Mental Health Courts Can Struggle to Fulfill Decades-Old Promise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GAINESVILLE, Ga. — In early December, Donald Brown stood nervously in the Hall County Courthouse, concerned he’d be sent back to jail.
The 55-year-old struggles with depression, addiction, and suicidal thoughts. He worried a judge would terminate him from a special diversion program meant to keep people with mental illness from being incarcerated. He was failing to keep up with the program’s onerous work and community service requirements.
“I’m kind of scared. I feel kind of defeated,” Brown said.
Last year, Brown threatened to take his life with a gun and his family called 911 seeking help, he said. The police arrived, and Brown was arrested and charged with a felony of firearm possession.
After months in jail, Brown was offered access to the Health Empowerment Linkage and Possibilities, or HELP, Court. If he pleaded guilty, he’d be connected to services and avoid prison time. But if he didn’t complete the program, he’d possibly face incarceration.
“It’s almost like coercion,” Brown said. “‘Here, sign these papers and get out of jail.’ I feel like I could have been dealt with a lot better.”
Advocates, attorneys, clinicians, and researchers said courts such as the one Brown is navigating can struggle to live up to their promise. The diversion programs, they said, are often expensive and resource-intensive, and serve fewer than 1% of the more than 2 million people who have a serious mental illness and are booked into U.S. jails each year.
People can feel pressured to take plea deals and enter the courts, seeing the programs as the only route to get care or avoid prison time. The courts are selective, due in part to political pressures on elected judges and prosecutors. Participants must often meet strict requirements that critics say aren’t treatment-focused, such as regular hearings and drug screenings.
And there is a lack of conclusive evidence on whether the courts help participants long-term. Some legal experts, like Lea Johnston, a professor of law at the University of Florida, worry the programs distract from more meaningful investments in mental health resources.
Jails and prisons are not the place for individuals with mental disorders, she said. “But I’m also not sure that mental health court is the solution.”
The country’s first mental health court was established in Broward County, Florida, in 1997, “as a way to promote recovery and mental health wellness and avoid criminalizing mental health problems.” The model was replicated with millions in funding from such federal agencies as the Substance Abuse and Mental Health Services Administration and the Department of Justice.
More than 650 adult and juvenile mental health courts were operational as of 2022, according to the National Treatment Court Resource Center. There’s no set way to run them. Generally, participants receive treatment plans and get linked to services. Judges and mental health clinicians oversee their progress.
Researchers from the center found little evidence that the courts improve participants’ mental health or keep them out of the criminal justice system. “Few studies … assess longer-term impacts” of the programs “beyond one year after program exit,” said a 2022 policy brief on mental health courts.
The courts work best when paired with investments in services such as clinical treatment, recovery programs, and housing and employment opportunities, said Kristen DeVall, the center’s co-director.
“If all of these other supports aren’t invested in, then it’s kind of a wash,” she said.
The courts should be seen as “one intervention in that larger system,” DeVall said, not “the only resource to serve folks with mental health needs” who get caught up in the criminal justice system.
Resource limitations can also increase the pressures to apply for mental health court programs, said Lisa M. Wayne, executive director of the National Association of Criminal Defense Lawyers. People seeking help might not feel they have alternatives.
“It’s not going to be people who can afford mental health intervention. It’s poor people, marginalized folks,” she said.
Other court skeptics wonder about the larger costs of the programs.
In a study of a mental health court in Pennsylvania, Johnston and a University of Florida colleague found participants were sentenced to longer time under government supervision than if they’d gone through the regular criminal justice system.
“The bigger problem is they’re taking attention away from more important solutions that we should be investing in, like community mental health care,” Johnston said.
When Melissa Vergara’s oldest son, Mychael Difrancisco, was arrested on felony gun charges in Queens in May 2021, she thought he would be an ideal candidate for the New York City borough’s mental health court because of his diagnosis of autism spectrum disorder and other behavioral health conditions.
She estimated she spent tens of thousands of dollars to prepare Difrancisco’s case for consideration. Meanwhile, her son sat in jail on Rikers Island, where she said he was assaulted multiple times and had to get half a finger amputated after it was caught in a cell door.
In the end, his case was denied diversion into mental health court. Difrancisco, 22, is serving a prison sentence that could be as long as four years and six months.
“There’s no real urgency to help people with mental health struggles,” Vergara said.
Critics worry such high bars to entry can lead the programs to exclude people who could benefit the most. Some courts don’t allow those accused of violent or sexual crimes to participate. Prosecutors and judges can face pressure from constituents that may lead them to block individuals accused of high-profile offenses.
And judges often aren’t trained to make decisions about participants’ care, said Raji Edayathumangalam, senior policy social worker with New York County Defender Services.
“It’s inappropriate,” she said. “We’re all licensed to practice in our different professions for a reason. I can’t show up to do a hernia operation just because I read about it or sat next to a hernia surgeon.”
Mental health courts can be overly focused on requirements such as drug testing, medication compliance, and completing workbook assignments, rather than progress toward recovery and clinical improvement, Edayathumangalam said.
Completing the programs can leave some participants with clean criminal records. But failing to meet a program’s requirements can trigger penalties — including incarceration.
During a recent hearing in the Clayton County Behavioral Health Accountability Court in suburban Atlanta, one woman left the courtroom in tears when Judge Shana Rooks Malone ordered her to report to jail for a seven-day stay for “being dishonest” about whether she was taking court-required medication.
It was her sixth infraction in the program — previous consequences included written assignments and “bench duty,” in which participants must sit and think about their participation in the program.
“I don’t like to incarcerate,” Malone said. “That particular participant has had some challenges. I’m rooting for her. But all the smaller penalties haven’t worked.”
Still, other participants praised Malone and her program. And, in general, some say such diversion programs provide a much-needed lifeline.
Michael Hobby, 32, of Gainesville was addicted to heroin and fentanyl when he was arrested for drug possession in August 2021. After entry into the HELP Court program, he got sober, started taking medication for anxiety and depression, and built a stable life.
“I didn’t know where to reach out for help,” he said. “I got put in handcuffs, and it saved my life.”
Even as Donald Brown awaited his fate, he said he had started taking medication to manage his depression and has stayed sober because of HELP Court.
“I’ve learned a new way of life. Instead of getting high, I’m learning to feel things now,” he said.
Brown avoided jail that early December day. A hearing to decide his fate could happen in the next few weeks. But even if he’s allowed to remain in the program, Brown said, he’s worried it’s only a matter of time before he falls out of compliance.
“To try to improve myself and get locked up for it is just a kick in the gut,” he said. “I tried really hard.”
KFF Health News senior correspondent Fred Clasen-Kelly contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Stuck in fight-or-flight mode? 5 ways to complete the ‘stress cycle’ and avoid burnout or depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you remember a time when you felt stressed leading up to a big life event and then afterwards felt like a weight had been lifted? This process – the ramping up of the stress response and then feeling this settle back down – shows completion of the “stress cycle”.
Some stress in daily life is unavoidable. But remaining stressed is unhealthy. Chronic stress increases chronic health conditions, including heart disease and stroke and diabetes. It can also lead to burnout or depression.
Exercise, cognitive, creative, social and self-soothing activities help us process stress in healthier ways and complete the stress cycle.
What does the stress cycle look like?
Scientists and researchers refer to the “stress response”, often with a focus on the fight-or-flight reactions. The phrase the “stress cycle” has been made popular by self-help experts but it does have a scientific basis.
The stress cycle is our body’s response to a stressful event, whether real or perceived, physical or psychological. It could be being chased by a vicious dog, an upcoming exam or a difficult conversation.
The stress cycle has three stages:
- stage 1 is perceiving the threat
- stage 2 is the fight-or-flight response, driven by our stress hormones: adrenaline and cortisol
- stage 3 is relief, including physiological and psychological relief. This completes the stress cycle.
Different people will respond to stress differently based on their life experiences and genetics.
Unfortunately, many people experience multiple and ongoing stressors out of their control, including the cost-of-living crisis, extreme weather events and domestic violence.
Remaining in stage 2 (the flight-or-flight response), can lead to chronic stress. Chronic stress and high cortisol can increase inflammation, which damages our brain and other organs.
When you are stuck in chronic fight-or-flight mode, you don’t think clearly and are more easily distracted. Activities that provide temporary pleasure, such as eating junk food or drinking alcohol are unhelpful strategies that do not reduce the stress effects on our brain and body. Scrolling through social media is also not an effective way to complete the stress cycle. In fact, this is associated with an increased stress response.
Stress and the brain
In the brain, chronic high cortisol can shrink the hippocampus. This can impair a person’s memory and their capacity to think and concentrate.
Chronic high cortisol also reduces activity in the prefrontal cortex but increases activity in the amygdala.
The prefrontal cortex is responsible for higher-order control of our thoughts, behaviours and emotions, and is goal-directed and rational. The amygdala is involved in reflexive and emotional responses. Higher amygdala activity and lower prefrontal cortex activity explains why we are less rational and more emotional and reactive when we are stressed.
There are five types of activities that can help our brains complete the stress cycle. https://www.youtube.com/embed/eD1wliuHxHI?wmode=transparent&start=0 It can help to understand how the brain encounters stress.
1. Exercise – its own complete stress cycle
When we exercise we get a short-term spike in cortisol, followed by a healthy reduction in cortisol and adrenaline.
Exercise also increases endorphins and serotonin, which improve mood. Endorphins cause an elated feeling often called “runner’s high” and have anti-inflammatory effects.
When you exercise, there is more blood flow to the brain and higher activity in the prefrontal cortex. This is why you can often think more clearly after a walk or run. Exercise can be a helpful way to relieve feelings of stress.
Exercise can also increase the volume of the hippocampus. This is linked to better short-term and long-term memory processing, as well as reduced stress, depression and anxiety.
2. Cognitive activities – reduce negative thinking
Overly negative thinking can trigger or extend the stress response. In our 2019 research, we found the relationship between stress and cortisol was stronger in people with more negative thinking.
Higher amygdala activity and less rational thinking when you are stressed can lead to distorted thinking such as focusing on negatives and rigid “black-and-white” thinking.
Activities to reduce negative thinking and promote a more realistic view can reduce the stress response. In clinical settings this is usually called cognitive behaviour therapy.
At home, this could be journalling or writing down worries. This engages the logical and rational parts of our brain and helps us think more realistically. Finding evidence to challenge negative thoughts (“I’ve prepared well for the exam, so I can do my best”) can help to complete the stress cycle.
Journalling could help process stressful events and complete the stress cycle. Shutterstock/Fellers Photography 3. Getting creative – a pathway out of ‘flight or fight’
Creative activities can be art, craft, gardening, cooking or other activities such as doing a puzzle, juggling, music, theatre, dancing or simply being absorbed in enjoyable work.
Such pursuits increase prefrontal cortex activity and promote flow and focus.
Flow is a state of full engagement in an activity you enjoy. It lowers high-stress levels of noradrenaline, the brain’s adrenaline. When you are focussed like this, the brain only processes information relevant to the task and ignores non-relevant information, including stresses.
4. Getting social and releasing feel-good hormones
Talking with someone else, physical affection with a person or pet and laughing can all increase oxytocin. This is a chemical messenger in the brain that increases social bonding and makes us feel connected and safe.
Laughing is also a social activity that activates parts of the limbic system – the part of the brain involved in emotional and behavioural responses. This increases endorphins and serotonin and improves our mood.
5. Self-soothing
Breathing exercises and meditation stimulate the parasympathetic nervous system (which calms down our stress responses so we can “reset”) via the vagus nerves, and reduce cortisol.
A good cry can help too by releasing stress energy and increasing oxytocin and endorphins.
Emotional tears also remove cortisol and the hormone prolactin from the body. Our prior research showed cortisol and prolactin were associated with depression, anxiety and hostility.
Getting moving can help with stress and its effects on the brain. Shutterstock/Jaromir Chalabala Action beats distraction
Whether it’s watching a funny or sad movie, exercising, journalling, gardening or doing a puzzle, there is science behind why you should complete the stress cycle.
Doing at least one positive activity every day can also reduce our baseline stress level and is beneficial for good mental health and wellbeing.
Importantly, chronic stress and burnout can also indicate the need for change, such as in our workplaces. However, not all stressful circumstances can be easily changed. Remember help is always available.
If you have concerns about your stress or health, please talk to a doctor.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14 or Kids Helpline on 1800 55 1800.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong and Susan J. Thomas, Associate professor in Mental Health and Behavioural Science, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Nutrition To Combat Lymphedema & Lipedema
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Kelly Sturm is a rehab specialist (Doctor of Physical Therapy), and also a certified lymphedema therapist. Here’s what helps her patients with lymphedema and lipedema:
Don’t fan the flames
Lymphedema and lipedema are inflammatory lymphatic diseases affecting mostly women. As such, an anti-inflammatory diet will be important, but there are other factors too:
- Anti-inflammatory diet: this is to reduce the chronic inflammation associated with lymphatic diseases. This means eating plenty of fruit and vegetables, especially berries and leafy greens, and avoiding things like sugar, alcohol, caffeine, and processed foods. And of course, don’t smoke.
- Intermittent fasting: this also helps by giving the body a chance to correct itself; when the body isn’t digesting food, it has a lot more resources to devote to its favorite activity: maintenance. This results in lower inflammation, and better fat redistribution.
- Weight loss: not a bandwagon we often get on at 10almonds as it’s rarely the most important thing, but in this case it is of high importance (second only to dealing with the inflammation), as excess weight around the lymph nodes and vessels can lead to dysfunction and swelling. Thus, reducing the weight can ease that and allow the body to heal.
For more details on all of the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Eat To Beat Inflammation ← also some non-dietary advice in there too
- Ask Not What Your Lymphatic System Can Do For You…
- Lose Weight, But Healthily ← more useful than just trying to run a calorie deficit
Take care!
Share This Post
-
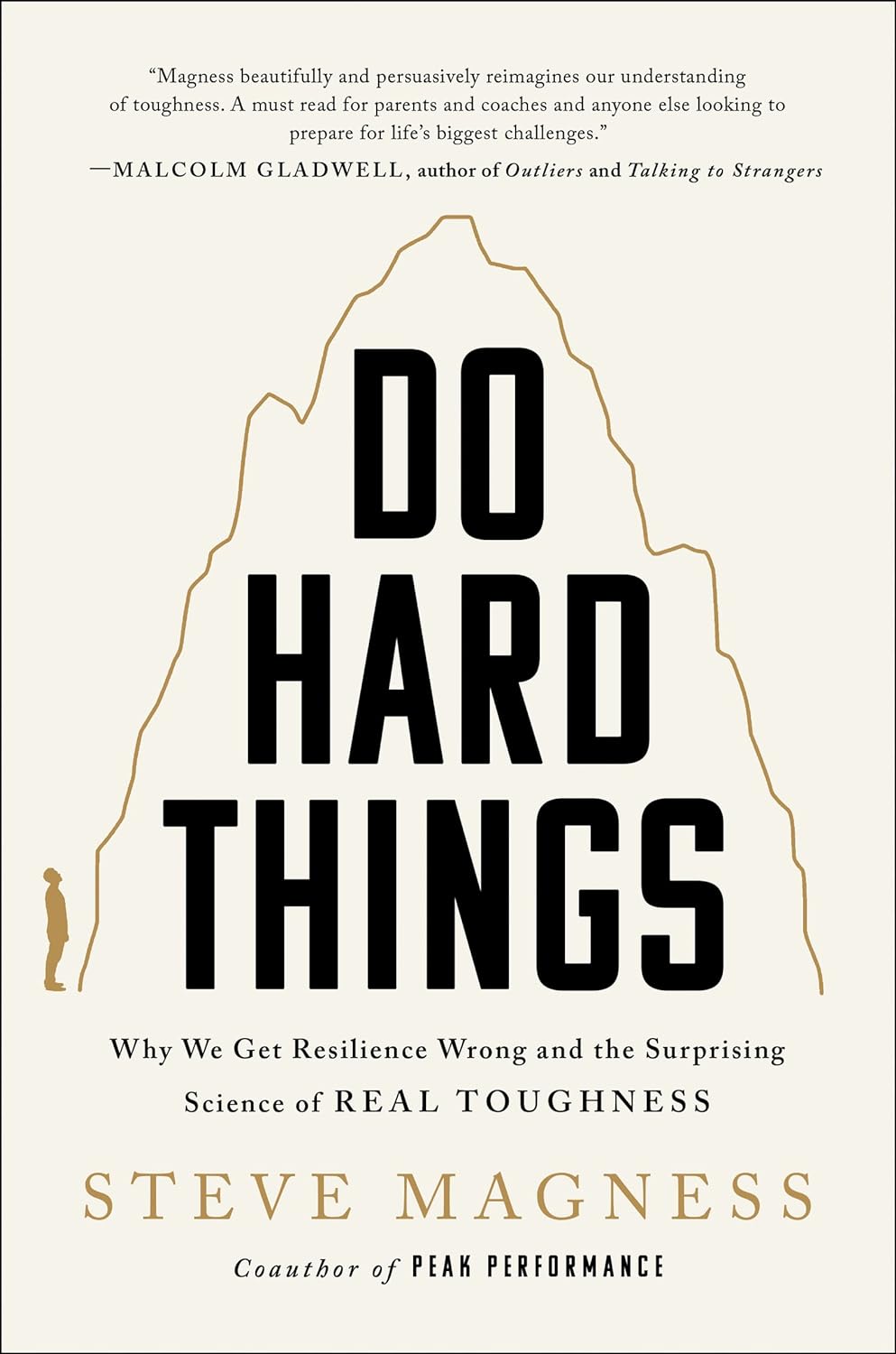
Do Hard Things – by Steve Magness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to say that we must push ourselves if we want to achieve worthwhile things—and it’s also easy to push ourselves into an early grave by overreaching. So, how to do the former, without doing the latter?
That’s what this book’s about. The author, speaking from a background in the science of sports psychology, applies his accumulated knowledge and understanding to the more general problems of life.
Most of us are, after all, not sportspeople or if we are, not serious ones. Those few who are, will get benefit from this book too! But it’s mostly aimed at the rest of us who are trying to work out whether/when we should scale up, scale back, change track, or double down:
- How much can we really achieve in our career?
- How about in retirement?
- Do we ever really get too old for athletic feats, or should we keep pressing on?
Magness brings philosophy and psychological science together, to help us sort our way through.
Nor is this just a pep talk—there’s readily applicable, practical, real-world advice here, things to enable us to do our (real!) best without getting overwhelmed.
The style is pop-science, very easy-reading, and clear and comprehensible throughout—without succumbing to undue padding either.
Bottom line: this is a very pleasant read, that promises to make life more meaningful and manageable at the same time. Highly recommendable!
Click here to check out Do Hard Things, and get the most out of life!
Share This Post
Related Posts
-
7 Signs of Undiagnosed Autism in Adults
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to adults and autism, there are two kinds of person in the popular view: those who resemble the Rain Man, and those who are making it up. But, it’s not so, as Paul Micallef explains:
The signs
We’ll not keep them a mystery; they are:
- Social interaction difficulties: such a person may struggle with understanding social cues, leading to awkwardness, isolation, or appearing eccentric.
- Need for structure and routine: either highly structured or disorganized, both of which stem from executive function challenges. The former, of course, is a coping mechanism, while the latter is the absence of same.
- Sensory sensitivities: can include sensitivities or insensitivities to light, sound, temperature, smells, tastes, and so forth.
- Spiky skillset: extreme strengths in certain areas, coupled with significant difficulties in others, leading to uneven abilities. May be able to dismantle and rebuild a PC, while not knowing how to arrange an Über.
- Emotional regulation issues: experiences of meltdowns, shutdowns, or withdrawal as coping mechanisms when overwhelmed. Not that this is “or”, not necessarily “and”. The latter goes especially unnoticed as an emotional regulation issue, because for everyone else, it’s something that’s not there to see.
- Unusual associations: making mental connections or associations that seem random or uncommon compared to others. The mind went to 17 places quickly and while everyone else got from idea A to idea B, this person is already at idea Q.
- Being “just different”: a general sense of being the odd one out, standing out in subtle or distinct ways. This is rather a catch-all, but if there’s someone who fits this, there’s a good chance, the other things apply too.
For more on all of these, whether pertaining to yourself or a loved one (or both!), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- 16 Overlooked Autistic Traits In Women
- What is AuDHD? 5 important things to know when someone has both autism and ADHD
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cassava vs Parsnip – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cassava to parsnips, we picked the parsnips.
Why?
This one wasn’t close!
In terms of macros, cassava has more than 2x the carbs while parsnips have nearly 3x the fiber, making for a very clear win for parsnips.
In the category of vitamins, cassava has more of vitamins B3 and C, while parsnips have more of vitamins B1, B2, B5, B6, B9, E, and K, with very large margins of difference in the latter two cases. Another overwhelming win for parsnips.
Looking at minerals, cassava is not higher in any minerals, while parsnips have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc; a very one-sided win for parsnips!
So, by all means enjoy either or both (diversity is good), but there’s a clear winner here today, and it’s parsnips.
Want to learn more?
You might like:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strong At Every Age: 15 Habits To Level Up Your Health & Fitness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not every increase in health and fitness needs to look like a training montage from the “Rocky” movies!
Making progress every day
We’ll not keep the 15 habits a secret; they are:
- Follow the one-minute rule: commit to just one minute of action—this makes starting easier, and often you’ll end up doing more once you’ve got started.
- Make the habit exciting: add fun elements to make the habit more enjoyable, like using new gear or accessories.
- Do it first: prioritize new habits by doing them early in the day to ensure they get done.
- Share the love: pair new habits with activities you already enjoy, where practical, to do “temptation bundling”.
- Embrace the uncomfortable: get used to discomfort daily to grow and build resilience for bigger changes.
- Do as little as possible: start small with habits, to minimize resistance and focus on consistency.
- Think how to be lazy: simplify processes and use shortcuts; there are no extra prizes for it having been difficult!
- Make the appointment: schedule habits with set dates and times, to increase accountability.
- Let habits evolve: adapt habits to fit current circumstances; that way you can still stay consistent over time.
- Plan ahead: prepare in advance to avoid setbacks—what could stop you from succeeding, and how can you pre-empt that?
- Pause to reflect: regularly evaluate what works and what doesn’t, to adjust and improve.
- Shut off your brain: avoid overthinking and start taking action now, not later, to build momentum.
- Question and learn: stay curious and open to learning, or else you will plateau quickly!
- Ask why: understand the deeper reasons behind any resistance, and make clear for yourself the value of the habit.
- Love your failures: embrace any setbacks as learning opportunities and, as such, stepping stones to success.
For more on all of each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: