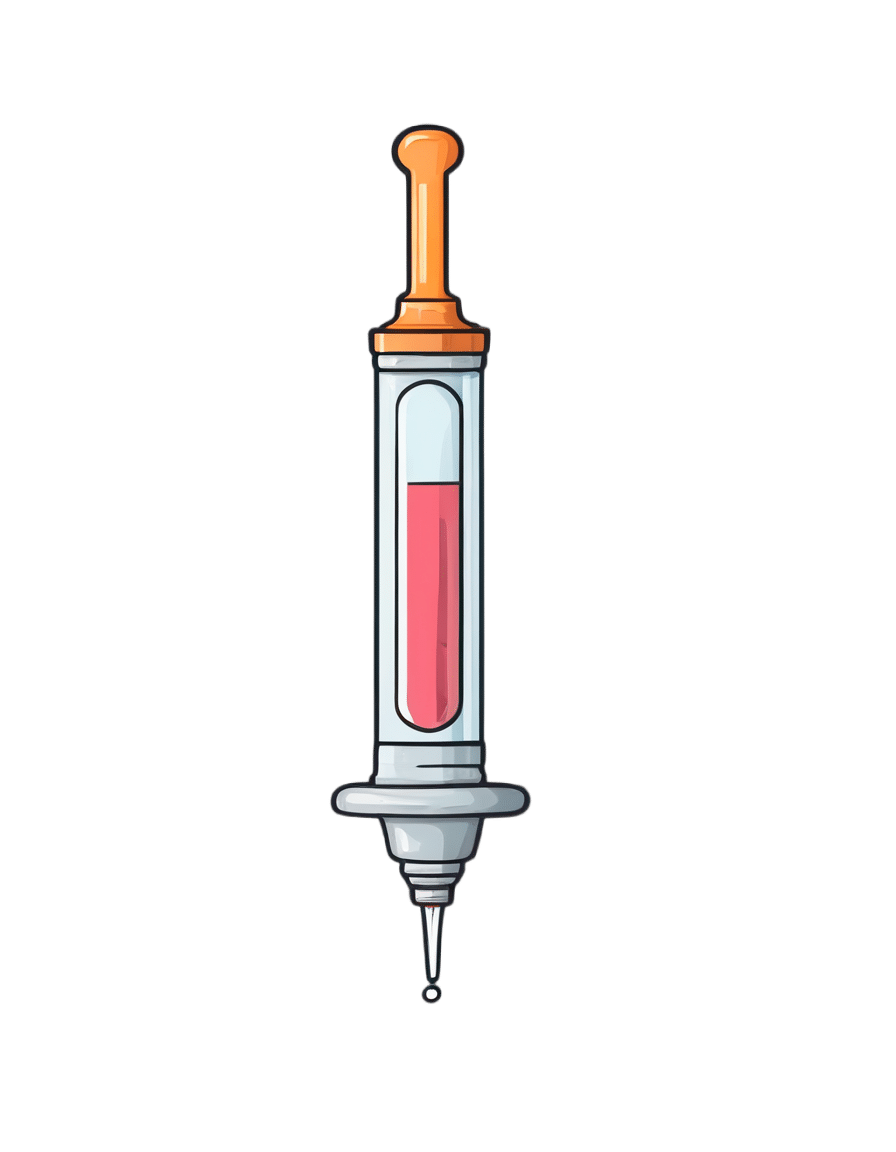
Oral vaccines could provide relief for people who suffer regular UTIs. Here’s how they work
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a recent TikTok video, Australian media personality Abbie Chatfield shared she was starting a vaccine to protect against urinary tract infections (UTIs).
Huge news for the UTI girlies. I am starting a UTI vaccine tonight for the first time.
Chatfield suffers from recurrent UTIs and has turned to the Uromune vaccine, an emerging option for those seeking relief beyond antibiotics.
But Uromune is not a traditional vaccine injected to your arm. So what is it and how does it work?

First, what are UTIs?
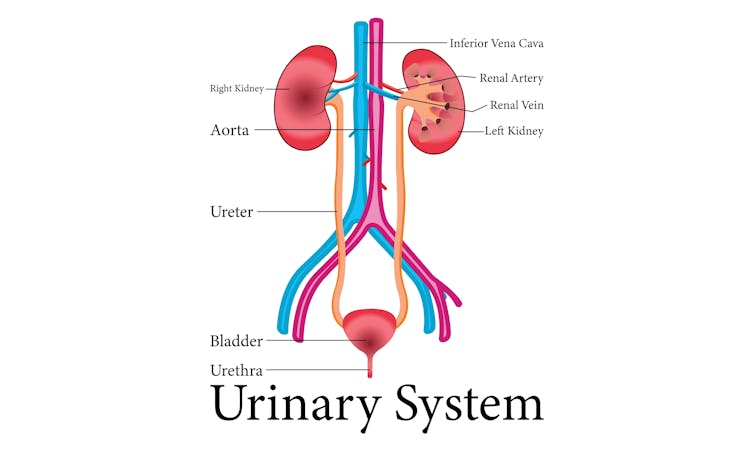
UTIs are caused by bacteria entering the urinary system. This system includes the kidneys, bladder, ureters (thin tubes connecting the kidneys to the bladder), and the urethra (the tube through which urine leaves the body).
The most common culprit is Escherichia coli (E. coli), a type of bacteria normally found in the intestines.
While most types of E. coli are harmless in the gut, it can cause infection if it enters the urinary tract. UTIs are particularly prevalent in women due to their shorter urethras, which make it easier for bacteria to reach the bladder.
Roughly 50% of women will experience at least one UTI in their lifetime, and up to half of those will have a recurrence within six months.
The symptoms of a UTI typically include a burning sensation when you wee, frequent urges to go even when the bladder is empty, cloudy or strong-smelling urine, and pain or discomfort in the lower abdomen or back. If left untreated, a UTI can escalate into a kidney infection, which can require more intensive treatment.
While antibiotics are the go-to treatment for UTIs, the rise of antibiotic resistance and the fact many people experience frequent reinfections has sparked more interest in preventive options, including vaccines.
What is Uromune?
Uromune is a bit different to traditional vaccines that are injected into the muscle. It’s a sublingual spray, which means you spray it under your tongue. Uromune is generally used daily for three months.
It contains inactivated forms of four bacteria that are responsible for most UTIs, including E. coli. By introducing these bacteria in a controlled way, it helps your immune system learn to recognise and fight them off before they cause an infection. It can be classified as an immunotherapy.
A recent study involving 1,104 women found the Uromune vaccine was 91.7% effective at reducing recurrent UTIs after three months, with effectiveness dropping to 57.6% after 12 months.
These results suggest Uromune could provide significant (though time-limited) relief for women dealing with frequent UTIs, however peer-reviewed research remains limited.
Any side effects of Uromune are usually mild and may include dry mouth, slight stomach discomfort, and nausea. These side effects typically go away on their own and very few people stop treatment because of them. In rare cases, some people may experience an allergic reaction.
How can I access it?
In Australia, Uromune has not received full approval from the Therapeutic Goods Administration (TGA), and so it’s not something you can just go and pick up from the pharmacy.
However, Uromune can be accessed via the TGA’s Special Access Scheme or the Authorised Prescriber pathway. This means a GP or specialist can apply for approval to prescribe Uromune for patients with recurrent UTIs. Once the patient has a form from their doctor documenting this approval, they can order the vaccine directly from the manufacturer.

Uromune is not covered under the Pharmaceutical Benefits Scheme, meaning patients must cover the full cost out-of-pocket. The cost of a treatment program is around A$320.
Uromune is similarly available through special access programs in places like the United Kingdom and Europe.
Other options in the pipeline
In addition to Uromune, scientists are exploring other promising UTI vaccines.
Uro-Vaxom is an established immunomodulator, a substance that helps regulate or modify the immune system’s response to bacteria. It’s derived from E. coli proteins and has shown success in reducing UTI recurrences in several studies. Uro-Vaxom is typically prescribed as a daily oral capsule taken for 90 days.
FimCH, another vaccine in development, targets something called the adhesin protein that helps E. coli attach to urinary tract cells. FimCH is typically administered through an injection and early clinical trials have shown promising results.
Meanwhile, StroVac, which is already approved in Germany, contains inactivated strains of bacteria such as E. coli and provides protection for up to 12 months, requiring a booster dose after that. This injection works by stimulating the immune system in the bladder, offering temporary protection against recurrent infections.
These vaccines show promise, but challenges like achieving long-term immunity remain. Research is ongoing to improve these options.
No magic bullet, but there’s reason for optimism
While vaccines such as Uromune may not be an accessible or perfect solution for everyone, they offer real hope for people tired of recurring UTIs and endless rounds of antibiotics.
Although the road to long-term relief might still be a bit bumpy, it’s exciting to see innovative treatments like these giving people more options to take control of their health.
Iris Lim, Assistant Professor in Biomedical Science, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Seven Principles for Making Marriage Work – by Dr. John Gottman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of relationship advice can seem a little wishy-washy. Hardline clinical work, on the other hand, can seem removed from the complex reality of married life. Dr. Gottman, meanwhile, strikes a perfect balance.
He looks at huge datasets, and he listens to very many couples. He famously isolated four relational factors that predict divorce with 91% accuracy, his “Four Horsemen”:
- Criticism
- Contempt
- Defensiveness
- Stonewalling
He also, as the title of this book promises (and we get a chapter-by-chapter deep-dive on each of them) looks at “Seven principles for making marriage work”. They’re not one-word items, so including them here would take up the rest of our space, and this is a book review not a book summary. However…
Dr. Gottman’s seven principles are, much like his more famous “four horsemen”, deeply rooted in science, while also firmly grounded in the reality of individual couples. Essentially, by listening to very many couples talk about their relationships, and seeing how things panned out with each of them in the long-term, he was able to see what things kept on coming up each time in the couples that worked out. What did they do differently?
And, that’s the real meat of the book. Science yes, but lots of real-world case studies and examples, from couples that worked and couples that didn’t.
In so doing, he provides a roadmap for couples who are serious about making their marriage the best it can be.
Bottom line: this is a must-have book for couples in general, no matter how good or bad the relationship.
- For some it’ll be a matter of realising “You know what; this isn’t going to work”
- For others, it’ll be a matter of “Ah, relief, this is how we can resolve that!”
- For still yet others, it’ll be a matter of “We’re doing these things right; let’s keep them forefront in our minds and never get complacent!”
- And for everyone who is in a relationship or thinking of getting into one, it’s a top-tier manual.
Share This Post
-
Heart Attack: His & Hers (Be Prepared!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Heart attack symptoms vary by sex. This is governed by hormones, so if you are for example a postmenopausal woman and not on HRT, your symptoms might be nearer that of men.
The following symptom list is intended as a rough “most likely” guide. You may not get all of the symptoms you “should”. You could get symptoms from the “wrong” category. So don’t sweat the minutiae, but do be aware of…
Symptoms for everyone:
- Jaw, neck, and/or back pain
- Nausea and/or vomiting
- Shortness of breath
- Feeling of impending doom ← heart attack survivors assure us that you’ll know this one if you experience it
Additional symptoms (mostly) just for men:
- Pressure and/or pain in the upper chest
- Discomfort and/or tingling in the arms
- Sudden cold sweat
Additional symptoms (mostly) just for women:
- Pressure and/or pain in the lower chest and/or abdomen
- Feeling of fullness and/or indigestion
- Fatigue, dizziness, possibly fainting
In the event of experiencing symptoms…
Call 911 or your local equivalent.This is not the time to wait to see if it goes away by itself. If unsure, call. Better safe than sorry/dead.
If you are not alone, or if it is someone with you who is having the suspected heart attack, it may be quicker to go to the Emergency Room by car, than wait for an ambulance.
Even if you choose to do that, you should still call 911 anyway, as the responder will be able to instruct you in real-time, not something we can do in a newsletter.
Note that if available, this means three people in the car is ideal:
Driver, patient, and third person on the phone giving information and following instructions.
Emergency situations rarely go entirely by-the-book, but with a little foreknowledge and at least one person with a calm head, preventable deaths can be avoided.
Share This Post
-
Reasons to Stay Alive – by Matt Haig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Matt Haig’s (excellent) The Comfort Book, and now it’s time for his more famous book: Reasons To Stay Alive. So, what’s this one, beyond the obvious?
It narrates the experience of anxiety, depression, and suicidality, and discovering how to find beauty and joy in the world despite it all. It’s not that the author found a magical cure—he still experiences depression and anxiety (cannot speak for suicidality) but he knows now how to manage it, and live his life.
You may be wondering: is this book instructional; is it reproducible, or is it just an autobiography? It’s centered around his own experience and learnings, but it gives a huge sense of not feeling alone, of having hope, and it gives a template for making sense of one’s own experience, even if every person will of course have some points of differences, the commonalities are nonetheless of immense value.
The writing style is similar to The Comfort Book; it’s lots of small chapters, and all very easy-reading. Well, the subject matter is sometimes rather heavy, but the language is easy-reading! In other words, just the thing for when one is feeling easily overwhelmed, or not feeling up to reading a lot.
Bottom line: whether or not you suffer with anxiety and/or depression, whether or not you sometimes feel suicidal, the contents of this book are important, valuable insights for everyone.
Click here to check out Reasons To Stay Alive, and see through the highs and lows of life.
Share This Post
Related Posts
-
The Ultimate Booster
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Winning The Biological Arms Race
The human immune system (and indeed, other immune systems, but we are all humans here, after all) is in a constant state of war with pathogens, and that war is a constant biological arms race:
- We improve our defenses and destroy the attackers; the 1% of pathogens that survived now “know” how to counter that trick.
- The pathogens wreak havoc in our systems; the n% of us that survive now have immune systems that “know” how to counter that trick.
Vaccines are a mighty tool in our favor here, because they’re the technology that stops our n% from also being a very low number.
With vaccines, we can effectively pass on established defenses onto the population at large, as this cute video explains very well and very simply in 57 seconds:
Click Here If The Embedded Video Doesn’t Load Automatically!
The problem with vaccines
The problem is that this accelerates the arms race. It’s like a chess game where we are able to respond to every move quickly (which is good for us), and/but this means passing the move over to our opponent sooner.
That problem’s hard to avoid, because the alternative has always been “let people die in much larger numbers”.
Traditional vs mRNA vaccines
A quick refresher before we continue to the big news of the day:
- Traditional vaccines use a disabled version of a pathogen to trigger an immune response that will teach the body to recognize the pathogen ready for when the full version shows up
- mRNA vaccines use a custom-made bit of genetic information to tell the body to make its own harmless fake pathogen and then respond to the harmless fake pathogen it made.
Note: this happens independently of the host’s DNA, so no, it does not change your DNA
See also: The Truth About Vaccines
Here’s a more detailed explainer (with a helpful diagram) using the COVID mRNA vaccine as an example:
Genome.gov | How does an mRNA vaccine work?
However, this still leaves us “chasing strains”, because as the pathogen (in this case, a virus) adapts, the vaccine has to be updated too, hence all the boosters.
This is a lot like a security update for your computer’s antivirus software. They’re annoying, but they do an important job.
No more “chasing strains”
The press conference soundbite on this sums it up well:
❝Scientists at UC Riverside have demonstrated a new, RNA-based vaccine strategy that is effective against any strain of a virus and can be used safely even by babies or the immunocompromised.❞
Read in full: Vaccine breakthrough means no more chasing strains
You may be wondering: what makes this one effective against any strain?
❝What I want to emphasize about this vaccine strategy is that it is broad.
It is broadly applicable to any number of viruses, broadly effective against any variant of a virus, and safe for a broad spectrum of people. This could be the universal vaccine that we have been looking for.
Viruses may mutate in regions not targeted by traditional vaccines. However, we are targeting their whole genome with thousands of small RNAs. They cannot escape this.❞
Importantly, this means it can be applied not just to one disease, let alone just one strain of COVID. Rather, it can be used for a wide variety of viruses that have similar viral functions—COVID / SARS in general, including influenza, and even viruses such as dengue.
How it does this: the above article explains in more detail, but in few words: it targets tiny strings of the genome that are present in all strains of the virus.
Illustrative example: if you wanted to block 10almonds (please don’t), you could block our email address.
But if we were malicious (we’re not) we could be sneaky and change it, so you’d have to block the new one, and the cycle repeats.
But if you were block all emails containing the tiny string of characters “10almonds”, changing our email address would no longer penetrate your defenses.
Now imagine also blocking strings such as “One-Minute Book Review” and “Today’s almonds have been activated by” and other strings we use in every email.
Now multiply this by thousands of strings (because genomes are much larger than our little newsletter), and you see its effectiveness!
Great! How can I get this?
It’s still in the testing stages for now; this is “breaking news” science, after all.
The study itself
…is paywalled for now, sadly, but if you happen to have institutional access, here it is:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From immunotherapy to mRNA vaccines – the latest science on melanoma treatment explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More than 16,000 Australians will be diagnosed with melanoma each year. Most of these will be caught early, and can be cured by surgery.
However, for patients with advanced or metastatic melanoma, which has spread from the skin to other organs, the outlook was bleak until the advent of targeted therapies (that attack specific cancer traits) and immune therapies (that leverage the immune system). Over the past decade, these treatments have seen a significant climb in the number of advanced melanoma patients surviving for at least five years after diagnosis, from less than 10% in 2011 to around 50% in 2021.
While this is great news, there are still many melanoma patients who cannot be treated effectively with current therapies. Researchers have developed two exciting new therapies that are being evaluated in clinical trials for advanced melanoma patients. Both involve the use of immunotherapy at different times and in different ways.
The first results from these trials are now being shared publicly, offering insight into the future of melanoma treatment.
Svitlana Hulko/Shutterstock Immunotherapy before surgery
Immunotherapy works by boosting the power of a patient’s immune system to help kill cancer cells. One type of immunotherapy uses something called “immune checkpoint inhibitors”.
Immune cells carry “immune checkpoint” proteins, which control their activity. Cancer cells can interact with these checkpoints to turn off immune cells and hide from the immune system. Immune checkpoint inhibitors block this interaction and help keep the immune system activated to fight the cancer.
Results from an ongoing phase 3 trial using immune checkpoint inhibitors were recently published in the New England Journal of Medicine.
This trial used two types of immune checkpoint inhibitors: nivolumab, which blocks an immune checkpoint called PD-1, and ipilimumab, which blocks CTLA-4.
More than 16,000 Australians are diagnosed with melanoma each year. Delovely Pics/Shutterstock Some 423 patients (including many from Australia) were enrolled in the trial, and participants were randomly assigned to one of two groups.
The first group had surgery to remove their melanoma, and were then given immunotherapy (nivolumab) to help kill any remaining cancer cells. Giving a systemic (whole body) therapy such as immunotherapy after surgery is a standard way of treating melanoma. The second group received immunotherapy first (nivolumab plus ipilimumab) and then underwent surgery. This is a new approach to treating these cancers.
Based on previous observations, the researchers had predicted that giving patients immunotherapy while the whole tumour was still present would activate the tumour-fighting abilities of the patient’s immune system much better than giving it once the tumour had been removed.
Sure enough, 12 months after starting therapy, 83.7% of patients who received immunotherapy before surgery remained cancer-free, compared to 57.2% in the control group who received immunotherapy after surgery.
Based on these results, Australian of the year Georgina Long – who co-led the trial with Christian Blank from The Netherlands Cancer Institute – has suggested this method of immunotherapy before surgery should be considered a new standard of treatment for higher risk stage 3 melanoma. She also said a similar strategy should be evaluated for other cancers.
The promising results of this phase 3 trial suggest we might see this combination treatment being used in Australian hospitals within the next few years.
mRNA vaccines
Another emerging form of melanoma therapy is the post-surgery combination of a different checkpoint inhibitor (pembrolizumab, which blocks PD-1), with a messenger RNA vaccine (mRNA-4157).
While checkpoint inhibitors like pembrolizumab have been around for more than a decade, mRNA vaccines like mRNA-4157 are a newer phenomenon. You might be familiar with mRNA vaccines though, as the biotechnology companies Pfizer-BioNTech and Moderna released COVID vaccines based on mRNA technology.
mRNA-4157 works basically the same way – the mRNA is injected into the patient and produces antigens, which are small proteins that train the body’s immune system to attack a disease (in this case, cancer, and for COVID, the virus).
However, mRNA-4157 is unique – literally. It’s a type of personalised medicine, where the mRNA is created specifically to match a patient’s cancer. First, the patient’s tumour is genetically sequenced to figure out what antigens will best help the immune system to recognise their cancer. Then a patient-specific version of mRNA-4157 is created that produces those antigens.
The latest results of a three-year, phase 2 clinical trial which combined pembrolizumab and mRNA-4157 were announced this past week. Overall, 2.5 years after starting the trial, 74.8% of patients treated with immunotherapy combined with mRNA-4157 post-surgery remained cancer-free, compared to 55.6% of those treated with immunotherapy alone. These were patients who were suffering from high-risk, late-stage forms of melanoma, who generally have poor outcomes.
It’s worth noting these results have not yet been published in peer-reviewed journals. They’re available as company announcements, and were also presented at some cancer conferences in the United States.
Based on the results of this trial, the combination of pembrolizumab and the vaccine progressed to a phase 3 trial in 2023, with the first patients being enrolled in Australia. But the final results of this trial are not expected until 2029.
It is hoped this mRNA-based anti-cancer vaccine will blaze a trail for vaccines targeting other types of cancer, not just melanoma, particularly in combination with checkpoint inhibitors to help stimulate the immune system.
Despite these ongoing advances in melanoma treatment, the best way to fight cancer is still prevention which, in the case of melanoma, means protecting yourself from UV exposure wherever possible.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research) and John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
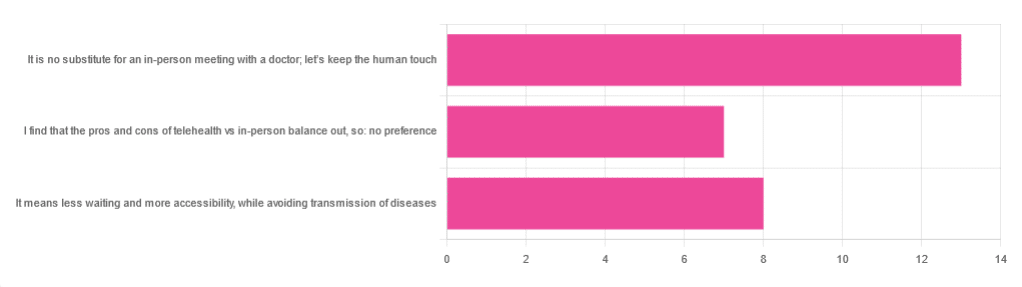
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: