Millet vs Rye – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing millet to rye, we picked the rye.
Why?
In terms of macros, they’re about equal on protein, and rye has more carbs and fiber, the ratio of which give it the lower glycemic index, so we say rye wins this category.
In the category of vitamins, millet has more of vitamins B1, B2, B6, and B9, while rye has more of vitamins A, B5, E, and K. Notionally, that’s a 4:4 tie, though rye’s margins of difference are an order of magnitude greater, so we say rye takes a marginal victory on this one.
When it comes to minerals, there’s nothing to debate here: millet has more copper, while rye has more calcium, manganese, phosphorus, potassium, selenium, and zinc. An easy win for rye on this one.
Adding up the sections gives the overall win to rye, but there is one other thing worth mentioning: millet is naturally gluten-free, but rye is not, so if you are avoiding gluten for any reason, you’ll want to pick the millet in this case.
See also: Gluten: What’s The Truth?
Aside from that, by all means enjoy either or both, in moderation! Diversity is good.
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The first pig kidney has been transplanted into a living person. But we’re still a long way from solving organ shortages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a world first, we heard last week that US surgeons had transplanted a kidney from a gene-edited pig into a living human. News reports said the procedure was a breakthrough in xenotransplantation – when an organ, cells or tissues are transplanted from one species to another. https://www.youtube.com/embed/cisOFfBPZk0?wmode=transparent&start=0 The world’s first transplant of a gene-edited pig kidney into a live human was announced last week.
Champions of xenotransplantation regard it as the solution to organ shortages across the world. In December 2023, 1,445 people in Australia were on the waiting list for donor kidneys. In the United States, more than 89,000 are waiting for kidneys.
One biotech CEO says gene-edited pigs promise “an unlimited supply of transplantable organs”.
Not, everyone, though, is convinced transplanting animal organs into humans is really the answer to organ shortages, or even if it’s right to use organs from other animals this way.
There are two critical barriers to the procedure’s success: organ rejection and the transmission of animal viruses to recipients.
But in the past decade, a new platform and technique known as CRISPR/Cas9 – often shortened to CRISPR – has promised to mitigate these issues.
What is CRISPR?
CRISPR gene editing takes advantage of a system already found in nature. CRISPR’s “genetic scissors” evolved in bacteria and other microbes to help them fend off viruses. Their cellular machinery allows them to integrate and ultimately destroy viral DNA by cutting it.
In 2012, two teams of scientists discovered how to harness this bacterial immune system. This is made up of repeating arrays of DNA and associated proteins, known as “Cas” (CRISPR-associated) proteins.
When they used a particular Cas protein (Cas9) with a “guide RNA” made up of a singular molecule, they found they could program the CRISPR/Cas9 complex to break and repair DNA at precise locations as they desired. The system could even “knock in” new genes at the repair site.
In 2020, the two scientists leading these teams were awarded a Nobel prize for their work.
In the case of the latest xenotransplantation, CRISPR technology was used to edit 69 genes in the donor pig to inactivate viral genes, “humanise” the pig with human genes, and knock out harmful pig genes. https://www.youtube.com/embed/UKbrwPL3wXE?wmode=transparent&start=0 How does CRISPR work?
A busy time for gene-edited xenotransplantation
While CRISPR editing has brought new hope to the possibility of xenotransplantation, even recent trials show great caution is still warranted.
In 2022 and 2023, two patients with terminal heart diseases, who were ineligible for traditional heart transplants, were granted regulatory permission to receive a gene-edited pig heart. These pig hearts had ten genome edits to make them more suitable for transplanting into humans. However, both patients died within several weeks of the procedures.
Earlier this month, we heard a team of surgeons in China transplanted a gene-edited pig liver into a clinically dead man (with family consent). The liver functioned well up until the ten-day limit of the trial.
How is this latest example different?
The gene-edited pig kidney was transplanted into a relatively young, living, legally competent and consenting adult.
The total number of gene edits edits made to the donor pig is very high. The researchers report making 69 edits to inactivate viral genes, “humanise” the pig with human genes, and to knockout harmful pig genes.
Clearly, the race to transform these organs into viable products for transplantation is ramping up.
From biotech dream to clinical reality
Only a few months ago, CRISPR gene editing made its debut in mainstream medicine.
In November, drug regulators in the United Kingdom and US approved the world’s first CRISPR-based genome-editing therapy for human use – a treatment for life-threatening forms of sickle-cell disease.
The treatment, known as Casgevy, uses CRISPR/Cas-9 to edit the patient’s own blood (bone-marrow) stem cells. By disrupting the unhealthy gene that gives red blood cells their “sickle” shape, the aim is to produce red blood cells with a healthy spherical shape.
Although the treatment uses the patient’s own cells, the same underlying principle applies to recent clinical xenotransplants: unsuitable cellular materials may be edited to make them therapeutically beneficial in the patient.
CRISPR technology is aiming to restore diseased red blood cells to their healthy round shape. Sebastian Kaulitzki/Shutterstock We’ll be talking more about gene-editing
Medicine and gene technology regulators are increasingly asked to approve new experimental trials using gene editing and CRISPR.
However, neither xenotransplantation nor the therapeutic applications of this technology lead to changes to the genome that can be inherited.
For this to occur, CRISPR edits would need to be applied to the cells at the earliest stages of their life, such as to early-stage embryonic cells in vitro (in the lab).
In Australia, intentionally creating heritable alterations to the human genome is a criminal offence carrying 15 years’ imprisonment.
No jurisdiction in the world has laws that expressly permits heritable human genome editing. However, some countries lack specific regulations about the procedure.
Is this the future?
Even without creating inheritable gene changes, however, xenotransplantation using CRISPR is in its infancy.
For all the promise of the headlines, there is not yet one example of a stable xenotransplantation in a living human lasting beyond seven months.
While authorisation for this recent US transplant has been granted under the so-called “compassionate use” exemption, conventional clinical trials of pig-human xenotransplantation have yet to commence.
But the prospect of such trials would likely require significant improvements in current outcomes to gain regulatory approval in the US or elsewhere.
By the same token, regulatory approval of any “off-the-shelf” xenotransplantation organs, including gene-edited kidneys, would seem some way off.
Christopher Rudge, Law lecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
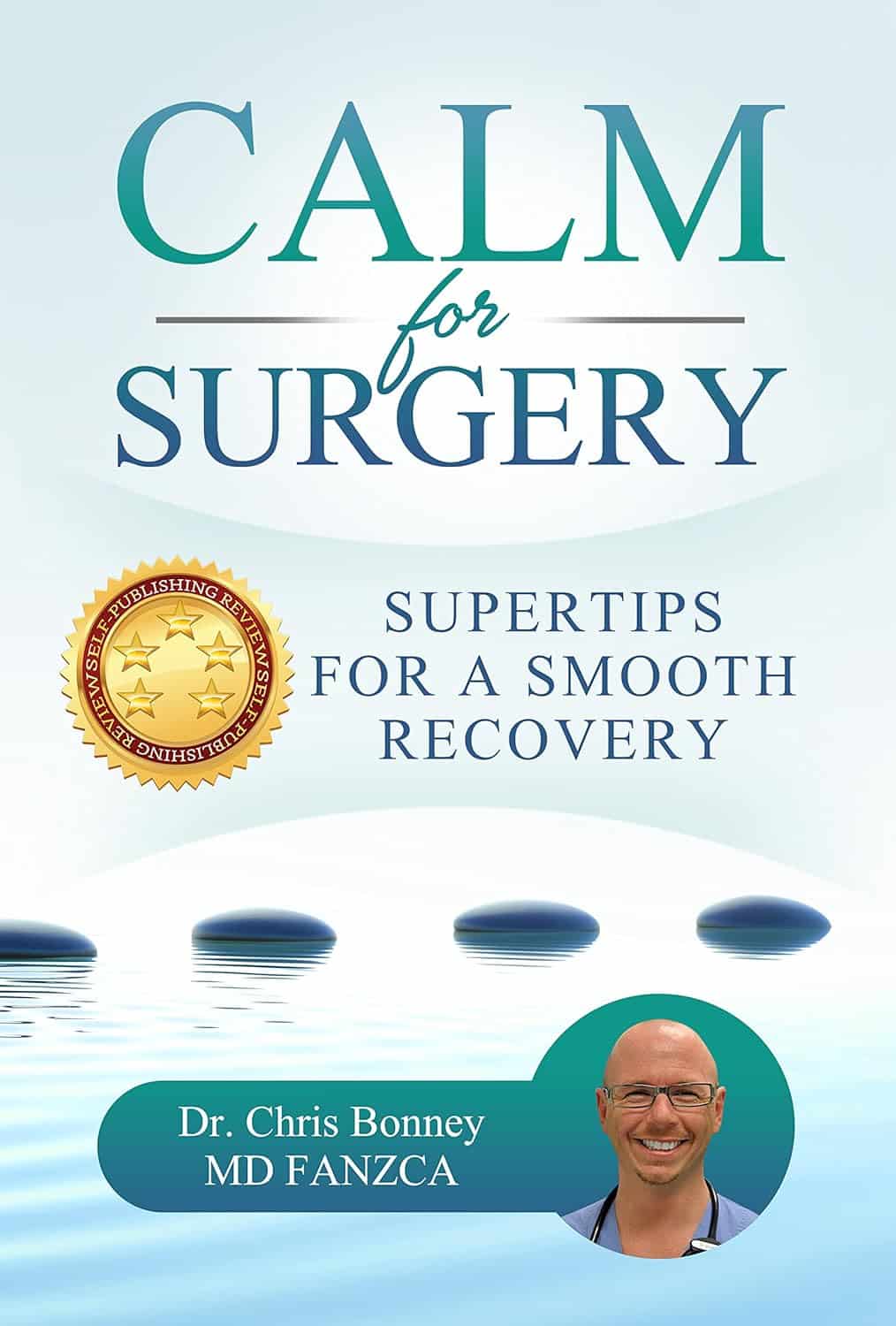
Calm For Surgery – by Dr Chris Bonney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As a general rule of thumb, nobody likes having surgery. We may like the results of the surgery, we may like having the surgery done and behind us, but surgery itself is not most people’s idea of fun, and honestly, the recovery period afterwards can be a pain in every sense of the word.
Dr. Chris Bonney, an anesthesiologist, gives us the industry-secrets low-down, and is the voice of experience when it comes to the things to know about and/or prepare in advance—the little things that make a world of difference to your in-hospital experience and afterwards.
Think of it like “frequent flyer traveller tips” but for surgeries, whereupon knowing a given tip can mean the difference between deeply traumatic suffering and merely not being at your usual best. We think that’s worth it.
Share This Post
-
Steps For Keeping Your Feet A Healthy Foundation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Important Steps For Good Health
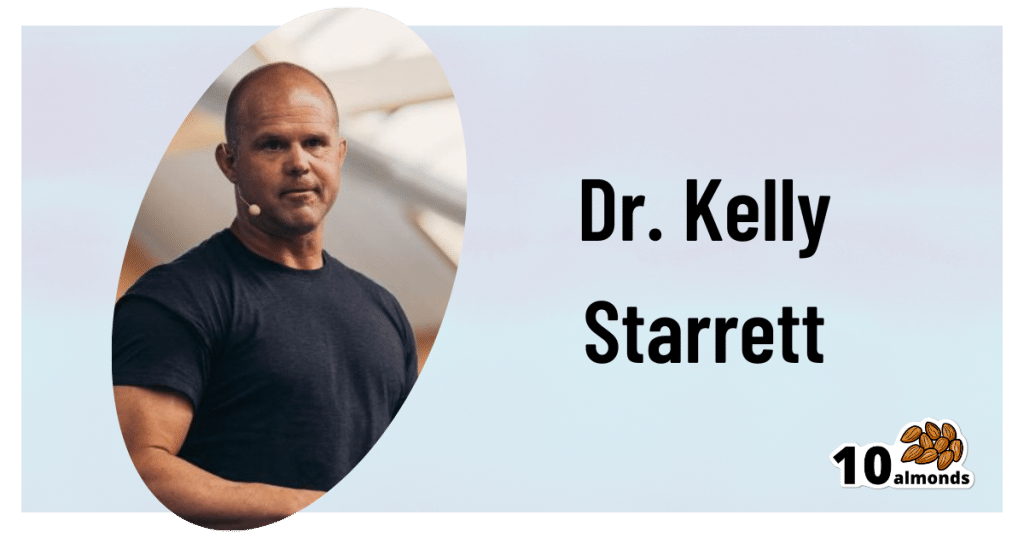
This is Dr. Kelly Starrett. He’s a physiotherapist, author, speaker, trainer. He has been described as a “celebrity” and “founding father” of CrossFit. He mostly speaks and writes about mobility in general; today we’re going to be looking at what he has to say specifically about our feet.
A strong foundation
“An army marches on its stomach”, Napoleon famously wrote.
More prosaically: an army marches on its feet, and good foot-care is a top priority for soldiers—indeed, in some militaries, even so much as negligently getting blisters is a military offense.
Most of us are not soldiers, but there’s a lesson to be learned here:
Your feet are the foundation for much of the rest of your health and effectiveness.
KISS for feet
No, not like that.
Rather: “Keep It Simple, Stupid”
Dr. Starrett is not only a big fan of not overcomplicating things, but also, he tells us how overcomplicating things can actively cause problems. When it comes to footwear, for example, he advises:
❝When you wear shoes, wear the flat kind. If you’re walking the red carpet on Oscar night, fine, go ahead and wear a shoe with a heel. Once in a while is okay.
But most of the time, you should wear shoes that are flat and won’t throw your biological movement hardware into disarray.
When you have to wear shoes, whether it’s running shoes, work shoes, or combat boots, buy the flat kind, also known as “zero drop”—meaning that the heel is not raised above the forefoot (at all).
What you want to avoid, or wean yourself away from, are shoes with the heels raised higher off the ground than the forefeet.❞
Of course, going barefoot is great for this, but may not be an option for all of us when out and about. And in the home, going barefoot (or shod in just socks) will only confer health benefits if we’re actually on our feet! So… How much time do you spend on your feet at home?
Allow your feet to move like feet
By evolution, the human body is built for movement—especially walking and running. That came with moving away from hanging around in trees for fruit, to hunting and gathering between different areas of the savannah. Today, our hunting and gathering may be done at the local grocery store, but we still need to keep our mobility, especially when it comes to our feet.
Now comes the flat footwear you don’t want: flip-flops and similar
If we wear flip-flops, or other slippers or shoes that hold onto our feet only at the front, we’re no longer walking like we’re supposed to. Instead of being the elegant product of so much evolution, we’re now walking like those AT-AT walkers in Star Wars, you know, the ones that fell over so easily?
Our feet need to be able to tilt naturally while walking/running, without our footwear coming off.
Golden rule for this: if you can’t run in them, you shouldn’t be walking in them
Exception: if for example you need something on your feet for a minute or two in the shower at the gym/pool, flip-flops are fine. But anything more than that, and you want something better.
Watch your step
There’s a lot here that’s beyond the scope of what we can include in this short newsletter, but:
If we stand or walk or run incorrectly, we’re doing gradual continual damage to our feet and ankles (potentially also our knees and hips, which problems in turn have a knock-on effect for our spine, and you get the idea—this is Bad™)
Some general pointers for keeping things in good order include:
- Your weight should be mostly on the balls of your feet, not your heels
- Your feet should be pretty much parallel, not turned out or in
- When standing, your center of gravity should be balanced between heel and forefoot
Quick tip for accomplishing this last one: Stand comfortably, your feet parallel, shoulder-width apart. Now, go up on your tip-toes. When you’ve done so, note where your spine is, and keep it there (apart from in its up-down axis) when you slowly go back to having your feet flat on the ground, so it’s as though your spine is sliding down a pole that’s fixed in place.
If you do this right, your center of gravity will now be perfectly aligned with where it’s supposed to be. It might feel a bit weird at first, but you’ll get used to it, and can always reset it whenever you want/need, by repeating the exercise.
If you’d like to know more from Dr. Starrett, you can check out his website here 🙂
Share This Post
Related Posts
-
The Other Alzheimer’s Risk Factor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The usually-listed 7 known risk factors of dementia (in general, not just Alzheimer’s) do not include today’s item. For a recap, those were:
The 7 Known Risk Factors For Dementia
The bonus risk factor
This idea is not completely novel; it’s been known for a while that traumatic brain injury (TBI) can increase the risk of dementia, but it has generally been chalked up to “if you damage an organ, then that organ does not function so well afterwards”.
However, in the case of Alzheimer’s, it seems there’s something deeper at play. Specifically, a study that found…
❝…traumatic brain injury alters the small vessels in the brain, resulting in an accumulation of amyloid beta—a hallmark of Alzheimer’s disease.
The findings suggest that vascular dysfunction could be an early driver in neurodegenerative disorders rather than being caused by neuronal damage.❞
This association held true even in quite young patients!
The study from Sweden looked at brain tissue from TBI patients (who had had to have brain tissue removed for medical reasons due to bleeding and swelling), and found that the (traumatic) changes to the vascular smooth muscle cells were associated with increased aggregation of amyloid-β.
In terms of establishing cause and effect: since it could be safely concluded the amyloid-β had not caused the TBI (which all had external explanations such as “car crash” or such), it can be deduced that almost* certainly the TBI caused the amyloid-β aggregation.
*because little to nothing in science is every truly certain. As in life in general, really; the difference is that scientists admit it!
You may be wondering: what was the control? It would be a very generous group of citizens indeed who would volunteer bits of their brains that hadn’t needed removing. However, the answer is that the control brain bits came from a biobank, and were from uninjured patients with no history of TBI or neurodegenerative disorders, and who had died from systemic, unrelated causes. Having been dead for a matter of hours, and the fixation time for the brain bits from the living people taking long enough that everybody’s brain bits had been out of their respective living bodies for a similar length of time, this was deemed an acceptable, if imperfect, control.
You can read the study in its entirety here; it is fascinating:
The practical take-away
The practical take-away, of course, is: look after your brain
Not just in the sense of eat fiber, get healthy fats, move more, get good sleep, stay intellectually stimulated, etc*, but also in the sense of “keep your brain physically safe”.
Now, you may think that you already try not to get into car crashes, and perhaps you do not compete in contact sports, but do be aware that one of the leading causes of TBI in older people is, ignominiously, falling down.
And if you think “that only happens to older/other people”, then be aware: there’s a first time for everything and you are not immune. With that in mind, do check out:
Fall Special! ← the seasonal title notwithstanding, this is about not falling down in the first place, and being less injurable if you do fall down
*This was a modest and vague list for brevity’s sake, so for much more detail, enjoy:
How To Reduce Your Alzheimer’s Risk ← this is rather more comprehensive
Want to know more?
Here you can read about the largest study of its kind into lifestyle factors and Alzheimer’s disease:
Alzheimer’s Causative Factors To Avoid ← the methods and conclusions of Dr. David Snowdon’s famous “Nun Study”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Early Detection May Help Kentucky Tamp Down Its Lung Cancer Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anthony Stumbo’s heart sank after the doctor shared his mother’s chest X-ray.
“I remember that drive home, bringing her back home, and we basically cried,” said the internal medicine physician, who had started practicing in eastern Kentucky near his childhood home shortly before his mother began feeling ill. “Nobody wants to get told they’ve got inoperable lung cancer. I cried because I knew what this meant for her.”
Now Stumbo, whose mother died the following year, in 1997, is among a group of Kentucky clinicians and researchers determined to rewrite the script for other families by promoting training and boosting awareness about early detection in the state with the highest lung cancer death rate. For the past decade, Kentucky researchers have promoted lung cancer screening, first recommended by the U.S. Preventive Services Task Force in 2013. These days the Bluegrass State screens more residents who are at high risk of developing lung cancer than any state except Massachusetts — 10.6% of eligible residents in 2022, more than double the national rate of 4.5% — according to the most recent American Lung Association analysis.
The effort has been driven by a research initiative called the Kentucky LEADS (Lung Cancer Education, Awareness, Detection, and Survivorship) Collaborative, which in 2014 launched to improve screening and prevention, to identify more tumors earlier, when survival odds are far better. The group has worked with clinicians and hospital administrators statewide to boost screening rates both in urban areas and regions far removed from academic medical centers, such as rural Appalachia. But, a decade into the program, the researchers face an ongoing challenge as they encourage more people to get tested, namely the fear and stigma that swirl around smoking and lung cancer.
Lung cancer kills more Americans than any other malignancy, and the death rates are worst in a swath of states including Kentucky and its neighbors Tennessee and West Virginia, and stretching south to Mississippi and Louisiana, according to data from the Centers for Disease Control and Prevention.
It’s a bit early to see the impact on lung cancer deaths because people may still live for years with a malignancy, LEADS researchers said. Plus, treatment improvements and other factors may also help reduce death rates along with increased screening. Still, data already shows that more cancers in Kentucky are being detected before they become advanced, and thus more difficult to treat, they said. Of total lung cancer cases statewide, the percentage of advanced cases — defined as cancers that had spread to the lymph nodes or beyond — hovered near 81% between 2000 and 2014, according to Kentucky Cancer Registry data. By 2020, that number had declined to 72%, according to the most recent data available.
“We are changing the story of families. And there is hope where there has not been hope before,” said Jennifer Knight, a LEADS principal investigator.
Older adults in their 60s and 70s can hold a particularly bleak view of their mortality odds, given what their loved ones experienced before screening became available, said Ashley Shemwell, a nurse navigator for the lung cancer screening program at Owensboro Health, a nonprofit health system that serves Kentucky and Indiana.
“A lot of them will say, ‘It doesn’t matter if I get lung cancer or not because it’s going to kill me. So I don’t want to know,’” said Shemwell. “With that generation, they saw a lot of lung cancers and a lot of deaths. And it was terrible deaths because they were stage 4 lung cancers.” But she reminds them that lung cancer is much more treatable if caught before it spreads.
The collaborative works with several partners, including the University of Kentucky, the University of Louisville, and GO2 for Lung Cancer, and has received grant funding from the Bristol Myers Squibb Foundation. Leaders have provided training and other support to 10 hospital-based screening programs, including a stipend to pay for resources such as educational materials or a nurse navigator, Knight said. In 2022, state lawmakers established a statewide lung cancer screening program based in part on the group’s work.
Jacob Sands, a lung cancer physician at Boston’s Dana-Farber Cancer Institute, credits the LEADS collaborative with encouraging patients to return for annual screening and follow-up testing for any suspicious nodules. “What the Kentucky LEADS program is doing is fantastic, and that is how you really move the needle in implementing lung screening on a larger scale,” said Sands, who isn’t affiliated with the Kentucky program and serves as a volunteer spokesperson for the American Lung Association.
In 2014, Kentucky expanded Medicaid, increasing the number of lower-income people who qualified for lung cancer screening and any related treatment. Adults 50 to 80 years old are advised to get a CT scan every year if they have accumulated at least 20 pack years and still smoke or have quit within the past 15 years, according to the latest task force recommendation, which widened the pool of eligible adults. (To calculate pack years, multiply the packs of cigarettes smoked daily by years of smoking.) The lung association offers an online quiz, called “Saved By The Scan,” to figure out likely eligibility for insurance coverage.
Half of U.S. patients aren’t diagnosed until their cancer has spread beyond the lungs and lymph nodes to elsewhere in the body. By then, the five-year survival rate is 8.2%.
But regular screening boosts those odds. When a CT scan detects lung cancer early, patients have an 81% chance of living at least 20 years, according to data published in November in the journal Radiology.
Some adults, like Lisa Ayers, didn’t realize lung cancer screening was an option. Her family doctor recommended a CT scan last year after she reported breathing difficulties. Ayers, who lives in Ohio near the Kentucky border, got screened at UK King’s Daughters, a hospital in far eastern Kentucky. The scan didn’t take much time, and she didn’t have to undress, the 57-year-old said. “It took me longer to park,” she quipped.
She was diagnosed with a lung carcinoid tumor, a type of neuroendocrine cancer that can grow in various parts of the body. Her cancer was considered too risky for surgery, Ayers said. A biopsy showed the cancer was slow-growing, and her doctors said they would monitor it closely.
Ayers, a lifelong smoker, recalled her doctor said that her type of cancer isn’t typically linked to smoking. But she quit anyway, feeling like she’d been given a second chance to avoid developing a smoking-related cancer. “It was a big wake-up call for me.”
Adults with a smoking history often report being treated poorly by medical professionals, said Jamie Studts, a health psychologist and a LEADS principal investigator, who has been involved with the research from the start. The goal is to avoid stigmatizing people and instead to build rapport, meeting them where they are that day, he said.
“If someone tells us that they’re not ready to quit smoking but they want to have lung cancer screening, awesome; we’d love to help,” Studts said. “You know what? You actually develop a relationship with an individual by accepting, ‘No.’”
Nationally, screening rates vary widely. Massachusetts reaches 11.9% of eligible residents, while California ranks last, screening just 0.7%, according to the lung association analysis.
That data likely doesn’t capture all California screenings, as it may not include CT scans done through large managed care organizations, said Raquel Arias, a Los Angeles-based associate director of state partnerships at the American Cancer Society. She cited other 2022 data for California, looking at lung cancer screening for eligible Medicare fee-for-service patients, which found a screening rate of 1%-2% in that population.
But, Arias said, the state’s effort is “nowhere near what it needs to be.”
The low smoking rate in California, along with its image as a healthy state, “seems to have come with the unintended consequence of further stigmatizing people who smoke,” said Arias, citing one of the findings from a 2022 report looking at lung cancer screening barriers. For instance, eligible patients may be reluctant to share prior smoking habits with their health provider, she said.
Meanwhile, Kentucky screening efforts progress, scan by scan.
At Appalachian Regional Healthcare, 3,071 patients were screened in 2023, compared with 372 in 2017. “We’re just scratching the surface of the potential lives that we can have an effect on,” said Stumbo, a lung cancer screening champion at the health system, which includes 14 hospitals, most located in eastern Kentucky.
The doctor hasn’t shed his own grief about what his family missed after his mother died at age 51, long before annual screening was recommended. “Knowing that my children were born, and never knowing their grandmother,” he said, “just how sad is that?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Older Men’s Connections Often Wither When They’re on Their Own
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At age 66, South Carolina physician Paul Rousseau decided to retire after tending for decades to the suffering of people who were seriously ill or dying. It was a difficult and emotionally fraught transition.
“I didn’t know what I was going to do, where I was going to go,” he told me, describing a period of crisis that began in 2017.
Seeking a change of venue, Rousseau moved to the mountains of North Carolina, the start of an extended period of wandering. Soon, a sense of emptiness enveloped him. He had no friends or hobbies — his work as a doctor had been all-consuming. Former colleagues didn’t get in touch, nor did he reach out.
His wife had passed away after a painful illness a decade earlier. Rousseau was estranged from one adult daughter and in only occasional contact with another. His isolation mounted as his three dogs, his most reliable companions, died.
Rousseau was completely alone — without friends, family, or a professional identity — and overcome by a sense of loss.
“I was a somewhat distinguished physician with a 60-page resume,” Rousseau, now 73, wrote in the Journal of the American Geriatrics Society in May. “Now, I’m ‘no one,’ a retired, forgotten old man who dithers away the days.”
In some ways, older men living alone are disadvantaged compared with older women in similar circumstances. Research shows that men tend to have fewer friends than women and be less inclined to make new friends. Often, they’re reluctant to ask for help.
“Men have a harder time being connected and reaching out,” said Robert Waldinger, a psychiatrist who directs the Harvard Study of Adult Development, which has traced the arc of hundreds of men’s lives over a span of more than eight decades. The men in the study who fared the worst, Waldinger said, “didn’t have friendships and things they were interested in — and couldn’t find them.” He recommends that men invest in their “social fitness” in addition to their physical fitness to ensure they have satisfying social interactions.
Slightly more than 1 in every 5 men ages 65 to 74 live alone, according to 2022 Census Bureau data. That rises to nearly 1 in 4 for those 75 or older. Nearly 40% of these men are divorced, 31% are widowed, and 21% never married.
That’s a significant change from 2000, when only 1 in 6 older men lived by themselves. Longer life spans for men and rising divorce rates are contributing to the trend. It’s difficult to find information about this group — which is dwarfed by the number of women who live alone — because it hasn’t been studied in depth. But psychologists and psychiatrists say these older men can be quite vulnerable.
When men are widowed, their health and well-being tend to decline more than women’s.
“Older men have a tendency to ruminate, to get into our heads with worries and fears and to feel more lonely and isolated,” said Jed Diamond, 80, a therapist and the author of “Surviving Male Menopause” and “The Irritable Male Syndrome.”
Add in the decline of civic institutions where men used to congregate — think of the Elks or the Shriners — and older men’s reduced ability to participate in athletic activities, and the result is a lack of stimulation and the loss of a sense of belonging.
Depression can ensue, fueling excessive alcohol use, accidents, or, in the most extreme cases, suicide. Of all age groups in the United States, men over age 75 have the highest suicide rate, by far.
For this column, I spoke at length to several older men who live alone. All but two (who’d been divorced) were widowed. Their experiences don’t represent all men who live alone. But still, they’re revealing.
The first person I called was Art Koff, 88, of Chicago, a longtime marketing executive I’d known for several years. When I reached out in January, I learned that Koff’s wife, Norma, had died the year before, leaving him hobbled by grief. Uninterested in eating and beset by unremitting loneliness, Koff lost 45 pounds.
“I’ve had a long and wonderful life, and I have lots of family and lots of friends who are terrific,” Koff told me. But now, he said, “nothing is of interest to me any longer.”
“I’m not happy living this life,” he said.
Nine days later, I learned that Koff had died. His nephew, Alexander Koff, said he had passed out and was gone within a day. The death certificate cited “end stage protein calorie malnutrition” as the cause.
The transition from being coupled to being single can be profoundly disorienting for older men. Lodovico Balducci, 80, was married to his wife, Claudia, for 52 years before she died in October 2023. Balducci, a renowned physician known as the “patriarch of geriatric oncology,” wrote about his emotional reaction in the Journal of the American Geriatrics Society, likening Claudia’s death to an “amputation.”
“I find myself talking to her all the time, most of the time in my head,” Balducci told me in a phone conversation. When I asked him whom he confides in, he admitted, “Maybe I don’t have any close friends.”
Disoriented and disorganized since Claudia died, he said his “anxiety has exploded.”
We spoke in late February. Two weeks later, Balducci moved from Tampa to New Orleans, to be near his son and daughter-in-law and their two teenagers.
“I am planning to help as much as possible with my grandchildren,” he said. “Life has to go on.”
Verne Ostrander, a carpenter in the small town of Willits, California, about 140 miles north of San Francisco, was reflective when I spoke with him, also in late February. His second wife, Cindy Morninglight, died four years ago after a long battle with cancer.
“Here I am, almost 80 years old — alone,” Ostrander said. “Who would have guessed?”
When Ostrander isn’t painting watercolors, composing music, or playing guitar, “I fall into this lonely state, and I cry quite a bit,” he told me. “I don’t ignore those feelings. I let myself feel them. It’s like therapy.”
Ostrander has lived in Willits for nearly 50 years and belongs to a men’s group and a couples’ group that’s been meeting for 20 years. He’s in remarkably good health and in close touch with his three adult children, who live within easy driving distance.
“The hard part of living alone is missing Cindy,” he told me. “The good part is the freedom to do whatever I want. My goal is to live another 20 to 30 years and become a better artist and get to know my kids when they get older.”
The Rev. Johnny Walker, 76, lives in a low-income apartment building in a financially challenged neighborhood on Chicago’s West Side. Twice divorced, he’s been on his own for five years. He, too, has close family connections. At least one of his several children and grandchildren checks in on him every day.
Walker says he had a life-changing religious conversion in 1993. Since then, he has depended on his faith and his church for a sense of meaning and community.
“It’s not hard being alone,” Walker said when I asked whether he was lonely. “I accept Christ in my life, and he said that he would never leave us or forsake us. When I wake up in the morning, that’s a new blessing. I just thank God that he has brought me this far.”
Waldinger recommended that men “make an effort every day to be in touch with people. Find what you love — golf, gardening, birdwatching, pickleball, working on a political campaign — and pursue it,” he said. “Put yourself in a situation where you’re going to see the same people over and over again. Because that’s the most natural way conversations get struck up and friendships start to develop.”
Rousseau, the retired South Carolina doctor, said he doesn’t think about the future much. After feeling lost for several years, he moved across the country to Jackson, Wyoming, in the summer of 2023. He embraced solitude, choosing a remarkably isolated spot to live — a 150-square-foot cabin with no running water and no bathroom, surrounded by 25,000 undeveloped acres of public and privately owned land.
“Yes, I’m still lonely, but the nature and the beauty here totally changed me and focused me on what’s really important,” he told me, describing a feeling of redemption in his solitude.
Rousseau realizes that the death of his parents and a very close friend in his childhood left him with a sense of loss that he kept at bay for most of his life. Now, he said, rather than denying his vulnerability, he’s trying to live with it. “There’s only so long you can put off dealing with all the things you’re trying to escape from.”
It’s not the life he envisioned, but it’s one that fits him, Rousseau said. He stays busy with volunteer activities — cleaning tanks and running tours at Jackson’s fish hatchery, serving as a part-time park ranger, and maintaining trails in nearby national forests. Those activities put him in touch with other people, mostly strangers, only intermittently.
What will happen to him when this way of living is no longer possible?
“I wish I had an answer, but I don’t,” Rousseau said. “I don’t see my daughters taking care of me. As far as someone else, I don’t think there’s anyone else who’s going to help me.”
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit http://kffhealthnews.org/columnists to submit your requests or tips.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: