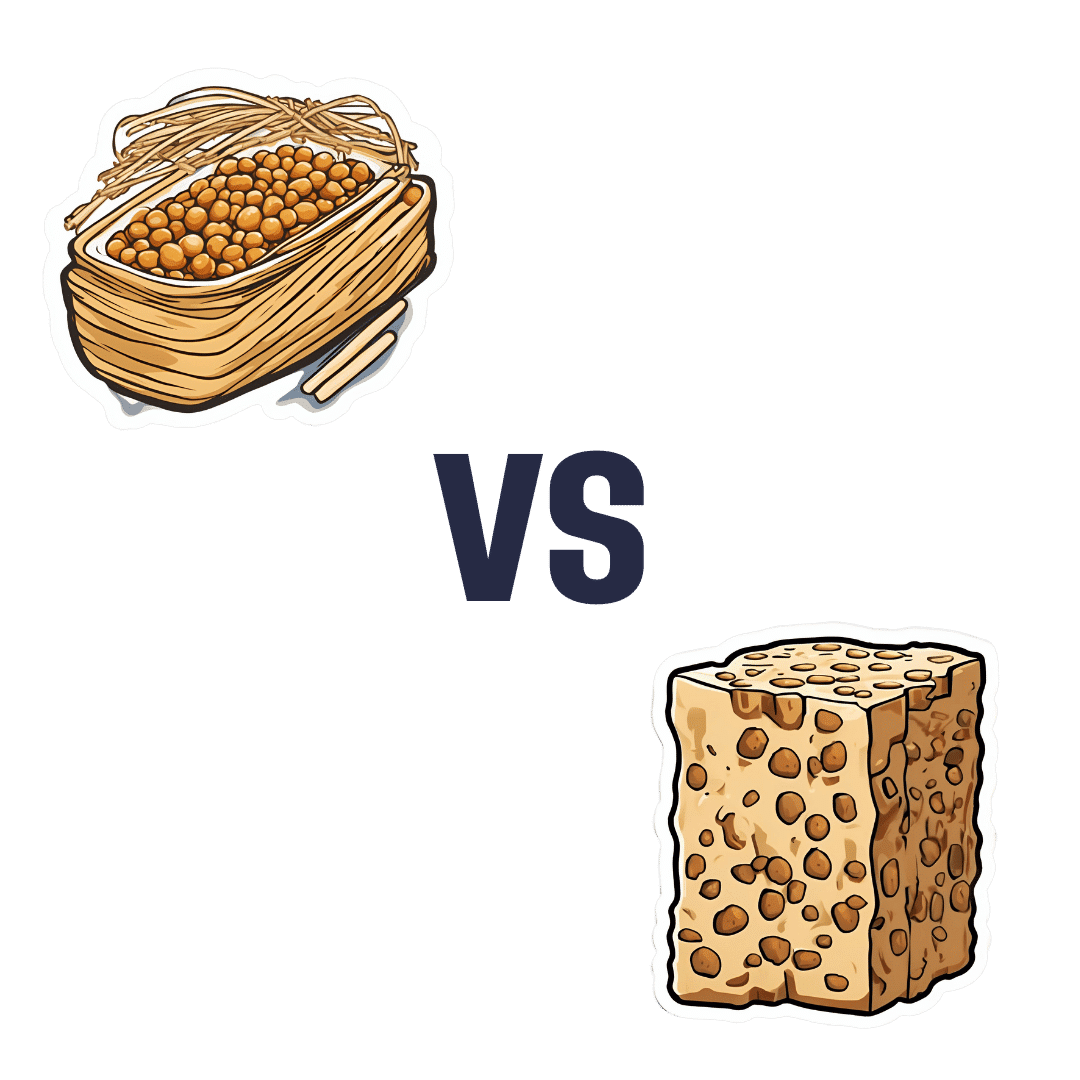
Natto vs Tempeh – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing nattō to tempeh, we picked the nattō.
Why?
Both are great, but in the battle of fermented soybeans vs fermented soybeans with extra steps, it turns out that the simplest option is the best, even if tempeh was a close runner-up:
In terms of macros, nattō has more carbs and fiber for the same protein and fat; we’ll call this category a tie or a marginal win for nattō.
In the category of vitamins, nattō has more of vitamins B1, C, E, K, and choline, while tempeh has more of vitamins B2, B3, B6, and B9. A clearer, yet still modest, win for nattō.
Minerals, however, are what really set them apart: nattō has more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc, while tempeh has more phosphorus. An overwhelming win for nattō this time.
In short: enjoy either or both, but nattō is the more nutritionally dense option!
Want to learn more?
You might like:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nattō is featured as part of the diet 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blue Cheese vs Brunost – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blue cheese to brunost, we picked the brunost.
Why?
First, for the unfamiliar, as brunost isn’t necessarily as popular as blue cheese in N. America where most of our readers are:
Brunost, literally “brown cheese” is a traditional Norwegian affair made from aggressively boiling milk, cream, and whey in an iron cauldron. Whereas the blue in blue cheese comes from mold, the brown in brown cheese comes from caramelizing the milk sugars in the cauldron. When we say “cauldron”, yes, there is nowadays mass-produced brunost that is no longer made in something that could be mistaken for a witch’s brew, but the use of cast iron is actually important to the process, and has been the subject of regulatory controversy in Norway; first the cast iron was abandoned, then because that changed the cheese they fortified the product with added iron supplementation, then that was banned, then they reversed it because it affected iron levels in the general population. Nowadays, it is usually made with iron, one way or another.
Ok, so let’s see how they stack up against each other:
In terms of macronutrients, the two cheeses are comparable in fat, but brunost has more carbs—because whereas bacteria (and to a lesser extent, the mold) ate nearly all the carbs in the blue cheese, the caramelization of the milk sugars in brunost meant the result stayed higher in carbs. Both are considered “low GI” foods, but this category is still at least a moderate win for blue cheese.
When it comes to vitamins, brunost is higher in vitamins A, B1, B2, B3, B5, B6, and B12, while blue cheese is higher in vitamin B9. In other words, a clear and easy win for brunost.
In the category of minerals, brunost has more copper, iron, magnesium, manganese, phosphorus, and potassium. Meanwhile, blue cheese contains more zinc, although we can also mention that blue cheese has about 2x the sodium, which is generally not considered a benefit. The two cheeses are about equal in calcium and selenium. Adding these up makes for another clear and easy win for brunost.
In short, unless you are strongly avoiding [even low-GI foods’] carbs for some reason, brunost wins the day by virtue of its overwhelmingly better vitamin and mineral content.
Still, like most fermented dairy products, both cheeses can be enjoyed in moderation as part of a healthy diet (assuming you don’t have an allergy/intolerance).
Want to learn more?
You might like to read:
Take care!
Share This Post
-
Feeding You Lies – by Vani Hari
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to advertising, we know that companies will often be as misleading as they can get away with. But just how misleading is it?
Vani Hari, of “Food Babe” fame, is here to unravel it all.
The book covers many areas of food and drink advertising and marketing, and gives particular attention to:
- Sodas (with and without sugar), and how deleterious they are to the health—as well as not even helping people lose weight, but actively hindering
- Nutritionally fortified foods, and what we may or may not actually get from them by the time the processing is done
- Organic food, and what that may or may not mean
She also covers a lot of what happens outside of supermarkets, way back in universities and corporate boardrooms. In short, who is crossing whose palms with silver for a seal of approval… And what that means for us as consumers.
A strength of this book that sets it apart from many of its genre, by the way, is that while being deeply critical of certain institutions’ practices, it doesn‘t digress into tinfoil-hat pseudoscientific scaremongering, either. Here at 10almonds we love actual science, so that was good to see too.
Bottom line: is you’d like to know “can they say that and get away with it if it’s not true?” and make decisions based on the actual nutritional value of things, this is a great book for you.
Click here to check out “Feeding You Lies” on Amazon and make your shopping healthier!
Share This Post
-
The Blood Sugar Solution – by Dr. Mark Hyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The main purpose of this book is combating metabolic disease, the amalgam of what’s often prediabetes (sometimes fully-fledged diabetes) and cardiovascular disease (sometimes fully-fledged heart disease).
To achieve this (after an introductory section explaining what the sociomedical problems are and why the sociomedical problems are happening), he offers a seven-step program; we’ll not keep those steps a mystery; they are:
- Boost your nutrition
- Regulate your hormones
- Reduce inflammation
- Improve your digestion
- Maximize detoxification
- Enhance energy metabolism
- Soothe your mind
Thereafter, it’s all about leading the reader by the hand through the steps; he also offers a six-week action plan, and a six-week meal plan with recipes.
The style is very sensationalist (too sensationalist for this reviewer’s personal taste) but nevertheless backed up with hard science when it comes to hard claims. So, if you don’t mind wading through (or skipping) some early chapters that are a bit “used car salesman” in feel, there’s actually a lot of good information, especially in the middle of the book, and useful practical guides in the middle and end.
Bottom line: if you want a good comprehensive science-based practical guide to addressing the risk of metabolic disease, this is that.
Click here to check out The Blood Sugar Solution, and look after yours!
Share This Post
Related Posts
-
How To Leverage Placebo Effect For Yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Placebo Effect: Making Things Work Since… Well, A Very Long Time Ago
The placebo effect is a well-known, well-evidenced factor that is very relevant when it comes to the testing and implementation of medical treatments:
NIH | National Center for Biotechnology Information | Placebo Effect
Some things that make placebo effect stronger include:
- Larger pills instead of small ones: because there’s got to be more going on in there, right?
- Thematically-colored pills: e.g. red for stimulant effects, blue for relaxing effects
- Things that seem expensive: e.g. a well-made large heavy machine, over a cheap-looking flimsy plastic device. Similarly, medication from a small glass jar with a childproof lock, rather than popped out from a cheap blister-pack.
- Things that seem rational: if there’s an explanation for how it works that you understand and find rational, or at least you believe you understand and find rational ← this works in advertising, too; if there’s a “because”, it lands better almost regardless of what follows the word “because”
- Things delivered confidently by a professional: this is similar to the “argument from authority” fallacy (whereby a proposed authority will be more likely trusted, even if this is not their area of expertise at all, e.g. celebrity endorsements), but in the case of placebo trials, this often looks like a well-dressed middle-aged or older man with an expensive haircut calling for a young confident-looking aide in a lab coat to administer the medicine, and is received better than a slightly frazzled academic saying “and, uh, this one’s yours” while handing you a pill.
- Things with ritual attached: this can be related to the above (the more pomp and circumstance is given to the administration of the treatment, the better), but it can also be as simple as an instruction on an at-home-trial medication saying “take 20 minutes before bed”. Because, if it weren’t important, they wouldn’t bother to specify that, right? So it must be important!
And now for a quick personality test
Did you see the above as a list of dastardly tricks to watch out for, or did you see the above as a list of things that can make your actual medication more effective?
It’s arguably both, of course, but the latter more optimistic view is a lot more useful than the former more pessimistic one.
Since placebo effect works at least somewhat even when you know about it, there is nothing to stop you from leveraging it for your own benefit when taking medication or doing health-related things.
Next time you take your meds or supplements or similar, pause for a moment for each one to remember what it is and what it will be doing for you. This is a lot like the principles (which are physiological as well as psychological) of mindful eating, by the way:
How To Get More Nutrition From The Same Food
Placebo makes some surprising things evidence-based
We’ve addressed placebo effect sometimes as part of an assessment of a given alternative therapy, often in our “Mythbusting Friday” edition of 10almonds.
- In some cases, placebo is adjuvant to the therapy, i.e. it is one of multiple mechanisms of action (example: chiropractic or acupuncture)
- In some cases, placebo is the only known mechanism of action (example: homeopathy)
- In some cases, even placebo can’t help (example: ear candling)
One other fascinating and far-reaching (in a potentially good way) thing that placebo makes evidence-based is: prayer
…which is particularly interesting for something that is fundamentally faith-based, i.e. the opposite of evidence-based.
Now, we’re a health science publication, not a theological publication, so we’ll consider actual divine intervention to be beyond the scope of mechanisms of action we can examine, but there’s been a lot of research done into the extent to which prayer is beneficial as a therapy, what things it may be beneficial for, and what factors affect whether it helps:
Prayer and healing: A medical and scientific perspective on randomized controlled trials
👆 full paper here, and it is very worthwhile reading if you have time, whether or not you are religious personally
Placebo works best when there’s a clear possibility for psychosomatic effect
We’ve mentioned before, and we’ll mention again:
- psychosomatic effect does not mean: “imagining it”
- psychosomatic effect means: “your brain regulates almost everything else in your body, directly or indirectly, including your autonomic functions, and especially notably when it comes to illness, your immune responses”
So, a placebo might well heal your rash or even shrink a tumor, but it probably won’t regrow a missing limb, for instance.
And, this is important: it’s not about how credible/miraculous the outcome will be!
Rather, it is because we have existing pre-programmed internal bodily processes for healing rashes and shrinking tumors, that just need to be activated—whereas we don’t have existing pre-programmed internal bodily processes for regrowing a missing limb, so that’s not something our brain can just tell our body to do.
So for this reason, in terms of what placebo can and can’t do:
- Get rid of cancer? Yes, sometimes—because the body has a process for doing that; enjoy your remission
- Fix a broken nail? No—because the body has no process for doing that; you’ll just have to cut it and wait for it to grow again
With that in mind, what will you use the not-so-mystical powers of placebo for? What ever you go for… Enjoy, and take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What does it mean to be transgender?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Transgender media coverage has surged in recent years for a wide range of reasons. While there are more transgender television characters than ever before, hundreds of bills are targeting transgender people’s access to medical care, sports teams, gender-specific public spaces, and other institutions.
Despite the increase in conversation about the transgender community, public confusion around transgender identity remains.
Read on to learn more about what it means to be transgender and understand challenges transgender people may face.
What does it mean to be transgender?
Transgender—or “trans”—is an umbrella term for people whose gender identity or gender expression does not conform to their sex assigned at birth. People can discover they are trans at any age.
Gender identity refers to a person’s inner sense of being a woman, a man, neither, both, or something else entirely. Trans people who don’t feel like women or men might describe themselves as nonbinary, agender, genderqueer, or two-spirit, among other terms.
Gender expression describes the way a person communicates their gender through their appearance—such as their clothing or hairstyle—and behavior.
A person whose gender expression doesn’t conform to the expectations of their assigned sex may not identify as trans. The only way to know for sure if someone is trans is if they tell you.
Cisgender—or “cis”—describes people whose gender identities match the sex they were assigned at birth.
How long have transgender people existed?
Being trans isn’t new. Although the word “transgender” only dates back to the 1960s, people whose identities defy traditional gender expectations have existed across cultures throughout recorded history.
How many people are transgender?
A 2022 Williams Institute study estimates that 1.6 million people over the age of 13 identify as transgender in the United States.
Is being transgender a mental health condition?
No. Conveying and communicating about your gender in a way that feels authentic to you is a normal and necessary part of self-expression.
Social and legal stigma, bullying, discrimination, harassment, negative media messages, and barriers to gender-affirming medical care can cause psychological distress for trans people. This is especially true for trans people of color, who face significantly higher rates of violence, poverty, housing instability, and incarceration—but trans identity itself is not a mental health condition.
What is gender dysphoria?
Gender dysphoria describes a feeling of unease that some trans people experience when their perceived gender doesn’t match their gender identity, or their internal sense of gender. A 2021 study of trans adults pursuing gender-affirming medical care found that most participants started experiencing gender dysphoria by the time they were 7.
When trans people don’t receive the support they need to manage gender dysphoria, they may experience depression, anxiety, social isolation, suicidal ideation, substance use disorder, eating disorders, and self-injury.
How do trans people manage gender dysphoria?
Every trans person’s experience with gender dysphoria is unique. Some trans people may alleviate dysphoria by wearing gender-affirming clothing or by asking others to refer to them by a new name and use pronouns that accurately reflect their gender identity. The 2022 U.S. Trans Survey found that nearly all trans participants who lived as a different gender than the sex they were assigned at birth reported that they were more satisfied with their lives.
Some trans people may also manage dysphoria by pursuing medical transition, which may involve taking hormones and getting gender-affirming surgery.
Access to gender-affirming medical care has been shown to reduce the risk of depression and suicide among trans youth and adults.
To learn more about the trans community, visit resources from the National Center for Transgender Equality, the Trevor Project, PFLAG, and Planned Parenthood.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Hospital Kept a Brain-Damaged Patient on Life Support to Boost Statistics. His Sister Is Now Suing for Malpractice.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
In 2018, Darryl Young was hoping for a new lease on life when he received a heart transplant at a New Jersey hospital after years of congestive heart failure. But he suffered brain damage during the procedure and never woke up.
The following year, a ProPublica investigation revealed that Young’s case was part of a pattern of heart transplants that had gone awry at Newark Beth Israel Medical Center in 2018. The spate of bad outcomes had pushed the center’s percentage of patients still alive one year after surgery — a key benchmark — below the national average. Medical staff were under pressure to boost that metric. ProPublica published audio recordings from meetings in which staff discussed the need to keep Young alive for a year, because they feared another hit to the program’s survival rate would attract scrutiny from regulators. On the recordings, the transplant program’s director, Dr. Mark Zucker, cautioned his team against offering Young’s family the option of switching from aggressive care to comfort care, in which no lifesaving efforts would be made. He acknowledged these actions were “very unethical.”
ProPublica’s revelations horrified Young’s sister Andrea Young, who said she was never given the full picture of her brother’s condition, as did the findings of a subsequent federal regulator’s probe that determined that the hospital was putting patients in “immediate jeopardy.” Last month, she filed a medical malpractice lawsuit against the hospital and members of her brother’s medical team.
The lawsuit alleges that Newark Beth Israel staff were “negligent and deviated from accepted standards of practice,” leading to Young’s tragic medical outcome.
Defendants in the lawsuit haven’t yet filed responses to the complaint in court documents. But spokesperson Linda Kamateh said in an email that “Newark Beth Israel Medical Center is one of the top heart transplant programs in the nation and we are committed to serving our patients with the highest quality of care. As this case is in active litigation, we are unable to provide further detail.” Zucker, who is no longer on staff at Newark Beth Israel, didn’t respond to requests for comment. His attorney also didn’t respond to calls and emails requesting comment.
Zucker also didn’t respond to requests for comment from ProPublica in 2018; Newark Beth Israel at the time said in a statement, made on behalf of Zucker and other staff, that “disclosures of select portions of lengthy and highly complex medical discussions, when taken out of context, may distort the intent of conversations.”
The lawsuit alleges that Young suffered brain damage as a result of severely low blood pressure during the transplant surgery. In 2019, when the federal Centers for Medicare and Medicaid Services scrutinized the heart transplant program following ProPublica’s investigation, the regulators found that the hospital had failed to implement corrective measures even after patients suffered, leading to further harm. For example, one patient’s kidneys failed after a transplant procedure in August 2018, and medical staff made recommendations internally to increase the frequency of blood pressure measurement during the procedure, according to the lawsuit. The lawsuit alleges that the hospital didn’t implement its own recommendations and that one month later, “these failures were repeated” in Young’s surgery, leading to brain damage.
The lawsuit also alleges that Young wasn’t asked whether he had an advance directive, such as a preference for a do-not-resuscitate order, despite a hospital policy stating that patients should be asked at the time of admission. The lawsuit also noted that CMS’ investigation found that Andrea Young was not informed of her brother’s condition.
Andrea Young said she understands that mistakes can happen during medical procedures, “however, it’s their duty and their responsibility to be honest and let the family know exactly what went wrong.” Young said she had to fight to find out what was going on with her brother, at one point going to the library and trying to study medical books so she could ask the right questions. “I remember as clear as if it were yesterday, being so desperate for answers,” she said.
Andrea Young said that she was motivated to file the lawsuit because she wants accountability. “Especially with the doctors never, from the outset, being forthcoming and truthful about the circumstances of my brother’s condition, not only is that wrong and unethical, but it took a lot away from our entire family,” she said. “The most important thing to me is that those responsible be held accountable.”
ProPublica’s revelation of “a facility putting its existence over that of a patient is a scary concept,” said attorney Jonathan Lomurro, who’s representing Andrea Young in this case with co-counsel Christian LoPiano. Besides seeking damages for Darryl Young’s children, “we want to call attention to this so it doesn’t happen again,” Lomurro said.
The lawsuit further alleges that medical staff at Newark Beth Israel invaded Young’s privacy and violated the Health Insurance Portability and Accountability Act, more commonly known as HIPAA, by sharing details of his case with the media without his permission. “We want people to be whistleblowers and want information out,” but that information should be told to patients and their family members directly, Lomurro said.
The 2019 CMS investigation determined that Newark Beth Israel’s program placed patients in “immediate jeopardy,” the most serious level of violation, and required the hospital to implement corrective plans. Newark Beth Israel did not agree with all of the regulator’s findings and in a statement at the time said that the CMS team lacked the “evidence, expertise and experience” to assess and diagnose patient outcomes.
The hospital did carry out the corrective plans and continues to operate a heart transplant program today. The most recent federal data, based on procedures from January 2021 through June 2023, shows that the one year probability of survival for a patient at Newark Beth is lower than the national average. It also shows that the number of graft failures, including deaths, in that time period was higher than the expected number of deaths for the program.
Andrea Young said she’s struggled with a feeling of emptiness in the years after her brother’s surgery. They were close and called each other daily. “There’s nothing in the world that can bring my brother back, so the only solace I will have is for the ones responsible to be held accountable,” she said. Darryl Young died on Sept 12, 2022, having never woken up after the transplant surgery.
A separate medical malpractice lawsuit filed in 2020 by the wife of another Newark Beth Israel heart transplant patient who died after receiving an organ infected with a parasitic disease is ongoing. The hospital has denied the allegations in court filing. The state of New Jersey, employer of the pathologists named in the case, settled for $1.7 million this month, according to the plaintiff’s attorney Christian LoPiano. The rest of the case is ongoing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: