Is it OK to lie to someone with dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There was disagreement on social media recently after a story was published about an aged care provider creating “fake-away” burgers that mimicked those from a fast-food chain, to a resident living with dementia. The man had such strict food preferences he was refusing to eat anything at meals except a burger from the franchise. This dementia symptom risks malnutrition and social isolation.
But critics of the fake burger approach labelled it trickery and deception of a vulnerable person with cognitive impairment.
Dementia is an illness that progressively robs us of memories. Although it has many forms, it is typical for short-term recall – the memory of something that happened in recent hours or days – to be lost first. As the illness progresses, people may come to increasingly “live in the past”, as distant recall gradually becomes the only memories accessible to the person. So a person in the middle or later stages of the disease may relate to the world as it once was, not how it is today.
This can make ethical care very challenging.

Is it wrong to lie?
Ethical approaches classically hold that specific actions are moral certainties, regardless of the consequences. In line with this moral absolutism, it is always wrong to lie.
But this ethical approach would require an elderly woman with dementia who continually approaches care staff looking for their long-deceased spouse to be informed their husband has passed – the objective truth.
Distress is the likely outcome, possibly accompanied by behavioural disturbance that could endanger the person or others. The person’s memory has regressed to a point earlier in their life, when their partner was still alive. To inform such a person of the death of their spouse, however gently, is to traumatise them.
And with the memory of what they have just been told likely to quickly fade, and the questioning may resume soon after. If the truth is offered again, the cycle of re-traumatisation continues.

A different approach
Most laws are examples of absolutist ethics. One must obey the law at all times. Driving above the speed limit is likely to result in punishment regardless of whether one is in a hurry to pick their child up from kindergarten or not.
Pragmatic ethics rejects the notion certain acts are always morally right or wrong. Instead, acts are evaluated in terms of their “usefulness” and social benefit, humanity, compassion or intent.
The Aged Care Act is a set of laws intended to guide the actions of aged care providers. It says, for example, psychotropic drugs (medications that affect mind and mood) should be the “last resort” in managing the behaviours and psychological symptoms of dementia.
Instead, “best practice” involves preventing behaviour before it occurs. If one can reasonably foresee a caregiver action is likely to result in behavioural disturbance, it flies in the face of best practice.
What to say when you can’t avoid a lie?
What then, becomes the best response when approached by the lady looking for her husband?
Gentle inquiries may help uncover an underlying emotional need, and point caregivers in the right direction to meet that need. Perhaps she is feeling lonely or anxious and has become focused on her husband’s whereabouts? A skilled caregiver might tailor their response, connect with her, perhaps reminisce, and providing a sense of comfort in the process.
This approach aligns with Dementia Australia guidance that carers or loved ones can use four prompts in such scenarios:
- acknowledge concern (“I can tell you’d like him to be here.”)
- suggest an alternative (“He can’t visit right now.”)
- provide reassurance (“I’m here and lots of people care about you.”)
- redirect focus (“Perhaps a walk outside or a cup of tea?”)
These things may or may not work. So, in the face of repeated questions and escalating distress, a mistruth, such as “Don’t worry, he’ll be back soon,” may be the most humane response in the circumstances.
Different realities
It is often said you can never win an argument with a person living with dementia. A lot of time, different realities are being discussed.
So, providing someone who has dementia with a “pretend” burger may well satisfy their preferences, bring joy, mitigate the risk of malnutrition, improve social engagement, and prevent a behavioural disturbance without the use of medication. This seems like the correct approach in ethical terms. On occasion, the end justifies the means.
Steve Macfarlane, Head of Clinical Services, Dementia Support Australia, & Associate Professor of Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ghanaian Red Bean & Sweet Potato Groundnut Stew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a dish popular in principle throughout West Africa. We say “in principle” because that’s a big place, and there is a lot of regional variation. The archetypal peanut stew is from Senegal (as maafe) or Mali (as tigadèguèna), but for its more balanced nutritional profile we’ve chosen one from Ghana—and since there are regional variations within Ghana too, we should specify that this one is from the south.
If you are allergic to nuts, you can substitute a seed butter (or tahini) for the nut butter, and omit the nuts—this will work in culinary terms and be fine healthwise, but we can’t claim it would be the same dish, having lost its defining ingredient. If your allergy is solely to peanuts, then substituting with any oily nut would work. So, not almonds for example, but cashews or even walnuts would be fine.
You will need
- 1½ lbs sweet potatoes, peeled and cut into ½” cubes
- 2 cups low-sodium vegetable stock
- 2 cans kidney beans, drained, cooked, and rinsed (or 2 cups same; cooked, drained, and rinsed)
- 1 can chopped tomatoes
- ½ cup unsalted dry-roasted peanuts
- 1 onion, chopped
- 1 red bell pepper, deseeded and chopped
- ¼ bulb garlic, finely chopped
- 2 heaped tbsp unsalted peanut butter, minimal (ideally: no) additives
- 2 tsp white miso paste
- 2 tsp grated fresh ginger
- 1 tsp ground cumin
- 1 tsp cayenne pepper
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- ½ tsp coarsely ground nigella seeds
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, or other pan suitable for both frying and fitting the entire stew in. Fry the onions until softened, turn the heat down low, and add the garlic, ginger, red bell pepper, cumin, cayenne, black pepper, and MSG/salt.
2) Add ¼ cup of the vegetable stock, and the sweet potato, and turn the heat back up, on high for about 30 seconds to get it to temperature, and then take it down to a simmer.
3) Stir in the miso paste and chopped tomatoes.
4) Add most of the rest of the vegetable stock, keeping ¼ cup aside. Simmer for about 20 minutes.
5) Stir in the kidney beans, and simmer for about 30 minutes more—the sweet potato should be soft now; if it isn’t, let it simmer a while longer until it is.
6) Combine the peanut butter with the remaining ¼ cup vegetable stock, and blend until smooth. Stir it into the stew.
7) If the stew is looking more like a soup than a stew, take out 1 cup and blend this 1 cup to a purée, adding it back in.
8) Add half the peanuts unto the stew. Taste, and adjust the seasonings if necessary.
9) Crush the remaining peanuts using a pestle and mortar; not too much though; you want them broken into bits, not pulverised.
10) Garnish with the crushed nuts and nigella seeds, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we used 4/5 today!
Take care!
Share This Post
-
Lettuce vs Arugula – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lettuce to arugula, we picked the arugula.
Why?
These two salad leaves that often fulfil quite similar culinary roles (base of a green salad) are actually of different families, and it shows…
In terms of macros, arugula is lower in carbs, and much higher in protein and fiber—to the point that the protein content in arugula is almost equal to the carb content, which for leaves, is not that common a thing to see.
When it comes to vitamins, things are more even: lettuce has more of vitamins A, B1, B3, B6, and K, while arugula has more of vitamins B5, B9, C, E, and choline. All in all, we can comfortably call it a tie on the vitamin front.
In the category of minerals, things are once again more decided: arugula has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. In contrast, lettuce boasts only more selenium. An easy win for arugula.
Both of these plants have plenty of health-giving phytochemicals, including flavonoids and carotenoids along with other less talked-about things, and while the profiles are quite different for each of them, they stack up about the same in terms of overall benefits in this category.
Taking the various categories into account, this of course adds up to an easy win for arugula, but do enjoy both, especially as lettuce brings benefits that arugula doesn’t in the two categories where they tied!
Want to learn more?
You might like to read:
- How To Avoid Age-Related Macular Degeneration
- Brain Food? The Eyes Have It!
- Spinach vs Kale – Which is Healthier?
Take care!
Share This Post
-
Yes, we still need chickenpox vaccines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For people who grew up before a vaccine was available, chickenpox is largely remembered as an unpleasant experience that almost every child suffered through. The highly contagious disease tore through communities, leaving behind more than a few lasting scars.
For many children, chickenpox was much more than a week or two of itchy discomfort. It was a serious and sometimes life-threatening infection.
Prior to the chickenpox vaccine’s introduction in 1995, 90 percent of children got chickenpox. Those children grew into adults with an increased risk of developing shingles, a disease caused by the same virus—varicella-zoster—as chickenpox, which lies dormant in the body for decades.
The vaccine changed all that, nearly wiping out chickenpox in the U.S. in under three decades. The vaccine has been so successful that some people falsely believe the disease no longer exists and that vaccination is unnecessary. This couldn’t be further from the truth.
Vaccination spares children and adults from the misery of chickenpox and the serious short- and long-term risks associated with the disease. The CDC estimates that 93 percent of children in the U.S. are fully vaccinated against chickenpox. However, outbreaks can still occur among unvaccinated and under-vaccinated populations.
Here are some of the many reasons why we still need chickenpox vaccines.
Chickenpox is more serious than you may remember
For most children, chickenpox lasts around a week. Symptoms vary in severity but typically include a rash of small, itchy blisters that scab over, fever, fatigue, and headache.
However, in one out of every 4,000 chickenpox cases, the virus infects the brain, causing swelling. If the varicella-zoster virus makes it to the part of the brain that controls balance and muscle movements, it can cause a temporary loss of muscle control in the limbs that can last for months. Chickenpox can also cause other serious complications, including skin, lung, and blood infections.
Prior to the U.S.’ approval of the vaccine in 1995, children accounted for most of the country’s chickenpox cases, with over 10,000 U.S. children hospitalized with chickenpox each year.
The chickenpox vaccine is very effective and safe
Chickenpox is an extremely contagious disease. People without immunity have a 90 percent chance of contracting the virus if exposed.
Fortunately, the chickenpox vaccine provides lifetime protection and is around 90 percent effective against infection and nearly 100 percent effective against severe illness. It also reduces the risk of developing shingles later in life.
In addition to being incredibly effective, the chickenpox vaccine is very safe, and serious side effects are extremely rare. Some people may experience mild side effects after vaccination, such as pain at the injection site and a low fever.
Although infection provides immunity against future chickenpox infections, letting children catch chickenpox to build up immunity is never worth the risk, especially when a safe vaccine is available. The purpose of vaccination is to gain immunity without serious risk.
The chickenpox vaccine is one of the greatest vaccine success stories in history
It’s difficult to overstate the impact of the chickenpox vaccine. Within five years of the U.S. beginning universal vaccination against chickenpox, the disease had declined by over 80 percent in some regions.
Nearly 30 years after the introduction of the chickenpox vaccine, the disease is almost completely wiped out. Cases and hospitalizations have plummeted by 97 percent, and chickenpox deaths among people under 20 are essentially nonexistent.
Thanks to the vaccine, in less than a generation, a disease that once swept through schools and affected nearly every child has been nearly eliminated. And, unlike vaccines introduced in the early 20th century, no one can argue that improved hygiene, sanitation, and health helped reduce chickenpox cases beginning in the 1990s.
Having chickenpox as a child puts you at risk of shingles later
Although most people recover from chickenpox within a week or two, the virus that causes the disease, varicella-zoster, remains dormant in the body. This latent virus can reactivate years after the original infection as shingles, a tingling or burning rash that can cause severe pain and nerve damage.
One in 10 people who have chickenpox will develop shingles later in life. The risk increases as people get older as well as for those with weakened immune systems.
Getting chickenpox as an adult can be deadly
Although chickenpox is generally considered a childhood disease, it can affect unvaccinated people of any age. In fact, adult chickenpox is far deadlier than pediatric cases.
Serious complications like pneumonia and brain swelling are more common in adults than in children with chickenpox. One in 400 adults who get chickenpox develops pneumonia, and one to two out of 1,000 develop brain swelling.
Vaccines have virtually eliminated chickenpox, but outbreaks still happen
Although the chickenpox vaccine has dramatically reduced the impact of a once widespread disease, declining immunity could lead to future outbreaks. A Centers for Disease Control and Prevention analysis found that chickenpox vaccination rates dropped in half of U.S. states in the 2022-2023 school year compared to the previous year. And more than a dozen states have immunization rates below 90 percent.
In 2024, New York City and Florida had chickenpox outbreaks that primarily affected unvaccinated and under-vaccinated children. With declining public confidence in routine vaccines and rising school vaccine exemption rates, these types of outbreaks will likely become more common.
The CDC recommends that children receive two chickenpox vaccine doses before age 6. Older children and adults who are unvaccinated and have never had chickenpox should also receive two doses of the vaccine.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Breast Milk’s Benefits That Are (So Far) Not Replicable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Simply The Breast 🎶
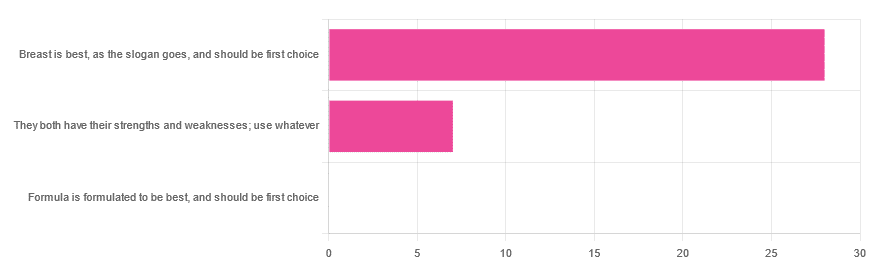
In Wednesday’s newsletter, we asked you for your opinion on breast vs formula milk (for babies!), and got the above-depicted, below-described, set of responses:
- 80% said “Breast is best, as the slogan goes, and should be first choice”
- 20% said “They both have their strengths and weaknesses; use whatever”
- 0% said “Formula is formulated to be best, and should be first choice”
That’s the first time we’ve ever had a possible poll option come back with zero votes whatsoever! It seems this topic is relatively uncontentious amongst our readership, so we’ll keep things brief today, but there is still a little mythbusting to be done.
So, what does the science say?
[Breast milk should be the first choice] at least for the few few weeks and months for the benefit of baby’s health as breast milk has protective factors formula does not: True or False?
True! The wording here was taken from one of our readers’ responses, by the way (thank you, Robin). There are a good number of those protective factors, the most well-known of which is passing on immune cells and cell-like things; in other words, immune-related information being passed from parent* to child.
*usually the mother, though in principle it could be someone else and in practice sometimes it is; the only real requirements are that the other person be healthy, lactating, and willing.
As for immune benefits, see for example:
Perspectives on Immunoglobulins in Colostrum and Milk
And for that matter, also:
(Colostrum is simply the milk that is produced for a short period after giving birth; the composition of milk will tend to change later)
In any case, immunoglobulin A is a very important component in breast milk (colostrum and later), as well as lactoferrin (has an important antimicrobial effect and is good for the newborn’s gut), and a plethora of cytokines:
As for that about the gut, lactoferrin isn’t the only breast milk component that benefits this, by far, and there’s a lot that can’t be replicated yet:
Human Breast Milk and the Gastrointestinal Innate Immune System
As long as your infant/child is nutritiously fed, it shouldn’t matter if it comes from breast or formula: True or False?
False! Formula milk will not convey those immune benefits.
This doesn’t mean that formula-feeding is neglectful; as several people who commented mentioned*, there are many reasons a person may not be able to breastfeed, and they certainly should not be shamed for that.
*(including the reader whose words we borrowed for this True/False item; the words we quoted above were prefaced with: “Not everyone is able to breastfeed for many different reasons”)
But, while formula milk is a very good second choice, and absolutely a respectable choice if breast milk isn’t an option (or an acceptable option) for whatever reason, it still does not convey all the health benefits of breast milk—yet! The day may come when they’ll find a way to replicate the immune benefits, but today is not that day.
They both have their strengths and weaknesses: True or False?
True! But formula’s strengths are only in the category of convenience and sometimes necessity—formula conveys no health benefits that breast milk could not do better, if available.
For many babies, formula means they get to eat, when without it they would starve due to non-availability of breast milk. That’s a pretty important role!
Note also: this is a health science publication, not a philosophical publication, but we’d be remiss not to mention one thing; let’s bring it in under the umbrella of sociology:
The right to bodily autonomy continues to be the right to bodily autonomy even if somebody else wants/needs something from your body.
Therefore, while there are indeed many good reasons for not being able to breastfeed, or even just not being safely* able to breastfeed, it is at the very least this writer’s opinion that nobody should be pressed to give their reason for not breastfeeding; “no” is already a sufficient answer.
*Writer’s example re safety: when I was born, my mother was on such drugs that it would have been a very bad idea for her to breastfeed me. There are plenty of other possible reasons why it might be unsafe for someone one way or another, but “on drugs that have a clear ‘do not take while pregnant or nursing’ warning” is a relatively common one.
All that said, for those who are willing and safely able, the science is clear: breast is best.
Want to read more?
The World Health Organization has a wealth of information (including explanations of its recommendations of, where possible, exclusive breastfeeding for the first 6 months, ideally continuing some breastfeeding for the first 2 years), here:
World Health Organization | Breastfeeding
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Taurine: An Anti-Aging Powerhouse? Exploring Its Unexpected Benefits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Mark Rosenberg explains:
Not a stimulant, but…
- Its presence in energy drinks often causes people to assume it’s a stimulant, but it’s not. In fact, it’s a GABA-agonist, thus having a calming effect.
- The real reason it’s in energy drinks is because it helps increase mitochondrial ATP production (ATP = adenosine triphosphate = how cells store energy that’s ready to use; mitochondria take glucose and make ATP)
- Taurine is also anti-inflammatory, antioxidant, and anticancer.
- In the category of aging, human studies are slow to give results for obvious reasons, but mouse studies show that supplementing taurine in middle-aged mice increased their lifespan by 10–12%, as well as improving various physiological markers of aging.
- Taking a closer look at aging—literally; looking at cellular aging—taurine reduces cellular senescence and protects telomeres, thus decreasing DNA mutations.
For more on the science of these, plus Dr. Rosenberg’s personal experience, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Taurine’s Benefits For Heart Health And More
- Dr. Greger’s Anti-Aging Eight
- Age & Aging: What Can (And Can’t) We Do About It?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Best Workouts for Women Over 40 To Give Your Metabolism A Makeover
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After 40, the usual course of events goes: your lean muscle mass decreases, which slows your metabolism and makes it easier to gain fat. At the same time, bone density decreases, increasing the risk of osteoporosis and frailty. This leads to lower mobility, flexibility, and overall frustration.
But it doesn’t have to be that way! Fitness coach Jessica Cooke explains how:
It all depends on this
Strength training helps counteract these effects by increasing lean muscle mass, which boosts metabolism and fat burning. It also improves bone density, reducing the risk of osteoporosis. Plus, it builds strength, fitness, and a toned physique.
The best part? It doesn’t require long workouts—short, effective sessions work best.
While walking is very beneficial for general health, it doesn’t provide the resistance needed to build muscle. Without resistance, your body composition won’t change, and so your metabolism will remain the same. Strength training is essential for burning fat at rest and improving overall fitness.
You don’t have to do high-impact exercises or jumping to see results. Low-impact strength training is effective and gentle on the joints. Lifting weights or using your body weight in a controlled manner will help build muscle and improve strength.
Many women only do cardio and neglect strength training, leading to minimal progress. Another common mistake is overcomplicating workouts—simple, consistent strength training is all you need.
Aim to strength train three times per week for 20 minutes. Focus on compound movements that work multiple muscle groups, such as:
- squats
- lunges
- deadlifts
- press-ups
- shoulder presses
- upright rows
- planks
- glute bridges
- sit-ups
- Russian twists
Start with light (e.g. 2-3 kg) weights and maintain proper form.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Don’t Let Menopause Run You Down: 4 Critical Things Female Runners Should Know
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: