The Counterintuitive Dos and Don’ts of Nail Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I take a vitamin supplement for strengthening my nails (particularly one of my big toes!) – but they are running out! What do you recommend for strengthening nails? What is/are the key ingredient(s)?❞
Vitamin-wise, biotin (vitamin B7) is an underrated and very important one. As a bonus, it’s really good for your hair too (hair and nails being made of fundamentally the same “stuff”. Because it has exceptionally low toxicity, it can be taken up to 10,000% of the NRV, so if shopping for supplements, a high biotin content is better than a low one.
A lot of products marketed as for “skin, hair, and nails” focus on vitamins A and E, which are good for the skin but aren’t so relevant for nails.
Nutritionally, getting plenty of protein (whatever form you normally take it is fine) is also important since keratin (as nails are made of) is a kind of protein.
Outside of nutritional factors, a few other considerations:
- Testosterone strengthens nails, and declining testosterone levels (as experienced by most men over the age of 45) can result in weaker nails. So for men over 45 especially, a diet that favors testosterone (think foods rich in magnesium and zinc) is good.
- Because estrogen doesn’t do for women’s nails what testosterone does for men’s nails, increasing our magnesium and zinc intake won’t help our nails (but it’s still good for other things, including energy levels in the day and good sleep at night, and most people are deficient in magnesium anyway)
- Those of us who enjoy painted nails would do well to let our nails go without polish sometimes, as it can dry them out. And, acrylic nails are truly ruinous to nail health, as are gel nails (the kind that use a UV lamp to harden them—which is also bad for the skin)
- When nails are brittle, it can be tempting to soak them to reduce their brittleness. However, this is actually counterproductive, as the water will leech nutrients from the nails, and by the time you’ve been out of the footbath (for example) for about an hour, your nails will bemore brittle than before you soaked them.
- Use a moisturizing lotion or nail-oil instead—bonus if it contains biotin, keratin, and/or other helpful nutrients.
- Keep yourself hydrated, too! Hydration that comes to your nails from the inside will deliver nutrients, rather than removing them.
About those supplements: we don’t sell them (or anything else) but for your convenience, here are some great ones (this writer takes pretty much the same, just a different brand because I’m in a different country):
Magnesium Gummies (600mg) & Biotin Gummies (10,000µg)
Enjoy!
❝I was wondering whether there were very simple, clear bullet points or instructions on things to be wary of in Yoga.❞
That’s quite a large topic, and not one that lends itself well to being conveyed in bullet points, but first we’ll share the article you sent us when sending this question:
Tips for Avoiding Yoga Injuries
…and next we’ll recommend the YouTube channel @livinleggings, whose videos we feature here from time to time. She (Liv) has a lot of good videos on problems/mistakes/injuries to avoid.
Here’s a great one to get you started:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
California Is Investing $500M in Therapy Apps for Youth. Advocates Fear It Won’t Pay Off.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With little pomp, California launched two apps at the start of the year offering free behavioral health services to youths to help them cope with everything from living with anxiety to body acceptance.
Through their phones, young people and some caregivers can meet BrightLife Kids and Soluna coaches, some who specialize in peer support or substance use disorders, for roughly 30-minute virtual counseling sessions that are best suited to those with more mild needs, typically those without a clinical diagnosis. The apps also feature self-directed activities, such as white noise sessions, guided breathing, and videos of ocean waves to help users relax.
“We believe they’re going to have not just great impact, but wide impact across California, especially in places where maybe it’s not so easy to find an in-person behavioral health visit or the kind of coaching and supports that parents and young people need,” said Gov. Gavin Newsom’s health secretary, Mark Ghaly, during the Jan. 16 announcement.
The apps represent one of the Democratic governor’s major forays into health technology and come with four-year contracts valued at $498 million. California is believed to be the first state to offer a mental health app with free coaching to all young residents, according to the Department of Health Care Services, which operates the program.
However, the rollout has been slow. Only about 15,000 of the state’s 12.6 million children and young adults have signed up for the apps, school counselors say they’ve never heard of them, and one of the companies isn’t making its app available on Android phones until summer.
Advocates for youth question the wisdom of investing taxpayer dollars in two private companies. Social workers are concerned the companies’ coaches won’t properly identify youths who need referrals for clinical care. And the spending is drawing lawmaker scrutiny amid a state deficit pegged at as much as $73 billion.
An App for That
Newsom’s administration says the apps fill a need for young Californians and their families to access professional telehealth for free, in multiple languages, and outside of standard 9-to-5 hours. It’s part of Newsom’s sweeping $4.7 billion master plan for kids’ mental health, which was introduced in 2022 to increase access to mental health and substance use support services. In addition to launching virtual tools such as the teletherapy apps, the initiative is working to expand workforce capacity, especially in underserved areas.
“The reality is that we are rarely 6 feet away from our devices,” said Sohil Sud, director of Newsom’s Children and Youth Behavioral Health Initiative. “The question is how we can leverage technology as a resource for all California youth and families, not in place of, but in addition to, other behavioral health services that are being developed and expanded.”
The virtual platforms come amid rising depression and suicide rates among youth and a shortage of mental health providers. Nearly half of California youths from the ages of 12 to 17 report having recently struggled with mental health issues, with nearly a third experiencing serious psychological distress, according to a 2021 study by the UCLA Center for Health Policy Research. These rates are even higher for multiracial youths and those from low-income families.
But those supporting youth mental health at the local level question whether the apps will move the needle on climbing depression and suicide rates.
“It’s fair to applaud the state of California for aggressively seeking new tools,” said Alex Briscoe of California Children’s Trust, a statewide initiative that, along with more than 100 local partners, works to improve the social and emotional health of children. “We just don’t see it as fundamental. And we don’t believe the youth mental health crisis will be solved by technology projects built by a professional class who don’t share the lived experience of marginalized communities.”
The apps, BrightLife Kids and Soluna, are operated by two companies: Brightline, a 5-year-old venture capital-backed startup; and Kooth, a London-based publicly traded company that has experience in the U.K. and has also signed on some schools in Kentucky and Pennsylvania and a health plan in Illinois. In the first five months of Kooth’s Pennsylvania pilot, 6% of students who had access to the app signed up.
Brightline and Kooth represent a growing number of health tech firms seeking to profit in this space. They beat out dozens of other bidders including international consulting companies and other youth telehealth platforms that had already snapped up contracts in California.
Although the service is intended to be free with no insurance requirement, Brightline’s app, BrightLife Kids, is folded into and only accessible through the company’s main app, which asks for insurance information and directs users to paid licensed counseling options alongside the free coaching. After KFF Health News questioned why the free coaching was advertised below paid options, Brightline reordered the page so that, even if a child has high-acuity needs, free coaching shows up first.
The apps take an expansive view of behavioral health, making the tools available to all California youth under age 26 as well as caregivers of babies, toddlers, and children 12 and under. When KFF Health News asked to speak with an app user, Brightline connected a reporter with a mother whose 3-year-old daughter was learning to sleep on her own.
‘It’s Like Crickets’
Despite being months into the launch and having millions in marketing funds, the companies don’t have a definitive rollout timeline. Brightline said it hopes to have deployed teams across the state to present the tools in person by midyear. Kooth said developing a strategy to hit every school would be “the main focus for this calendar year.”
“It’s a big state — 58 counties,” Bob McCullough of Kooth said. “It’ll take us a while to get to all of them.”
So far BrightLife Kids is available only on Apple phones. Brightline said it’s aiming to launch the Android version over the summer.
“Nobody’s really done anything like this at this magnitude, I think, in the U.S. before,” said Naomi Allen, a co-founder and the CEO of Brightline. “We’re very much in the early innings. We’re already learning a lot.”
The contracts, obtained by KFF Health News through a records request, show the companies operating the two apps could earn as much as $498 million through the contract term, which ends in June 2027, months after Newsom is set to leave office. And the state is spending hundreds of millions more on Newsom’s virtual behavioral health strategy. The state said it aims to make the apps available long-term, depending on usage.
The state said 15,000 people signed up in the first three months. When KFF Health News asked how many of those users actively engaged with the app, it declined to say, noting that data would be released this summer.
KFF Health News reached out to nearly a dozen California mental health professionals and youths. None of them were aware of the apps.
“I’m not hearing anything,” said Loretta Whitson, executive director of the California Association of School Counselors. “It’s like crickets.”
Whitson said she doesn’t think the apps are on “anyone’s” radar in schools, and she doesn’t know of any schools that are actively advertising them. Brightline will be presenting its tool to the counselor association in May, but Whitson said the company didn’t reach out to plan the meeting; she did.
Concern Over Referrals
Whitson isn’t comfortable promoting the apps just yet. Although both companies said they have a clinical team on staff to assist, Whitson said she’s concerned that the coaches, who aren’t all licensed therapists, won’t have the training to detect when users need more help and refer them to clinical care.
This sentiment was echoed by other school-based social workers, who also noted the apps’ duplicative nature — in some counties, like Los Angeles, youths can access free virtual counseling sessions through Hazel Health, a for-profit company. Nonprofits, too, have entered this space. For example, Teen Line, a peer-to-peer hotline operated by Southern California-based Didi Hirsch Mental Health Services, is free nationwide.
While the state is also funneling money to the schools as part of Newsom’s master plan, students and school-based mental health professionals voiced confusion at the large app investment when, in many school districts, few in-person counseling roles exist, and in some cases are dwindling.
Kelly Merchant, a student at College of the Desert in Palm Desert, noted that it can be hard to access in-person therapy at her school. She believes the community college, which has about 15,000 students, has only one full-time counselor and one part-time bilingual counselor. She and several students interviewed by KFF Health News said they appreciated having engaging content on their phone and the ability to speak to a coach, but all said they’d prefer in-person therapy.
“There are a lot of people who are seeking therapy, and people close to me that I know. But their insurances are taking forever, and they’re on the waitlist,” Merchant said. “And, like, you’re seeing all these people struggle.”
Fiscal conservatives question whether the money could be spent more effectively, like to bolster county efforts and existing youth behavioral health programs.
Republican state Sen. Roger Niello, vice chair of the Senate Budget and Fiscal Review Committee, noted that California is forecasted to face deficits for the next three years, and taxpayer watchdogs worry the apps might cost even more in the long run.
“What starts as a small financial commitment can become uncontrollable expenses down the road,” said Susan Shelley of the Howard Jarvis Taxpayers Association.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Can You Get Addicted To MSG, Like With Sugar?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Hello, I love your newsletter 🙂 Can I have a question? While browsing through your recepies, I realised many contained MSG. As someone based in Europe, I am not used to using MSG while cooking (of course I know that processed food bought in supermarket containes MSG). There is a stigma, that MSG is not particulary healthy, but rather it should be really bad and cause negative effects like headaches. Is this true? Also, can you get addicted to MSG, just like you get addicted to sugar? Thank you :)❞
Thank you for the kind words, and the interesting questions!
Short answer: no and no 🙂
Longer answer: most of the negative reputation about MSG comes from a single piece of satire written in the US in the 1960s, which the popular press then misrepresented as a genuine concern, and the public then ran with, mostly due to racism/xenophobia/sinophobia specifically, given the US’s historically not fabulous relations with China, and the moniker of “Chinese restaurant syndrome”, notwithstanding that MSG was first isolated in Japan, not China, more than 100 years ago.
The silver lining that comes out of this is that because of the above, MSG has been one of the most-studied food additives in recent decades, with many teams of scientists in many countries trying to determine its risks and not finding any (except insofar as anything in extreme quantities can kill you, including water or oxygen).
You can read more about this and other* myths about MSG, here:
Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
*such as pertaining to gluten sensitivity, which in reality MSG has no bearing on whatsoever as it does not contain gluten and is not even made of the same basic stuff; gluten being a protein made of (amongst other things) the amino acid glutamine, not a glutamate salt. Glutamate is as closely related to gluten as cyanocobalamin (vitamin B12) is to cyanide (the famous poison).
PS: if you didn’t click the above link to read that article, then 1) we really do recommend it 2) we did some LD50 calculations there and looked at available research, and found that for someone of this writer’s (very medium) size, eating 1kg of MSG at once is sufficient to cause toxicity, and injecting >250g of MSG may cause heart problems. So we don’t recommend doing that.
However, ½ tsp in a recipe that gives multiple portions is not going to get you anywhere close to the danger zone, unless you consume that entire meal by yourself hundreds of times per day. And if you do, the MSG is probably the least of your concerns.
(2 tsp of cassia cinnamon, however, is enough to cause coumarin toxicity; for this reason we recommend Ceylon (or “True” or “Sweet”) cinnamon in our recipes, as it has almost undetectable levels of coumarin)
With regard to your interesting question about addiction, first of all let’s speak briefly about sugar addiction:
Sugar addiction is, by broad scientific consensus, agreed-upon as an extant thing that does exist, and contemporary research is more looking into the “hows” and “whys” and “whats” rather than the “whether”. It is a somewhat complicated topic, because it’s halfway between what science would usually consider a chemical addiction, and what science would usually consider a behavioral addiction:
The Not-So-Sweet Science Of Sugar Addiction
The reasonable prevailing hypothesis, therefore, is that sugar simply has two moderate mechanisms of addiction, rather than one strong one.
The biochemical side of sugar addiction comes from the body’s metabolism of sugar, so this cannot be a thing for MSG, because there is nothing to metabolize in the same sense of the word (MSG being an inorganic compound with zero calories).
People can crave salt, especially when deficient in it, and MSG does contain sodium (it’s what the “S” stands for), but it contains a little under ⅓ of the sodium that table salt does (sodium chloride in whatever form, be it sea salt, rock salt, or such):
MSG vs. Salt: Sodium Comparison ← we do molecular calculations here!
Sea Salt vs MSG – Which is Healthier? ← this one for a head-to-head
However, even craving salt does not constitute an addiction; nobody is shamefully hiding their rock salt crystals under their bed and getting a fix when they feel low, and nor does withdrawal cause adverse side effects, except insofar as (once again) a person deficient in salt will crave salt.
Finally, the only other way we know of that one might wonder if MSG could be addictive, is about glutamate and glutamate receptors. The glutamate in MSG is the same glutamate (down to the atoms) as the glutamate formed if one consumes tomatoes in the presence of salt, and triggers the same glutamate receptors in the same way. We have the same number of receptors either way, and uptake is exactly the same (because again, it’s exactly the same chemical) so there is a maximum to how strong this effect can be, and that maximum is the same whatever the source of the glutamate was.
In this respect, if MSG is addictive, then so is a tomato salad with a pinch of salt: it’s not—it’s just tasty.
We haven’t cited papers in today’s article, but it’s just because we cited them already in the articles we linked, and so we avoided doubling up. Most of them are in that first link we gave 🙂
One final note
Technically anyone can develop a sensitivity to anything, so in theory someone could develop a sensitivity to MSG, just like they could for any other ingredient. Our usual legal/medical disclaimer applies.
However, it’s certainly not a common trigger, putting it well below common allergens like nuts (or less common allergens like, say, bananas), not even in the same league as common intolerances such as gluten, and less worthy of health risk warnings than, say, spinach (high in oxalates; fine for most people but best avoided if you have kidney problems).
The reason we use it in the recipes we use it in, is simply because it’s a lower-sodium alternative to salt, and while it contains a (very) tiny bit less sodium than low-sodium salt (which itself has about ⅓ the sodium of regular salt), it has more of a flavor-enhancing effect, such that one can use half as much, for a more than sixfold total sodium reduction. Which for most of us in the industrialized world, is beneficial.
Want to try some?
If today’s article has inspired you to give MSG a try, here’s an example product on Amazon 😎
Enjoy!
Share This Post
-
Broccoli vs Cauliflower – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to cauliflower, we picked the broccoli.
Why?
This one is quite straightforward. Superficially, they’re very similar:
Both are great cruciferous vegetables with many health benefits to offer. Even for those keen to avoid oxalates, which cruciferous vegetables in general can be high in, these ones are quite low.
However, if you have IBS, you might want to avoid both, for their raffinose content that may cause problems for you.
For pretty much everyone else, unless you have a special reason why it’s not the case for you, both are a good source of abundant vitamins and minerals, and yet…
Anything cauliflower can do, broccoli can do better!
Broccoli contains more of the vitamins they both contain, and more of the minerals they both contain.
Broccoli also beats cauliflower on amino acids (except lysine), and contains a lot more lutein and zeaxanthin, carotenoids important for healthy eyes and brain.
So by all means enjoy both, but if you’re going to pick one, pick broccoli!
Want to know more?
Check out: Brain Food? The Eyes Have It!
Enjoy!
Share This Post
Related Posts
-
Reflexology: What The Science Says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
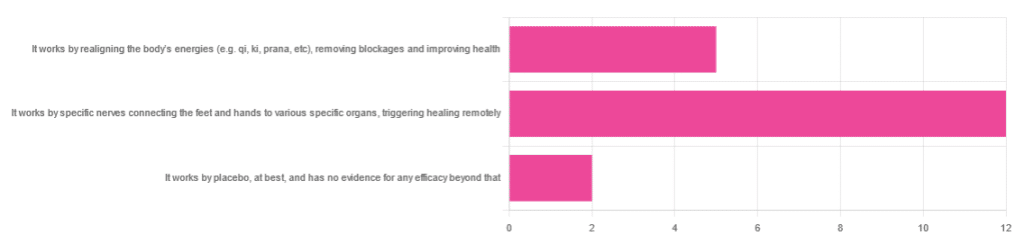
How Does Reflexology Work, Really?
In Wednesday’s newsletter, we asked you for your opinion of reflexology, and got the above-depicted, below-described set of responses:
- About 63% said “It works by specific nerves connecting the feet and hands to various specific organs, triggering healing remotely”
- About 26% said “It works by realigning the body’s energies (e.g. qi, ki, prana, etc), removing blockages and improving health“
- About 11% said “It works by placebo, at best, and has no evidence for any efficacy beyond that”
So, what does the science say?
It works by realigning the body’s energies (e.g. qi, ki, prana, etc), removing blockages and improving health: True or False?
False, or since we can’t prove a negative: there is no reliable scientific evidence for this.
Further, there is no reliable scientific evidence for the existence of qi, ki, prana, soma, mana, or whatever we want to call it.
To save doubling up, we did discuss this in some more detail, exploring the notion of qi as bioelectrical energy, including a look at some unreliable clinical evidence for it (a study that used shoddy methodology, but it’s important to understand what they did wrong, to watch out for such), when we looked at [the legitimately very healthful practice of] qigong, a couple of weeks ago:
Qigong: A Breath Of Fresh Air?
As for reflexology specifically: in terms of blockages of qi causing disease (and thus being a putative therapeutic mechanism of action for attenuating disease), it’s an interesting hypothesis but in terms of scientific merit, it was pre-emptively supplanted by germ theory and other similarly observable-and-measurable phenomena.
We say “pre-emptively”, because despite orientalist marketing, unless we want to count some ancient pictures of people getting a foot massage and say it is reflexology, there is no record of reflexology being a thing before 1913 (and that was in the US, by a laryngologist working with a spiritualist to produce a book that they published in 1917).
It works by specific nerves connecting the feet and hands to various specific organs, triggering healing remotely: True or False?
False, or since we can’t prove a negative: there is no reliable scientific evidence for this.
A very large independent review of available scientific literature found the current medical consensus on reflexology is that:
- Reflexology is effective for: anxiety (but short lasting), edema, mild insomnia, quality of sleep, and relieving pain (short term: 2–3 hours)
- Reflexology is not effective for: inflammatory bowel disease, fertility treatment, neuropathy and polyneuropathy, acute low back pain, sub acute low back pain, chronic low back pain, radicular pain syndromes (including sciatica), post-operative low back pain, spinal stenosis, spinal fractures, sacroiliitis, spondylolisthesis, complex regional pain syndrome, trigger points / myofascial pain, chronic persistent pain, chronic low back pain, depression, work related injuries of the hip and pelvis
Source: Reflexology – a scientific literary review compilation
(the above is a fascinating read, by the way, and its 50 pages go into a lot more detail than we have room to here)
Now, those items that they found it effective for, looks suspiciously like a short list of things that placebo is often good for, and/or any relaxing activity.
Another review was not so generous:
❝The best evidence available to date does not demonstrate convincingly that reflexology is an effective treatment for any medical condition❞
~ Dr. Edzard Ernst (MD, PhD, FMedSci)
Source: Is reflexology an effective intervention? A systematic review of randomised controlled trials
In short, from the available scientific literature, we can surmise:
- Some researchers have found it to have some usefulness against chiefly psychosomatic conditions
- Other researchers have found the evidence for even that much to be uncompelling
It works by placebo, at best, and has no evidence for any efficacy beyond that: True or False?
Mostly True; of course reflexology runs into similar problems as acupuncture when it comes to testing against placebo:
How Does One Test Acupuncture Against Placebo Anyway?
…but not quite as bad, since it is easier to give a random foot massage while pretending it is a clinical treatment, than to fake putting needles into key locations.
However, as the paper we cited just above (in answer to the previous True/False question) shows, reflexology does not appear to meaningfully outperform placebo—which points to the possibility that it does work by placebo, and is just a placebo treatment on the high end of placebo (because the placebo effect is real, does work, isn’t “nothing”, and some placebos work better than others).
For more on the fascinating science and useful (applicable in daily life!) practicalities of how placebo does work, check out:
How To Leverage Placebo Effect For Yourself
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Not-So-Sweet Science Of Sugar Addiction
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One
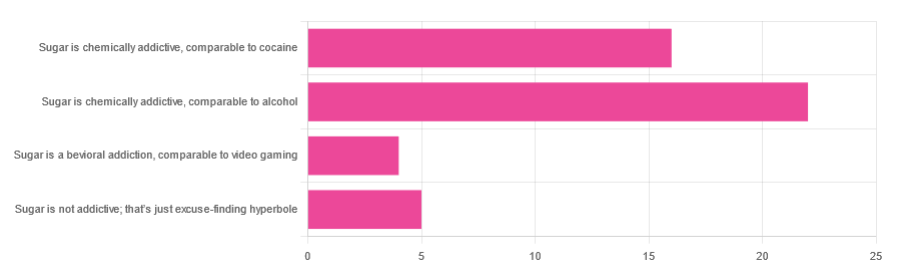
LumpMechanism Of Addiction Or Two?In Tuesday’s newsletter, we asked you to what extent, if any, you believe sugar is addictive; we got the above-depicted, below-described, set of responses:
- About 47% said “Sugar is chemically addictive, comparable to alcohol”
- About 34% said “Sugar is chemically addictive, comparable to cocaine”
- About 11% said “Sugar is not addictive; that’s just excuse-finding hyperbole”
- About 9% said “Sugar is a behavioral addiction, comparable to video gaming”
So what does the science say?
Sugar is not addictive; that’s just excuse-finding hyperbole: True or False?
False, by broad scientific consensus. As ever, the devil’s in the
detailsdefinitions, but while there is still discussion about how best to categorize the addiction, the scientific consensus as a whole is generally: sugar is addictive.That doesn’t mean scientists* are a hive mind, and so there will be some who disagree, but most papers these days are looking into the “hows” and “whys” and “whats” of sugar addiction, not the “whether”.
*who are also, let us remember, a diverse group including chemists, neurobiologists, psychologists, social psychologists, and others, often collaborating in multidisciplinary teams, each with their own focus of research.
Here’s what the Center of Alcohol and Substance Use Studies has to say, for example:
Sugar Addiction: More Serious Than You Think
Sugar is a chemical addiction, comparable to alcohol: True or False?
True, broadly, with caveats—for this one, the crux lies in “comparable to”, because the neurology of the addiction is similar, even if many aspects of it chemically are not.
In both cases, sugar triggers the release of dopamine while also (albeit for different chemical reasons) having a “downer” effect (sugar triggers the release of opioids as well as dopamine).
Notably, the sociology and psychology of alcohol and sugar addictions are also similar (both addictions are common throughout different socioeconomic strata as a coping mechanism seeking an escape from emotional pain).
See for example in the Journal of Psychoactive Drugs:
On the other hand, withdrawal symptoms from heavy long-term alcohol abuse can kill, while withdrawal symptoms from sugar are very much milder. So there’s also room to argue that they’re not comparable on those grounds.
Sugar is a chemical addiction, comparable to cocaine: True or False?
False, broadly. There are overlaps! For example, sugar drives impulsivity to seek more of the substance, and leads to changes in neurobiological brain function which alter emotional states and subsequent behaviours:
The impact of sugar consumption on stress driven, emotional and addictive behaviors
However!
Cocaine triggers a release of dopamine (as does sugar), but cocaine also acts directly on our brain’s ability to remove dopamine, serotonin, and norepinephrine:
The Neurobiology of Cocaine Addiction
…meaning that in terms of comparability, they (to use a metaphor now, not meaning this literally) both give you a warm feeling, but sugar does it by turning up the heating a bit whereas cocaine does it by locking the doors and burning down the house. That’s quite a difference!
Sugar is a behavioral addiction, comparable to video gaming: True or False?
True, with the caveat that this a “yes and” situation.
There are behavioral aspects of sugar addiction that can reasonably be compared to those of video gaming, e.g. compulsion loops, always the promise of more (without limiting factors such as overdosing), anxiety when the addictive element is not accessible for some reason, reduction of dopaminergic sensitivity leading to a craving for more, etc. Note that the last is mentioning a chemical but the mechanism itself is still behavioral, not chemical per se.
So, yes, it’s a behavioral addiction [and also arguably chemical in the manners we’ve described earlier in this article].
For science for this, we refer you back to:
The impact of sugar consumption on stress driven, emotional and addictive behaviors
Want more?
You might want to check out:
Beating Food Addictions: When It’s More Than “Just” Cravings
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
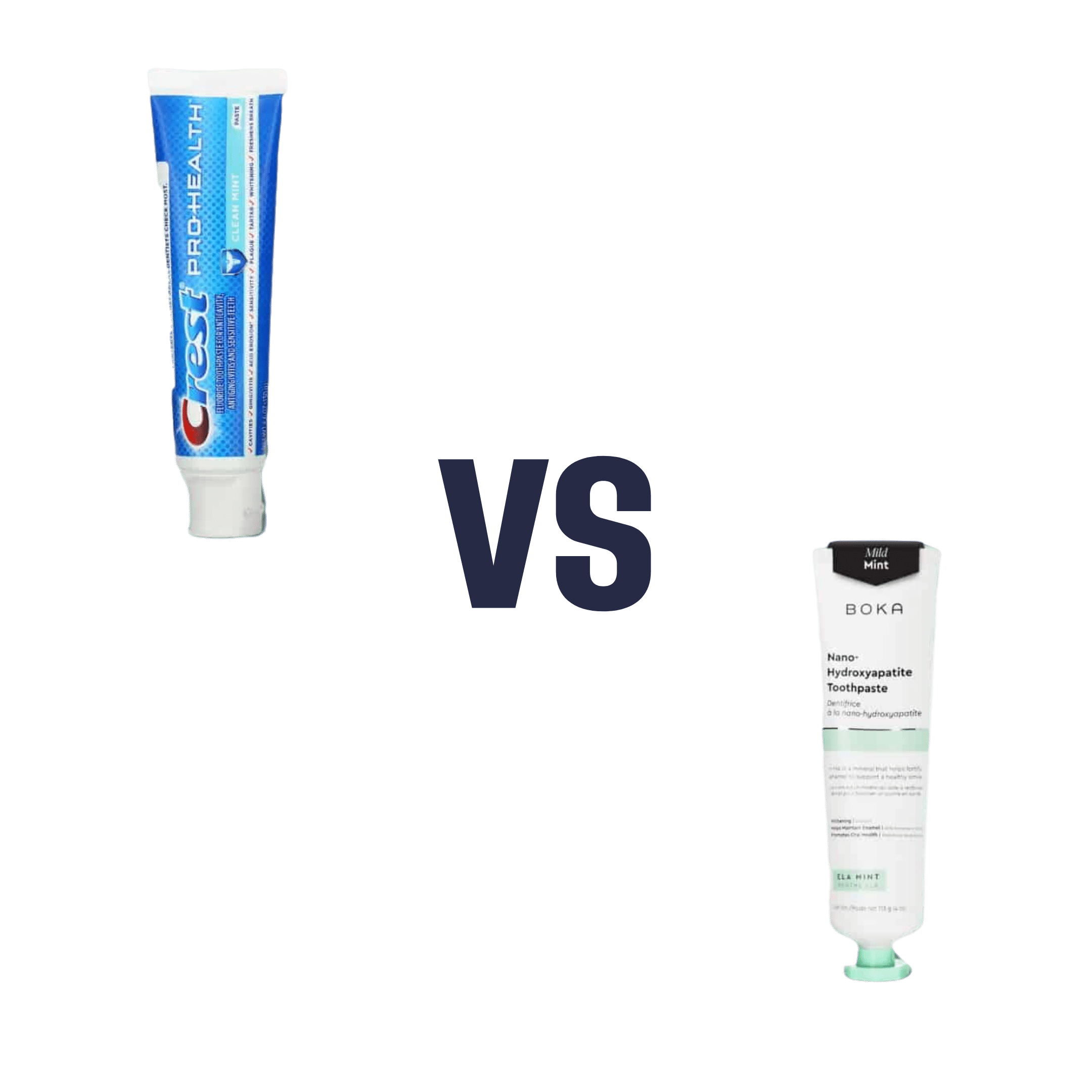
Fluoride Toothpaste vs Non-Fluoride Toothpaste – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fluoride toothpaste to non-fluoride toothpaste, we picked the fluoride.
Why?
Fluoride is indeed toxic; that’s why it’s in toothpaste (to kill things; namely, bacteria whose waste products would harm our teeth). However, we are much bigger than those bacteria.
Given the amount of fluoride in toothpaste (usually under 1mg per strip of toothpaste to cover a toothbrush head), the amount that people swallow unintentionally (about 1/20th of that, so about 0.1mg daily if brushing teeth twice daily), and the toxicity level of fluoride (32–64mg/kg), then even if we take the most dangerous ends of all those numbers (and an average body size), to suffer ill effects from fluoride due to brushing your teeth, would require that you brush your teeth more than 23,000 times per day.
Alternatively, if you were to ravenously eat the toothpaste instead of spitting it out, you’d only need to brush your teeth a little over 1,000 times per day.
All the same, please don’t eat toothpaste; that’s not the message here.
However! In head-to-head tests, fluoride toothpaste has almost always beaten non-fluoride toothpaste.
Almost? Yes, almost: hydroxyapatite performed equally in one study, but that’s not usually an option on as many supermarket shelves.
We found some on Amazon, though, which is the one we used for today’s head-to-head. Here it is:
However, before you rush to buy it, do be aware that the toxicity of hydroxyapatite appears to be about twice that of fluoride:
Scientific Committee on Consumer Safety Opinion On Hydroxyapatite (Nano)
…which is still very safe (you’d need to brush your teeth, and eat all the toothpaste, about 500 times per day, to get to toxic levels, if we run with the same numbers we discussed before. Again, please do not do that, though).
But, since the science so far suggests it’s about twice as toxic as fluoride, then regardless of that still being very safe, the fluoride is obviously (by the same metric) twice as safe, hence picking the fluoride.
Want more options?
Check out our previous main feature:
Less Common Oral Hygiene Options
(the above article also links back to our discussion of different toothpastes and mouthwashes, by the way)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: