It’s Not Hysteria – by Dr. Karen Tan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
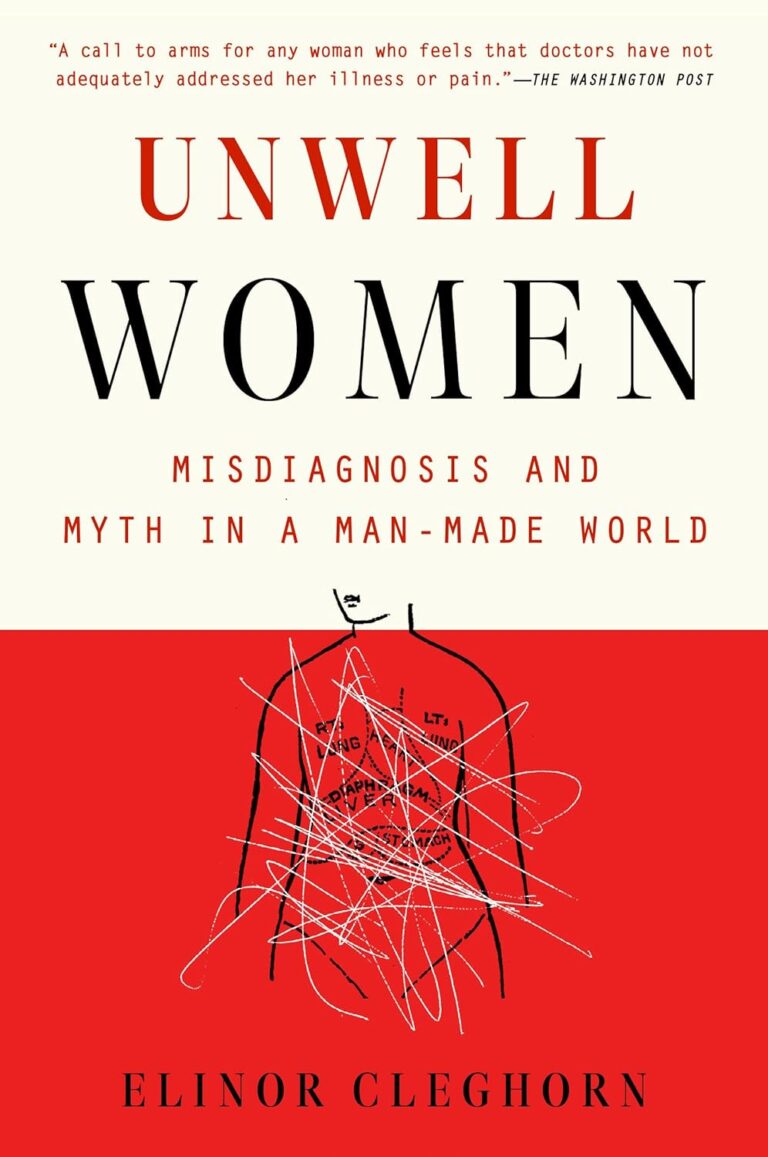
Firstly, who this book is aimed at: in case it wasn’t clear, this book assumes you have, or at least have had, a uterus. If that’s not you, then well, it’ll still be an interesting read but it won’t be about your reproductive health.
Secondly, about that “reproductive health”: it’s mostly not actually about reproductive health literally, but rather, the health of one’s reproductive organs and the things that they affect—which is a lot more than the ability to reproduce!
Dr. Tang takes us on a (respectably in-depth) tour of the relevant anatomy, before moving on to physiology, before continuing to pathology (i.e. things that can go wrong, and often do), and finally various treatment options, including elective procedures, and the pros and cons thereof.
She also talks the reader through talking about things with gynecologists and other healthcare providers, and making sure concerns are not dismissed out-of-hand (something that happens a lot, of course).
The style throughout is quite detailed prose, but without being difficult at all to read, and (assuming one is interested in the topic) it’s very engaging.
Bottom line: if you would like to know more about uteri and everything that is (or commonly/unfortunately) can be attached to them, the effects they have on the rest of the body and health, and what can be done about things not being quite right, then this is a good book for that.
Click here to check out It’s Not Hysteria, and understand more of what’s going on down there!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What does lion’s mane mushroom actually do, anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may know it as an ingredient in nootropic supplements. You may have heard of lion’s mane mushroom coffee. You may know it as the big shaggy white mushroom that grows in nature and can look very impressive.
What’s special about it?
The lion’s mane mushroom, or Hericium erinaceus (we mention, as studies we’ll cite often use the botanical name) is an adaptogenic agent that has an established ability to promote nerve regeneration through nerve growth factor neurotrophic activity. In other words, it helps (re)grow neurons.
In a 2023 study, researchers wondered if its abilities (well-established in the peripheral nervous system) would work in the central nervous system too, namely the brain, specifically the hippocampus (responsible for memory).
To boil what they found down to a single line, they concluded:
❝[Lion’s mane extract] therefore acts through a novel pan-neurotrophic signaling pathway, leading to improved cognitive performance.❞
You can read the full study for yourself (with pictures!) here:
Limitations of the study
It’s worth noting that the above study was performed on mice brains, not those of humans. As there is a shortage of human volunteers willing to have their brains sliced and examined under microscopes, we do not expect this study to be repeated with humans any time soon.
So, are there human studies that have been done?
There are! Particularly promising was this 2020 study of people with Alzheimer’s disease, wherein supplementation with 1g of lion’s mane mushroom daily for 49 weeks significantly increased cognitive test scores compared with a placebo; you can read about it here:
Additionally, this 2019 study showed that taking 1.2g daily for eight weeks helped relieve depression, anxiety, and sleep disorders in overweight or obese patiences:
Are there other health benefits?
It seems so! Unfortunately, most of its other health claims are only supported by animal studies so far, aside from one small study funded by a supplement company for their supplement that contained mostly Agaricus blazei (a different mushroom) with 14% lion’s mane.
However, in animal studies, lion’s mane has also shown promise:
- For digestion
- Against inflammation
- For cardiovascular health
- For diabetes management
- Against cancer
- Against aging
Where can I get it?
We don’t sell it (or anything else, for that matter) but if you’d like to try it, here’s an example product for your convenience:
Share This Post
-
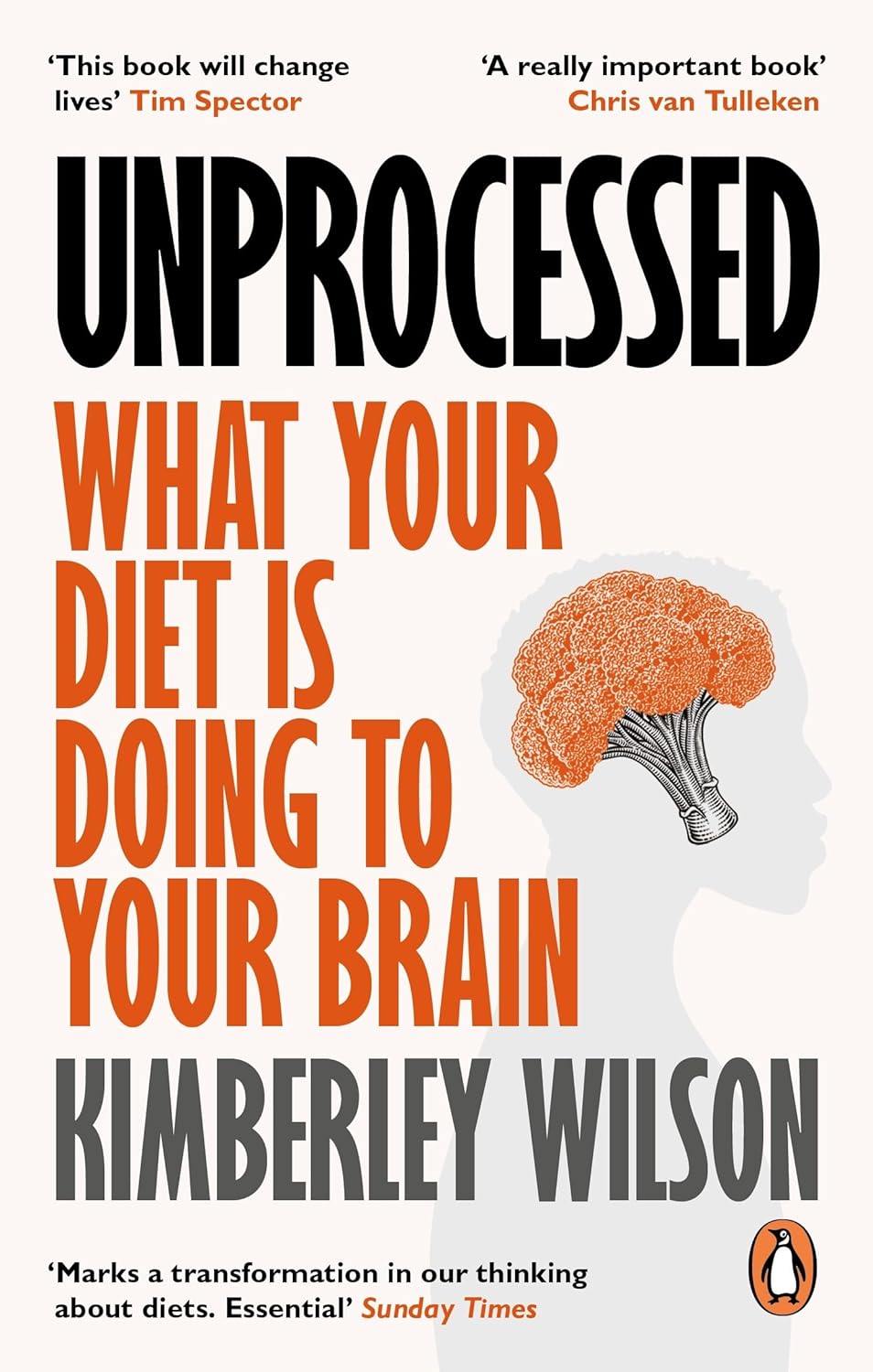
Unprocessed – by Kimberly Wilson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: hundreds of pages to say “eat less processed food”. That is, of course, also advisable (and indeed, is advised in the book too), but there’s a lot more going on here too.
Though not a doctor, the author is a psychologist who brings a lot of data to the table, especially when it comes to the neurophysiology at hand, what forgotten micronutrients many people are lacking, and what trends in society worsen these deficiencies in the population at large.
If you only care about the broadest of take-away advice, it is: eat a diet that’s mostly minimally processed plants and some oily fish, watch out for certain deficiencies in particular, and increase dietary intake of them where necessary (with taking supplements as a respectable next-best remedy).
On which note, a point of criticism is that there’s some incorrect information about veganism and brain health; she mentions that DHA is only found in fish (in fact, fish get it from algae, which has it, and is the basis of many vegan omega-3 supplements), and the B12 is found only in animals (also found in yeast, which is not an animal, as well as various bacteria in soil, and farm animals get their B12 from supplements these days anyway, so it is arguable that we could keep things simpler by just cutting out the middlecow).
However, the strength of this book really is in the delivery of understanding about why certain things matter. If you’re told “such-and-such is good for the brain”, you’ll up your intake for 1–60 days, depending on whether you bought a supermarket item or ordered a batch of supplements. And then you’ll forget, until 6–12 months later, and you’ll do it again. On the other hand, if you understand how something is good or bad for the brain, what it does (for good or ill) on a cellular level, the chemistry and neurophysiology at hand, you’ll make new habits for life.
The style is middle-range pop-science; by this we mean there are tables of data and some long words that are difficult to pronounce, but also it’s not just hard science throughout—there’s (as one might expect from an author who is a psychologist) a lot about the psychology and sociology of why many people make poor dietary decisions, and the things governments often do (or omit doing) that affect this adversely—and how we can avoid those traps as individuals (unless we be incarcerated or such).
As an aside, the author is British, so governmental examples are mostly UK-based, but it doesn’t take a lot to mentally measure that against what the governments of, for example, the US or Canada do the same or differently.
Bottom line: there’s a lot of great information about brain health here; the strongest parts are whether the author stays within her field (psychology encompasses such diverse topics as neurophysiology and aspects of sociology, but not microbiology, for example). If you want to learn about the physiology of brain health and enjoy quite a sociopolitical ride along the way, this one’s a good one for that.
Click here to check out Unprocessed, and make the best choices for you!
Share This Post
-
No Equipment Muscle Gain Routine for Ages 50+
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sarcopenia, the loss of muscle mass commonly associated with aging, can be a big problem as it leaves us vulnerable to injury (and also isn’t great for the metabolism—keeping adequate muscle mass ensures keeping the metabolism ticking over nicely). Will Harlow, over-50s specialist physiotherapist, is here to share a routine that works without weights:
Where it counts
There’s a fair amount of emphasis here on the lower body and core. That’s because in practical terms, this is what matters more for our health than having bulging biceps:
- First exercise: donkey calf raises to build strength in the calves using a chair.
- Second exercise: single-leg elevated lunge to work the quads and glutes, using a step or books for elevation.
- Third exercise: slow sit-to-stand for quads, glutes, and core strength, focusing on a slow descent.
- Fourth exercise: wall press-up to strengthen the chest, shoulders, and arms, with a variation using towels for increased resistance.
- Final exercise: shoulder raises using bottles or similar weights to target the shoulders and rotator cuffs.
Ok, so that last one was a slight cheat on his part as it does require grabbing a weight, but it’s not specialist equipment at least, and can just be something you grabbed at home. It’s also the least important of the five exercises, and can be skipped if necessary.
For more on all of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
The Optimal Morning Routine, Per Neuroscience
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Andrew Huberman, neuroscientist and professor of neurobiology, has insights:
The foundations of a good day
Here are some key things to consider:
- The role of light: get sunlight exposure within an hour of waking to anchor your body’s cortisol pulse, set your circadian rhythm, and boost mood-regulating dopamine. Light exposure on the skin also boost hormone levels like testosterone and estrogen, contributing to energy, motivation, and overall wellbeing.
- The role of caffeine: delay caffeine intake for 60–90 minutes after waking to allow adenosine to clear naturally, preventing afternoon energy crashes. Otherwise, caffeine will block the adenosine for 4–8 hours, causing the wave of adenosine-induced sleepiness to resurge later.
- The role of exercise: morning exercise helps clear adenosine, raise core body temperature, and improve wakefulness
- The role of cold: cold showers or ice baths trigger adrenaline and dopamine surges, enhancing mood and drive for hours.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Morning Routines That Just Flow
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
It’s Not You, It’s Your Hormones – by Nicki Williams, DipION, mBANT, CNHC
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, first a quick note: this book is very similar to the popular bestseller “The Galveston Diet”, not just in content, but all the way down to its formatting. Some Amazon reviewers have even gone so far as to suggest that “It’s Not You, It’s Your Hormones” (2017) brazenly plagiarized “The Galveston Diet” (2023). However, after carefully examining the publication dates, we feel quite confident that this book is not a copy of the one that came out six years after it. As such, we’ve opted for reviewing the original book.
Nicki Williams’ basic principle is that we can manage our hormonal fluctuations, by managing our diet. Specifically, in three main ways:
- Intermittent fasting
- Anti-inflammatory diet
- Eating more protein and healthy fats
Why should these things matter to our hormones? The answer is to remember that our hormones aren’t just the sex hormones. We have hormones for hunger and satedness, hormones for stress and relaxation, hormones for blood sugar regulation, hormones for sleep and wakefulness, and more. These many hormones make up our endocrine system, and affecting one part of it will affect the others.
Will these things magically undo the effects of the menopause? Well, some things yes, other things no. No diet can do the job of HRT. But by tweaking endocrine system inputs, we can tweak endocrine system outputs, and that’s what this book is for.
The style is very accessible and clear, and Williams walks us through the changes we may want to make, to avoid the changes we don’t want.
In the category of criticism, there is some extra support that’s paywalled, in the sense that she wants the reader to buy her personally-branded online plan, and it can feel a bit like she’s holding back in order to upsell to that.
Bottom line: this book is aimed at peri-menopausal and post-menopausal women. It could also definitely help a lot of people with PCOS too, and, when it comes down to it, pretty much anyone with an endocrine system. It’s a well-evidenced, well-established, healthy way of eating regardless of age, sex, or (most) physical conditions.
Click here to check out It’s Not You, It’s Your Hormones, and take control of yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those with a sweet tooth, it can be challenging to indulge one’s desires while also avoiding inflammation. Happily, Dr. Jia-Yia Lui has scientific insights to share!
Dr. Liu’s Top 10
We’ll not keep them a mystery; they are:
- Grapes
- Goji berries
- Barberries
- Persimmons
- Longans
- Lychees
- Raisins¹
- Applesauce²
- Plums³
- Dates
¹Yes, these are technically also grapes, but there are enough differences that Dr. Liu tackles them separately.
²It makes a difference how it’s made, though.
³And dried plums, in other words, prunes.For more details on all of these, plus their extra benefits and relevant considerations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- How to Prevent (or Reduce) Inflammation
- The Not-So-Sweet Science Of Sugar Addiction
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: