Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Your Doctor May Not Tell You About Fibromyalgia – by Dr. R. Paul St Amand
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The core claim of the book is that guaifenesin, an over-the-counter expectorant (with a good safety profile) usually taken to treat a chesty cough, is absorbed from the gastrointestinal tract, and is rapidly metabolized and excreted into the urine—and on the way, it lowers uric acid levels, which is a big deal for fibromyalgia sufferers.
He goes on to explain how the guaifenesin, by a similar biochemical mechanism, additionally facilitates the removal of other excess secretions that are associated with fibromyalgia.
The science for all this is… Compelling and logical, while not being nearly so well-established yet as his confidence would have us believe.
In other words, he could be completely wrong, because adequate testing has not yet been done. However, he also could be right; scientific knowledge is, by the very reality of scientific method, always a step behind hypothesis and theory (in that order).
Meanwhile, there are certainly many glowing testimonials from fibromyalgia sufferers, saying that this helped a lot.
Bottom line: if you have fibromyalgia and do not mind trying a relatively clinically untested (yet logical and anecdotally successful) protocol to lessen then symptoms (allegedly, to zero), then this book will guide you through that and tell you everything to watch out for.
Share This Post
-
The End of Stress – by Don Joseph Goewey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, we probably know to remember to take a deep breath once in a while, and adopt a “focus on what you can control, rather than what you can’t” attitude. In this book, Goewey covers a lot more.
After an overview of how we have a brain wired for stress, what it does to us, and why we should rewire that, he dives straight into such topics as:
- Letting go of fear—safely!
- Number-crunching the real risks
- Leading with good decisions, and trusting the process
- Actively practicing a peaceful mindset (some very good tips here)
- Transcending shame (and thus sidestepping the stress that it may otherwise bring)
The book brings together a lot of ideas and factors, seamlessly. From scientific data to case studies, to “try this and see”, encouraging us to try certain exercises for ourselves and be surprised at the results.
All in all, this is a great book on not just managing stress, but—as the title suggests—ending it in all and any cases it’s not useful to us. In other words, this book? It is useful to us.
Share This Post
-
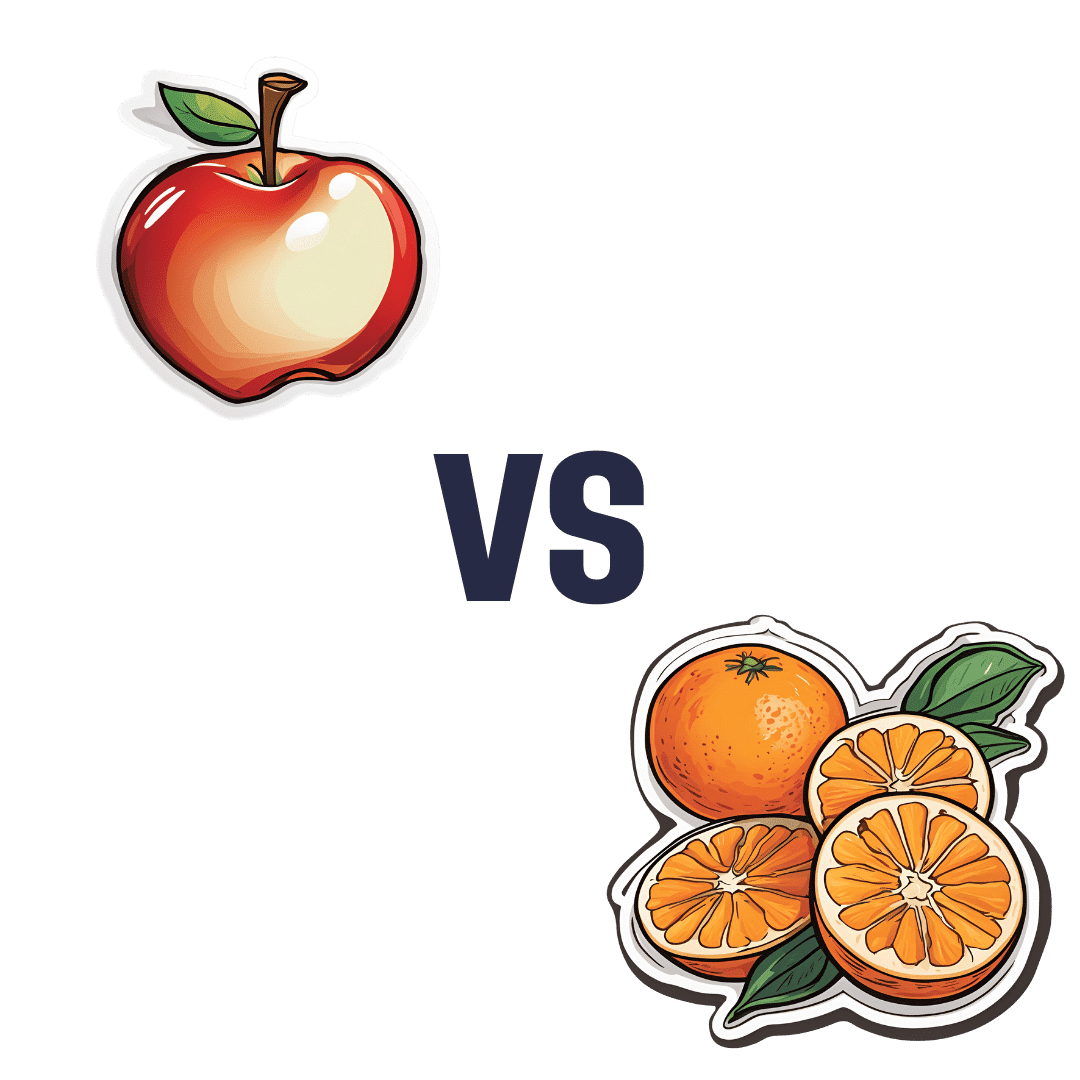
Apples vs Oranges – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apples to oranges, we picked the oranges.
Why?
In terms of macros, the two fruits are approximately equal (and indeed, on average, precisely equal in the most important metric, which is fiber). So, a tie here.
In the category of vitamins, apples are higher in vitamin K, while oranges are higher in vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline. An easy win for oranges this time.
When it comes to minerals, apples have more iron and manganese, while oranges have more calcium, copper, magnesium, phosphorus, potassium, selenium, and zinc. Another easy win for oranges.
So, adding up the sections, a clear win for oranges. But, by all means, enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
Related Posts
-
Bushfire smoke affects children differently. Here’s how to protect them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Bushfires are currently burning in Australian states including Victoria, Tasmania, Western Australia and South Australia. In some areas, fire authorities have warned residents about the presence of smoke.
Bushfire smoke is harmful to our health. Tiny particles of ash can lodge deep in the lungs.
Exposure to this type of smoke may worsen existing conditions such as asthma, and induce a range of health effects from irritation of the eyes, nose and throat to changes in the cardiovascular system.
Public health recommendations during smoke events tend to provide general advice, and don’t often include advice specifically geared at children. But children are not just little adults. They are uniquely vulnerable to environmental hazards such as bushfire smoke for a number of reasons.
Different physiology, different behaviour
Children’s lungs are still developing and maturing.
Airways are smaller in children, especially young children, which is associated with greater rates of particle deposition – when particles settle on the surfaces of the airways.
Children also breathe more air per kilogram of body weight compared with adults, and therefore inhale more polluted air relative to their size.
Further, children’s detoxification systems are still developing, so environmental toxins take longer to effectively clear from their bodies.
Meanwhile, children’s behaviour and habits may expose them to more environmental toxins than adults. For example, they tend to do more physical activity and spend more time outdoors. Higher levels of physical activity lead to more air inhaled per kilogram of body weight.
Also, a normal and important part of children’s early play is exploring their environment, including by putting things in their mouth. This can result in kids ingesting soil, dust and dirt, which often contain environmental contaminants.
For these reasons, it’s important to consider the specific needs of children when providing advice on what to do when there’s smoke in the air.
Keeping our environments healthy
The Australian government offers recommendations for minimising the health risks from exposure to bushfire smoke. The main advice includes staying indoors and keeping doors and windows closed.
This is great advice when the smoke is thick outside, but air pollutants may still accumulate inside the home. So it’s important to air your home once the smoke outside starts to clear. Take advantage of wind changes to open up and get air moving out of the house with a cross breeze.
Kids are natural scientists, so get them involved. For example, you and your child can “rate” the air each hour by looking at a landmark outside your home and rating how clearly you can see it. When you notice the haze is reducing, open up the house and clear the air.
Because air pollutants settle onto surfaces in our home and into household dust, an easy way to protect kids during smoky periods is to do a daily dust with a wet cloth and vacuum regularly. This will remove pollutants and reduce ingestion by children as they play. Frequent hand washing helps too.
Healthy bodies and minds
Research exploring the effects of bushfire smoke exposure on children’s health is sparse. However, during smoke events, we do see an increase in hospital visits for asthma, as well as children reporting irritation to their eyes, nose and throat.
If your child has asthma or another medical condition, ensure they take any prescribed medications on a regular schedule to keep their condition well controlled. This will minimise the risk of a sudden worsening of their symptoms with bushfire smoke exposure.
Make sure any action plans for symptom flare-ups are up to date, and ensure you have an adequate supply of in-date medication somewhere easy to locate and access.
Children may be anxious during a bushfire.
Media_Photos/ShutterstockKids can get worried during bushfires, and fire emergencies have been linked with a reduction in children’s mental health. Stories such as the Birdie’s Tree books can help children understand these events do pass and people help one another in times of difficulty.
Learning more about air pollution can help too. Our group has a children’s story explaining how air pollution affects our bodies and what can help.
It’s also important for parents and caregivers not to get too stressed, as children cope better when their parents manage their own anxiety and help their children do the same. Try to strike a balance between being vigilant and staying calm.
What about masks?
N95 masks can protect the wearer from fine particles in bushfire smoke, but their use is a bit complicated when it comes to kids. Most young children won’t be able to fit properly into an N95 mask, or won’t tolerate the tight fit for long periods. Also, their smaller airways make it harder for young children to breathe through a mask.
If you choose to use an N95 mask for your children, it’s best to save them for instances when high-level outdoor exposure is unavoidable, such as if you’re going outside when the smoke is very thick.
N95 masks should be replaced after around four hours or when they become damp.
If your child has an existing heart or lung condition, consult their doctor before having them wear an N95 mask.
Our team is currently recruiting for a study exploring the effects of bushfire smoke in children. If you live in south east Queensland and are interested in participating in the event of a bushfire or hazard reduction burn near your home, please express your interest here.
Dwan Vilcins, Group leader, Environmental Epidemiology, Children’s Health Environment Program, The University of Queensland; Nicholas Osborne, Associate Professor, School of Public Health, The University of Queensland, and Paul D. Robinson, Conjoint Professor in Respiratory and Sleep Medicine, Child Health Research Centre, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
DVT Risk Management Beyond The Socks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I know I am at higher risk of DVT after having hip surgery, any advice beside compression stockings?❞
First of all, a swift and easy recovery to you!
Surgery indeed increases the risk of deep vein thrombosis (henceforth: DVT), and hip or knee surgery especially so, for obvious reasons.
There are other risk factors you can’t control, like genetics (family history of DVT as an indicator) and age, but there are some that you can, including:
- smoking (so, ideally don’t; do speak to your doctor before quitting though, in case withdrawal might be temporarily worse for you than smoking)
- obesity (so, losing weight is good if overweight, but if this is going to happen, it’ll mostly happen in the kitchen not the gym, which may be a relief as you’re probably not the very most up for exercise at present)
- See also: Lose Weight, But Healthily
- sedentariness (so, while you’re probably not running marathons right now, please do try to keep moving, even if only gently)
Beyond that, yes compression socks, but also frequent gentle massage can help a lot to avoid clots forming.
Also, no surprises, a healthy diet will help, especially one that’s good for general heart health. Check out for example the Mediterranean DASH diet:
Four Ways To Upgrade The Mediterranean Diet
Also, obviously, speak with your doctor/pharmacist if you haven’t already about possible medications, including checking whether any of your current medications increase the risk and could be swapped for something that doesn’t.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Support For Long COVID & Chronic Fatigue
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Long COVID and Chronic Fatigue
Getting COVID-19 can be very physically draining, so it’s no surprise that getting Long COVID can (and usually does) result in chronic fatigue.
But, what does this mean and what can we do about it?
What makes Long COVID “long”
Long COVID is generally defined as COVID-19 whose symptoms last longer than 28 days, but in reality the symptoms not only tend to last for much longer than that, but also, they can be quite distinct.
Here’s a large (3,762 participants) study of Long COVID, which looked at 203 symptoms:
Characterizing long COVID in an international cohort: 7 months of symptoms and their impact
Three symptoms stood at out as most prevalent:
- Chronic fatigue (CFS)
- Cognitive dysfunction
- Post-exertional malaise (PEM)
The latter means “the symptoms get worse following physical or mental exertion”.
CFS, Chronic Fatigue Syndrome, is also called Myalgic Encephalomyelitis (ME).
What can be done about it?
The main “thing that people do about it” is to reduce their workload to what they can do, but this is not viable for everyone. Note that work doesn’t just mean “one’s profession”, but anything that requires physical or mental energy, including:
- Childcare
- Housework
- Errand-running
- Personal hygiene/maintenance
For many, this means having to get someone else to do the things—either with support of family and friends, or by hiring help. For many who don’t have those safety nets available, this means things simply not getting done.
That seems bleak; isn’t there anything more we can do?
Doctors’ recommendations are chiefly “wait it out and hope for the best”, which is not encouraging. Some people do recover from Long COVID; for others, it so far appears it might be lifelong. We just don’t know yet.
Doctors also recommend to journal, not for the usual mental health benefits, but because that is data collection. Patients who journal about their symptoms and then discuss those symptoms with their doctors, are contributing to the “big picture” of what Long COVID and its associated ME/CFS look like.
You may notice that that’s not so much saying what doctors can do for you, so much as what you can do for doctors (and in the big picture, eventually help them help people, which might include you).
So, is there any support for individuals with Long COVID ME/CFS?
Medically, no. Not that we could find.
However! Socially, there are grassroots support networks, that may be able to offer direct assistance, or at least point individuals to useful local resources.
Grassroots initiatives include Long COVID SOS and the Patient-Led Research Collaborative.
The patient-led organization Body Politic also used to have such a group, until it shut down due to lack of funding, but they do still have a good resource list:
Click here to check out the Body Politic resource list (it has eight more specific resources)
Stay strong!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: