot bath before bed—you might not want to switch those around!
The style is very pop-science, and does not have in-line citations for claims, but it does have a bibliography in the bag organized by each “one thing”, e.g. it might say “get some houseplants” and then list a number of references supporting that, with links to the studies showing how that helps. For those with the paper version, don’t worry, you can copy the URL from the book into your browser and see it that way. In any case, there are 2–6 scientific references for each claim, which is very respectable for a pop-sci book.
Bottom line: if you’re looking for evidence-based “one little thing” changes that can make a big difference, this book has lots!
Click here to check out Just One Thing, and improve your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Good Skin Solution – by Shann Jones
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not everyone knows that eczema is not just a skin condition; it’s an autoimmune condition. And thus to heal one’s skin, the gut is a good place to start.
This is not your average gut health book though, because it is focused on optimizing things for one’s skin… Although the author herself learned about this while helping her husband to battle an MRSA infection. In other words, a multi-fronted battle for sure.
The advices in this book are good for, as the subtitle promises, an assortment of other skin conditions too, including psoriasis, rosacea, and acne. She covers the usual bases, and recommends probiotics, of which she’s particularly keen to praise kefir, while advising against the use of antibiotics unless absolutely necessary—something we’ve talked about from time to time at 10almonds, too.
Not content to merely cover those things, she also talks allergies, and walking the fine line between avoiding triggers and developing hypersensitivity by treating to live in a perfectly clean bubble.
Ultimately, she offers “7 daily habits”, 3 of which involve goat’s milk kefir, that’s how keen on it she is. So if you’re vegan, probably this book isn’t as good value, however much it discusses the health woes that can be caused and/or exacerbated by drinking cow’s milk.
The style is very light and personable, which makes for easy reading, more like one friend talking to another, than a scientific textbook.
Bottom line: if you’d like healthier skin, are interested in dietary tweaks and homemade soaps, and have no aversion to goat’s milk and/or kefir, then this book is full of fascinating pointers.
Click here to check out The Good Skin Solution, and who knows, maybe you’ll find it’s the G.O.A.T!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: