Kiwi vs Lime – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to lime, we picked the kiwi.
Why?
Looking at the macros first, kiwi has more protein, more carbs, and more fiber. As with most fruits, the fiber is the number we’re most interested in for health purposes; in this case, kiwi is just slightly ahead of lime on all three of those.
In terms of vitamins, kiwi has more of vitamins A, B2, B3, B6, B9, C, E, K, and choline, while lime has a tiny bit more vitamin B5. As in, the vitamin that’s in pretty much anything and is practically impossible to be deficient in unless you are literally starving to death. You may be thinking: aren’t limes a famously good source of vitamin C? And yes, yes they are. But kiwis have >3x more. In other big differences, kiwis also have >6x more vitamin E and >67 times more vitamin K.
When it comes to minerals, kiwi has more calcium, copper, magnesium, manganese, phosphorus, potassium, and zinc, while lime has more iron and selenium. Another easy win for kiwis.
In short: enjoy both; both are good. But kiwis are the more nutritionally dense option by almost every way of measuring it.
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← kiwi is top of the list; it promotes cancer cell death while sparing healthy cells
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
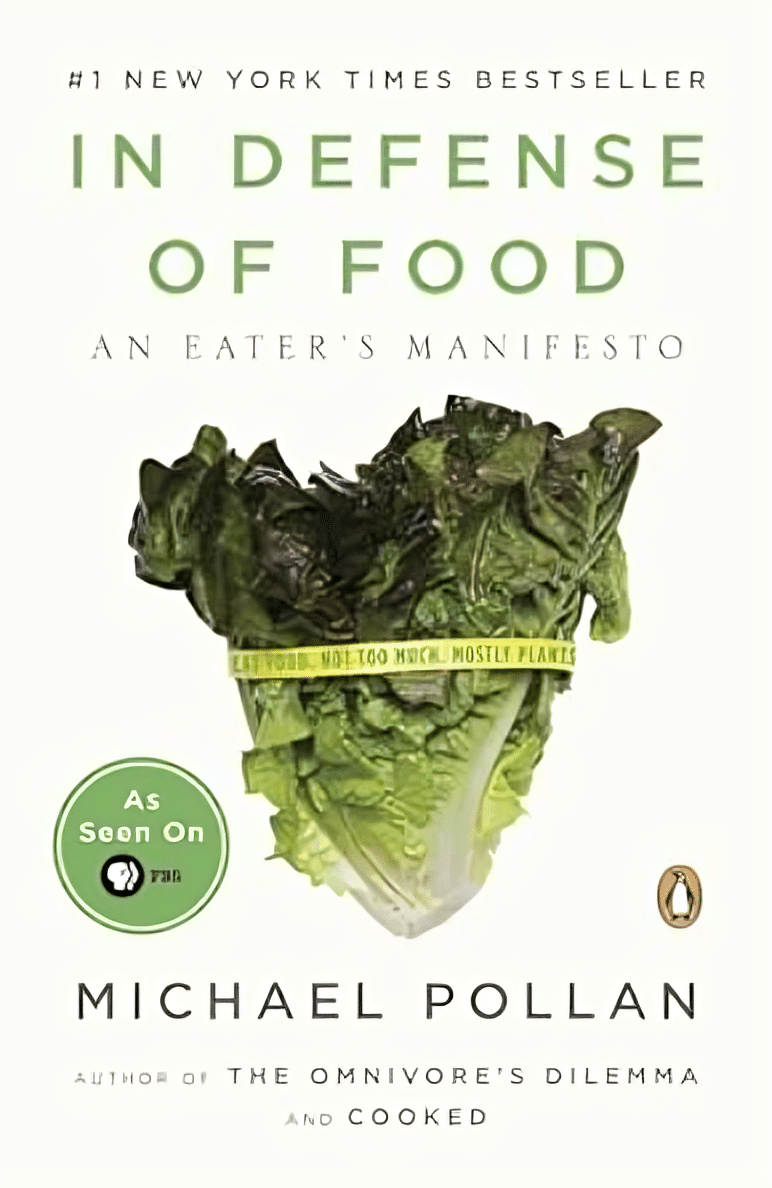
In Defense of Food – by Michael Pollan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Eat more like the French. Or the Italians. Or the Japanese. Or…
Somehow, whatever we eat is not good enough, and we should always be doing it differently!
Michael Pollan takes a more down-to-Earth approach.
He kicks off by questioning the wisdom of thinking of our food only in terms of nutritional profiles, and overthinking healthy-eating. He concludes, as many do, that a “common-sense, moderate” approach is needed.
And yet, most people who believe they are taking a “common-sense, moderate” approach to health are in fact over-fed yet under-nourished.
So, how to fix this?
He offers us a reframe: to think of food as a relationship, and health being a product of it:
- If we are constantly stressing about a relationship, it’s probably not good.
- On the other hand, if we are completely thoughtless about it, it’s probably not good either.
- But if we can outline some good, basic principles and celebrate it with a whole heart? It’s probably at the very least decent.
The style is very casual and readable throughout. His conclusions, by the way, can be summed up as “Eat real food, make it mostly plants, and make it not too much”.
However, to summarize it thusly undercuts a lot of the actual value of the book, which is the principles for discerning what is “real food” and what is “not too much”.
Bottom line: if you’re tired of complicated eating plans, this book can help produce something very simple, attainable, and really quite good.
Click here to check out In Defense of Food, for some good, hearty eating.
Share This Post
-
Sauerkraut vs Pickled Cucumber – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sauerkraut to pickled cucumber, we picked the sauerkraut.
Why?
Both of these fermented foods can give a gut-healthy microbiome boost, but how do they stack up otherwise?
In terms of macros, sauerkraut has more protein, carbs, and fiber. They are both low glycemic index foods, so we’ll go with the one that has more fiber out of the two, and that’s the ‘kraut.
In the category of vitamins, sauerkraut has more of vitamins B1, B2, B3, B5, B6, B7, B9, C, E, and choline, while pickled cucumbers have more of vitamins A and K. An easy win for sauerkraut.
When it comes to minerals, sauerkraut has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pickled cucumbers are not higher in any mineral, except sodium (on average, pickled cucumbers have about 2x the sodium of sauerkraut). Another clear win for sauerkraut.
In short, enjoy either or both in moderation, but it’s clear which boasts the most nutritional benefits, and that’s the sauerkraut!
Want to learn more?
You might like to read:
Make Friends With Your Gut (You Can Thank Us Later)
Take care!
Share This Post
-
Can Medical Schools Funnel More Doctors Into the Primary Care Pipeline?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout her childhood, Julia Lo Cascio dreamed of becoming a pediatrician. So, when applying to medical school, she was thrilled to discover a new, small school founded specifically to train primary care doctors: NYU Grossman Long Island School of Medicine.
Now in her final year at the Mineola, New York, school, Lo Cascio remains committed to primary care pediatrics. But many young doctors choose otherwise as they leave medical school for their residencies. In 2024, 252 of the nation’s 3,139 pediatric residency slots went unfilled and family medicine programs faced 636 vacant residencies out of 5,231 as students chased higher-paying specialties.
Lo Cascio, 24, said her three-year accelerated program nurtured her goal of becoming a pediatrician. Could other medical schools do more to promote primary care? The question could not be more urgent. The Association of American Medical Colleges projects a shortage of 20,200 to 40,400 primary care doctors by 2036. This means many Americans will lose out on the benefits of primary care, which research shows improves health, leading to fewer hospital visits and less chronic illness.
Many medical students start out expressing interest in primary care. Then they end up at schools based in academic medical centers, where students become enthralled by complex cases in hospitals, while witnessing little primary care.
The driving force is often money, said Andrew Bazemore, a physician and a senior vice president at the American Board of Family Medicine. “Subspecialties tend to generate a lot of wealth, not only for the individual specialists, but for the whole system in the hospital,” he said.
A department’s cache of federal and pharmaceutical-company grants often determines its size and prestige, he said. And at least 12 medical schools, including Harvard, Yale, and Johns Hopkins, don’t even have full-fledged family medicine departments. Students at these schools can study internal medicine, but many of those graduates end up choosing subspecialties like gastroenterology or cardiology.
One potential solution: eliminate tuition, in the hope that debt-free students will base their career choice on passion rather than paycheck. In 2024, two elite medical schools — the Albert Einstein College of Medicine and the Johns Hopkins University School of Medicine — announced that charitable donations are enabling them to waive tuition, joining a handful of other tuition-free schools.
But the contrast between the school Lo Cascio attends and the institution that founded it starkly illustrates the limitations of this approach. Neither charges tuition.
In 2024, two-thirds of students graduating from her Long Island school chose residencies in primary care. Lo Cascio said the tuition waiver wasn’t a deciding factor in choosing pediatrics, among the lowest-paid specialties, with an average annual income of $260,000, according to Medscape.
At the sister school, the Manhattan-based NYU Grossman School of Medicine, the majority of its 2024 graduates chose specialties like orthopedics (averaging $558,000 a year) or dermatology ($479,000).
Primary care typically gets little respect. Professors and peers alike admonish students: If you’re so smart, why would you choose primary care? Anand Chukka, 27, said he has heard that refrain regularly throughout his years as a student at Harvard Medical School. Even his parents, both PhD scientists, wondered if he was wasting his education by pursuing primary care.
Seemingly minor issues can influence students’ decisions, Chukka said. He recalls envying the students on hospital rotations who routinely were served lunch, while those in primary care settings had to fetch their own.
Despite such headwinds, Chukka, now in his final year, remains enthusiastic about primary care. He has long wanted to care for poor and other underserved people, and a one-year clerkship at a community practice serving low-income patients reinforced that plan.
When students look to the future, especially if they haven’t had such exposure, primary care can seem grim, burdened with time-consuming administrative tasks, such as seeking prior authorizations from insurers and grappling with electronic medical records.
While specialists may also face bureaucracy, primary care practices have it much worse: They have more patients and less money to hire help amid burgeoning paperwork requirements, said Caroline Richardson, chair of family medicine at Brown University’s Warren Alpert Medical School.
“It’s not the medical schools that are the problem; it’s the job,” Richardson said. “The job is too toxic.”
Kevin Grumbach, a professor of family and community medicine at the University of California-San Francisco, spent decades trying to boost the share of students choosing primary care, only to conclude: “There’s really very little that we can do in medical school to change people’s career trajectories.”
Instead, he said, the U.S. health care system must address the low pay and lack of support.
And yet, some schools find a way to produce significant proportions of primary care doctors — through recruitment and programs that provide positive experiences and mentors.
U.S. News & World Report recently ranked 168 medical schools by the percentage of graduates who were practicing primary care six to eight years after graduation.
The top 10 schools are all osteopathic medical schools, with 41% to 47% of their students still practicing primary care. Unlike allopathic medical schools, which award MD degrees, osteopathic schools, which award DO degrees, have a history of focusing on primary care and are graduating a growing share of the nation’s primary care physicians.
At the bottom of the U.S. News list is Yale, with 10.7% of its graduates finding lasting careers in primary care. Other elite schools have similar rates: Johns Hopkins, 13.1%; Harvard, 13.7%.
In contrast, public universities that have made it a mission to promote primary care have much higher numbers.
The University of Washington — No. 18 in the ranking, with 36.9% of graduates working in primary care — has a decades-old program placing students in remote parts of Washington, Wyoming, Alaska, Montana, and Idaho. UW recruits students from those areas, and many go back to practice there, with more than 20% of graduates settling in rural communities, according to Joshua Jauregui, assistant dean for clinical curriculum.
Likewise, the University of California-Davis (No. 22, with 36.3% of graduates in primary care) increased the percentage of students choosing family medicine from 12% in 2009 to 18% in 2023, even as it ranks high in specialty training. Programs such as an accelerated three-year primary care “pathway,” which enrolls primarily first-generation college students, help sustain interest in non-specialty medical fields.
The effort starts with recruitment, looking beyond test scores to the life experiences that forge the compassionate, humanistic doctors most needed in primary care, said Mark Henderson, associate dean for admissions and outreach. Most of the students have families who struggle to get primary care, he said. “So they care a lot about it, and it’s not just an intellectual, abstract sense.”
Establishing schools dedicated to primary care, like the one on Long Island, is not a solution in the eyes of some advocates, who consider primary care the backbone of medicine and not a separate discipline. Toyese Oyeyemi Jr., executive director of the Social Mission Alliance at the Fitzhugh Mullan Institute of Health Workforce Equity, worries that establishing such schools might let others “off the hook.”
Still, attending a medical school created to produce primary care doctors worked out well for Lo Cascio. Although she underwent the usual specialty rotations, her passion for pediatrics never flagged — owing to her 23 classmates, two mentors, and her first-year clerkship shadowing a community pediatrician. Now, she’s applying for pediatric residencies.
Lo Cascio also has deep personal reasons: Throughout her experience with a congenital heart condition, her pediatrician was a “guiding light.”
“No matter what else has happened in school, in life, in the world, and medically, your pediatrician is the person that you can come back to,” she said. “What a beautiful opportunity it would be to be that for someone else.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
I can’t afford olive oil. What else can I use?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you buy your olive oil in bulk, you’ve likely been in for a shock in recent weeks. Major supermarkets have been selling olive oil for up to A$65 for a four-litre tin, and up to $26 for a 750 millilitre bottle.
We’ve been hearing about the health benefits of olive oil for years. And many of us are adding it to salads, or baking and frying with it.
But during a cost-of-living crisis, these high prices can put olive oil out of reach.
Let’s take a look at why olive oil is in demand, why it’s so expensive right now, and what to do until prices come down.
Joyisjoyful/Shutterstock Remind me, why is olive oil so good for you?
Including olive oil in your diet can reduce your risk of developing type 2 diabetes and improve heart health through more favourable blood pressure, inflammation and cholesterol levels.
This is largely because olive oil is high in monounsaturated fatty acids and polyphenols (antioxidants).
Some researchers have suggested you can get these benefits from consuming up to 20 grams a day. That’s equivalent to about five teaspoons of olive oil.
Why is olive oil so expensive right now?
A European heatwave and drought have limited Spanish and Italian producers’ ability to supply olive oil to international markets, including Australia.
This has been coupled with an unusually cold and short growing season for Australian olive oil suppliers.
The lower-than-usual production and supply of olive oil, together with heightened demand from shoppers, means prices have gone up.
We’ve seen unfavourable growing conditions in Europe and Australia. KaMay/Shutterstock How can I make my olive oil go further?
Many households buy olive oil in large quantities because it is cheaper per litre. So, if you have some still in stock, you can make it go further by:
- storing it correctly – make sure the lid is on tightly and it’s kept in a cool, dark place, such as a pantry or cabinet. If stored this way, olive oil can typically last 12–18 months
- using a spray – sprays distribute oil more evenly than pourers, using less olive oil overall. You could buy a spray bottle to fill from a large tin, as needed
- straining or freezing it – if you have leftover olive oil after frying, strain it and reuse it for other fried dishes. You could also freeze this used oil in an airtight container, then thaw and fry with it later, without affecting the oil’s taste and other characteristics. But for dressings, only use fresh oil.
I’ve run out of olive oil. What else can I use?
Here are some healthy and cheaper alternatives to olive oil:
- canola oil is a good alternative for frying. It’s relatively low in saturated fat so is generally considered healthy. Like olive oil, it is high in healthy monounsaturated fats. Cost? Up to $6 for a 750mL bottle (home brand is about half the price)
- sunflower oil is a great alternative to use on salads or for frying. It has a mild flavour that does not overwhelm other ingredients. Some studies suggest using sunflower oil may help reduce your risk of heart disease by lowering LDL (bad) cholesterol and raising HDL (good) cholesterol. Cost? Up to $6.50 for a 750mL bottle (again, home brand is about half the price)
- sesame oil has a nutty flavour. It’s good for Asian dressings, and frying. Light sesame oil is typically used as a neutral cooking oil, while the toasted type is used to flavour sauces. Sesame oil is high in antioxidants and has some anti-inflammatory properties. Sesame oil is generally sold in smaller bottles than canola or sunflower oil. Cost? Up to $5 for a 150mL bottle.
There are plenty of alternative oils you can use in salads or for frying. narai chal/Shutterstock How can I use less oil, generally?
Using less oil in your cooking could keep your meals healthy. Here are some alternatives and cooking techniques:
- use alternatives for baking – unless you are making an olive oil cake, if your recipe calls for a large quantity of oil, try using an alternative such as apple sauce, Greek yoghurt or mashed banana
- use non-stick cookware – using high-quality, non-stick pots and pans reduces the need for oil when cooking, or means you don’t need oil at all
- steam instead – steam vegetables, fish and poultry to retain nutrients and moisture without adding oil
- bake or roast – potatoes, vegetables or chicken can be baked or roasted rather than fried. You can still achieve crispy textures without needing excessive oil
- grill – the natural fats in meat and vegetables can help keep ingredients moist, without using oil
- use stock – instead of sautéing vegetables in oil, try using vegetable broth or stock to add flavour
- try vinegar or citrus – use vinegar or citrus juice (such as lemon or lime) to add flavour to salads, marinades and sauces without relying on oil
- use natural moisture – use the natural moisture in ingredients such as tomatoes, onions and mushrooms to cook dishes without adding extra oil. They release moisture as they cook, helping to prevent sticking.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Heart-Healthy Gochujang Noodles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Soba noodles are a good source of rutin, which is great for the heart and blood. Additionally, buckwheat (as soba noodles are made from) is healthier in various ways than rice, and certainly a lot healthier than wheat (remember that despite the name, buckwheat is about as related to wheat as a lionfish is to a lion). This dish is filled with more than just fiber though; there are a lot of powerful phytochemicals at play here, in the various kinds of cabbage, plus of course things like gingerol, capsaicin, allicin, and piperine.
You will need
- 14 oz “straight to wok” style soba noodles
- 3 bok choi (about 7 oz)
- 3½ oz red cabbage, thinly sliced
- 10 oz raw and peeled large shrimp (if you are vegan, vegetarian, allergic to shellfish/crustaceans, or observant of a religion that does not eat such, substitute with small cubes of firm tofu)
- 1 can (8 oz) sliced water chestnuts, drained (drained weight about 5 oz)
- 2 tbsp gochujang paste
- 2 tbsp low-sodium soy sauce
- 1 tbsp sesame oil
- 2 tsp garlic paste
- 2 tsp ginger paste
- 1 tbsp chia seeds
- Avocado oil for frying (or another oil suitable for high temperatures—so, not olive oil)
Note: ideally you will have a good quality gochujang paste always in your cupboard, as it’s a great and versatile condiment. However, you can make your own approximation, by blending 5 pitted Medjool dates, 1 tbsp rice wine vinegar, 2 tbsp tomato purée, 2 tsp red chili flakes, 1 tsp garlic granules, and ¼ tsp MSG or ½ tsp low-sodium salt. This is not exactly gochujang, but unless you want to go shopping for ingredients more obscure in Western stores than gochujang, it’s close enough.
Method
(we suggest you read everything at least once before doing anything)
1) Mix together the gochujang paste with the sesame oil, soy sauce, garlic paste, and ginger paste, in a small bowl. Whisk in ¼ cup hot water, or a little more if it seems necessary, but go easy with it. This will be your stir-fry sauce.
2) Slice the base of the bok choi into thin disks; keep the leaves aside.
3) Heat the wok to the highest temperature you can safely muster, and add a little avocado oil followed by the shrimp. When they turn from gray to pink (this will take seconds, so be ready) add the sliced base of the bok choi, and also the sliced cabbage and water chestnuts, stirring frequently. Cook for about 2 minutes; do not reduce the heat.
4) Add the sauce you made, followed 1 minute later by the noodles, stirring them in, and finally the leafy tops of the bok choi.
5) Garnish with the chia seeds (or sesame seeds, but chia pack more of a nutritional punch), and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- What Matters Most For Your Heart?
- Red Cabbage vs White Cabbage – Which is Healthier?
- Ginger Does A Lot More Than You Think
- The Many Health Benefits Of Garlic
- Capsaicin For Weight Loss And Against Inflammation
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Emperor’s New Klotho, Or Something More?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Unzipping The Genes Of Aging?
Klotho is an enzyme encoded in humans’ genes—specifically, in the KL gene.
It’s found throughout all living parts of the human body (and can even circulate about in its hormonal form, or come to rest in its membranaceous form), and its subgroups are especially found:
- α-klotho: in the brain
- β-klotho: in the liver
- γ-klotho: in the kidneys
Great! Why do we care?
Klotho, its varieties and variants, its presence or absence, are very important in aging.
Almost every biological manifestation of aging in humans has some klotho-related indicator; usually the decrease or mutation of some kind of klotho.
Which way around the cause and effect go has been the subject of much debate and research: do we get old because we don’t have enough klotho, or do we make less klotho because we’re getting old?
Of course, everything has to be tested per variant and per system, so that can take a while (punctuated by research scientists begging for more grants to do the next one). Given that it’s about aging, testing in humans would take an incredibly long while, so most studies so far have been rodent studies.
The general gist of the results of rodent studies is “reduced klotho hastens aging; increased klotho slows it”.
(this can be known by artificially increasing or decreasing the level of klotho expression, again something easier in mice as it is harder to arrange transgenic humans for the studies)
Here’s one example of many, of that vast set of rodent studies:
Suppression of Aging in Mice by the Hormone Klotho
Relevance for Alzheimer’s, and a science-based advice
A few years ago (2020), an Alzheimer’s study was undertaken; they noted that the famous apolipoprotein E4 (apoE4) allele is the strongest genetic risk factor for Alzheimer’s, and that klotho may be another. FGF21 (secreted by the liver, mostly during fasting) binds to its own receptor (FGFR1) and its co-receptor β-klotho. Since this is a known neuroprotective factor, they wondered whether klotho itself may interact with β-amyloid (Aβ), and found:
❝Aβ can enhance the ability of klotho to draw FGF21 to regions of incipient neurodegeneration in AD❞
In other words: β-amyloid, the substance whose accumulation is associated with neurodegeneration in Alzheimer’s disease, is a mediator in klotho bringing a known neuroprotective factor, FGF21, to the areas of neurodegeneration
In fewer words: klotho calls the firefighters to the scene of the fire
Read more: Alignment of Alzheimer’s disease amyloid β-peptide and klotho
The advice based on this? Consider practicing intermittent fasting, if that is viable for you, as it will give your liver more FGF21-secreting time, and the more FGF21, the more firefighters arrive when klotho sounds the alarm.
See also: Intermittent Fasting: What’s the truth?
…and while you’re at it:
Does intermittent fasting have benefits for our brain?
A more recent (2023) study with a slightly different (but connected) purpose, found results consistent with this:
Longevity factor klotho enhances cognition in aged nonhuman primates
…and, for that matter this (2023) study that found:
Associations between klotho and telomere biology in high stress caregivers
…which looks promising, but we’d like to see it repeated with a sounder method (they sorted caregiving into “high-stress” and “low-stress” depending on whether a child was diagnosed with ASD or not, which is by no means a reliable way of sorting this). They did ask for reported subjective stress levels, but to be more objective, we’d like to see clinical markers of stress (e.g. cortisol levels, blood pressure, heart rate changes, etc).
A very recent (April 2024) study found that it has implications for more aspects of aging—and this time, in humans (but using a population-based cohort study, rather than lab conditions):
Can I get it as a supplement?
Not with today’s technology and today’s paucity of clinical trials, you can’t. Maybe in the future!
However… The presence of senescent (old, badly copied, stumbling and staggering onwards when they should have been killed and eaten and recycled already) cells actively reduces klotho levels, which means that taking supplements that are senolytic (i.e., that kill those senescent cells) can increase serum klotho levels:
Orally-active, clinically-translatable senolytics restore α-Klotho in mice and humans
Ok, what can I take for that?
We wrote about a senolytic supplement that you might enjoy, recently:
Fisetin: The Anti-Aging Assassin
Want to know more?
If you have the time, Dr. Peter Attia interviews Dr. Dena Dubal (researcher in several of the above studies) here:
Click Here If The Embedded Video Doesn’t Load Automatically
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: