I have a stuffy nose, how can I tell if it’s hay fever, COVID or something else?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hay fever (also called allergic rhinitis) affects 24% of Australians. Symptoms include sneezing, a runny nose (which may feel blocked or stuffy) and itchy eyes. People can also experience an itchy nose, throat or ears.
But COVID is still spreading, and other viruses can cause cold-like symptoms. So how do you know which one you’ve got?

Remind me, how does hay fever cause symptoms?
Hay fever happens when a person has become “sensitised” to an allergen trigger. This means a person’s body is always primed to react to this trigger.
Triggers can include allergens in the air (such as pollen from trees, grasses and flowers), mould spores, animals or house dust mites which mostly live in people’s mattresses and bedding, and feed on shed skin.
When the body is exposed to the trigger, it produces IgE (immunoglobulin E) antibodies. These cause the release of many of the body’s own chemicals, including histamine, which result in hay fever symptoms.
People who have asthma may find their asthma symptoms (cough, wheeze, tight chest or trouble breathing) worsen when exposed to airborne allergens. Spring and sometimes into summer can be the worst time for people with grass, tree or flower allergies.
However, animal and house dust mite symptoms usually happen year-round.

What else might be causing my symptoms?
Hay fever does not cause a fever, sore throat, muscle aches and pains, weakness, loss of taste or smell, nor does it cause you to cough up mucus.
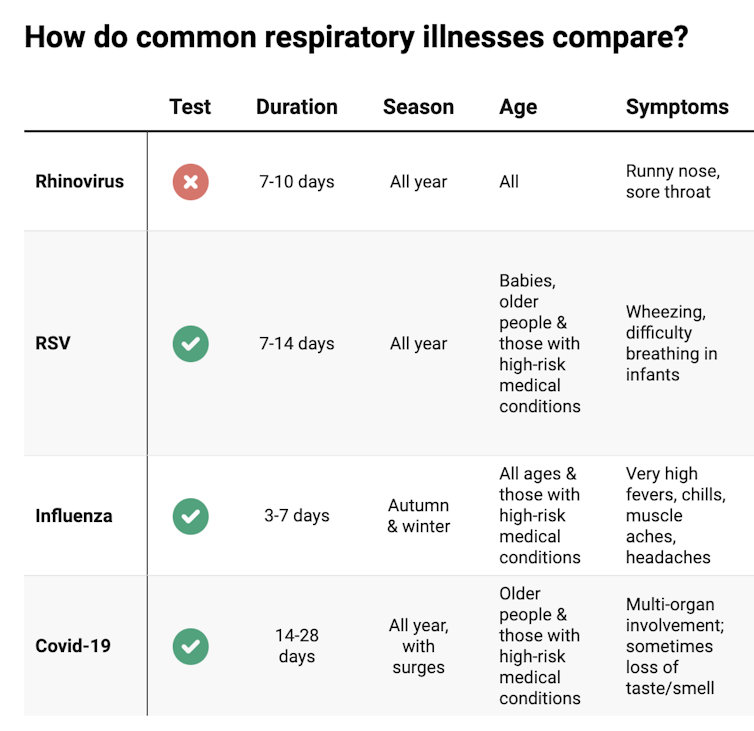
These symptoms are likely to be caused by a virus, such as COVID, influenza, respiratory syncytial virus (RSV) or a “cold” (often caused by rhinoviruses). These conditions can occur all year round, with some overlap of symptoms:
COVID still surrounds us. RSV and influenza rates appear higher than before the COVID pandemic, but it may be due to more testing.
So if you have a fever, sore throat, muscle aches/pains, weakness, fatigue, or are coughing up mucus, stay home and avoid mixing with others to limit transmission.
People with COVID symptoms can take a rapid antigen test (RAT), ideally when symptoms start, then isolate until symptoms disappear. One negative RAT alone can’t rule out COVID if symptoms are still present, so test again 24–48 hours after your initial test if symptoms persist.
You can now test yourself for COVID, RSV and influenza in a combined RAT. But again, a negative test doesn’t rule out the virus. If your symptoms continue, test again 24–48 hours after the previous test.
If it’s hay fever, how do I treat it?
Treatment involves blocking the body’s histamine release, by taking antihistamine medication which helps reduce the symptoms.
Doctors, nurse practitioners and pharmacists can develop a hay fever care plan. This may include using a nasal spray containing a topical corticosteroid to help reduce the swelling inside the nose, which causes stuffiness or blockage.
Nasal sprays need to delivered using correct technique and used over several weeks to work properly. Often these sprays can also help lessen the itchy eyes of hay fever.
Drying bed linen and pyjamas inside during spring can lessen symptoms, as can putting a smear of Vaseline in the nostrils when going outside. Pollen sticks to the Vaseline, and gently blowing your nose later removes it.
People with asthma should also have an asthma plan, created by their doctor or nurse practitioner, explaining how to adjust their asthma reliever and preventer medications in hay fever seasons or on allergen exposure.
People with asthma also need to be alert for thunderstorms, where pollens can burst into tinier particles, be inhaled deeper in the lungs and cause a severe asthma attack, and even death.
What if it’s COVID, RSV or the flu?
Australians aged 70 and over and others with underlying health conditions who test positive for COVID are eligible for antivirals to reduce their chance of severe illness.
Most other people with COVID, RSV and influenza will recover at home with rest, fluids and paracetamol to relieve symptoms. However some groups are at greater risk of serious illness and may require additional treatment or hospitalisation.
For RSV, this includes premature infants, babies 12 months and younger, children under two who have other medical conditions, adults over 75, people with heart and lung conditions, or health conditions that lessens the immune system response.
For influenza, people at higher risk of severe illness are pregnant women, Aboriginal people, people under five or over 65 years, or people with long-term medical conditions, such as kidney, heart, lung or liver disease, diabetes and decreased immunity.
If you’re concerned about severe symptoms of COVID, RSV or influenza, consult your doctor or call 000 in an emergency.
If your symptoms are mild but persist, and you’re not sure what’s causing them, book an appointment with your doctor or nurse practitioner. Although hay fever season is here, we need to avoid spreading other serious infectious.
For more information, you can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria); use the online Symptom Checker; or visit healthdirect.gov.au or the Australian Society of Clinical Immunology and Allergy.
Deryn Thompson, Eczema and Allergy Nurse; Lecturer, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Barley Malt Flour vs chickpea flour – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing barley malt flour to chickpea flour, we picked the chickpea.
Why?
First, some notes:
About chickpea flour: this is also called besan flour, gram flour, and garbanzo bean flour; they are all literally the same thing by different names, and are all flour made from ground chickpeas.
About barley malt flour: barley is a true grain, and does contain gluten. We’re not going to factor that into today’s decision, but if you are avoiding gluten, avoid barley. As for “malt”; malting grains means putting them in an environment (with appropriate temperature and humidity) that they can begin germination, and then drying them with hot air to stop the germination process from continuing, so that we still have grains to make flour out of, and not little green sprouting plants. It improves the nutritional qualities and, subjectively, the flavor.
To avoid repetition, we’re just going to write “barley” instead of “barley malt” now, but it’s still malted.
Now, let’s begin:
Looking at the macros first, chickpea flour has 2x the protein and also more fiber, while barley flour has more carbs. An easy win for chickpea flour.
In the category of vitamins, chickpea flour has more of vitamins A, B1, B5, B9, E, and K, while barley flour has more of vitamins B2, B3, B6, and C. A modest 6:4 victory for chickpea flour.
When it comes to minerals, things are much more one-sided; chickpea flour has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while barley flour has more selenium. An overwhelming win for chickpea flour.
Adding up these three wins for chickpea flour makes for a convincing story in favor of using that where reasonably possible as a flour! It has a slight nutty taste, so you might not want to use it in everything, but it is good for a lot of things.
Want to learn more?
You might like to read:
- Grains: Bread Of Life, Or Cereal Killer?
- Gluten: What’s The Truth?
- Sprout Your Seeds, Grains, Beans, Etc
Take care!
Share This Post
-
‘Emergency’ or Not, Covid Is Still Killing People. Here’s What Doctors Advise to Stay Safe.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With around 20,000 people dying of covid in the United States since the start of October, and tens of thousands more abroad, the covid pandemic clearly isn’t over. However, the crisis response is, since the World Health Organization and the Biden administration ended their declared health emergencies last year.
Let’s not confuse the terms “pandemic” and “emergency.” As Abraar Karan, an infectious disease physician and researcher at Stanford University, said, “The pandemic is over until you are scrunched in bed, feeling terrible.”
Pandemics are defined by neither time nor severity, but rather by large numbers of ongoing infections worldwide. Emergencies are acute and declared to trigger an urgent response. Ending the official emergency shifted the responsibility for curbing covid from leaders to the public. In the United States, it meant, for example, that the government largely stopped covering the cost of covid tests and vaccines.
But the virus is still infecting people; indeed, it is surging right now.
With changes in the nature of the pandemic and the response, KFF Health News spoke with doctors and researchers about how to best handle covid, influenza, and other respiratory ailments spreading this season.
A holiday wave of sickness has ensued as expected. Covid infections have escalated nationwide in the past few weeks, with analyses of virus traces in wastewater suggesting infection rates as high as last year’s. More than 73,000 people died of covid in the U.S. in 2023, meaning the virus remains deadlier than car accidents and influenza. Still, compared with last year’s seasonal surge, this winter’s wave of covid hospitalizations has been lower and death rates less than half.
“We’re seeing outbreaks in homeless shelters and in nursing homes, but hospitals aren’t overwhelmed like they have been in the past,” said Salvador Sandoval, a doctor and health officer at the Merced County public health department in California. He attributes that welcome fact to vaccination, covid treatments like Paxlovid, and a degree of immunity from prior infections.
While a new coronavirus variant, JN.1, has spread around the world, the current vaccines and covid tests remain effective.
Other seasonal illnesses are surging, too, but rates are consistent with those of previous years. Between 9,400 and 28,000 people died from influenza from Oct. 1 to Jan. 6, estimates the Centers for Disease Control and Prevention, and millions felt so ill from the flu that they sought medical care. Cases of pneumonia — a serious condition marked by inflamed lungs that can be triggered by the flu, covid, or other infections — also predictably rose as winter set in. Researchers are now less concerned about flare-ups of pneumonia in China, Denmark, and France in November and December, because they fit cyclical patterns of the pneumonia-causing bacteria Mycoplasma pneumoniae rather than outbreaks of a dangerous new bug.
Public health researchers recommend following the CDC guidance on getting the latest covid and influenza vaccines to ward off hospitalization and death from the diseases and reduce chances of getting sick. A recent review of studies that included 614,000 people found that those who received two covid vaccines were also less likely to develop long covid; often involving fatigue, cognitive dysfunction, and joint pain, the condition is marked by the development or continuation of symptoms a few months after an infection and has been debilitating for millions of people. Another analysis found that people who had three doses of covid vaccines were much less likely to have long covid than those who were unvaccinated. (A caveat, however, is that those with three doses might have taken additional measures to avoid infections than those who chose to go without.)
It’s not too late for an influenza vaccine, either, said Helen Chu, a doctor and epidemiologist at the University of Washington in Seattle. Influenza continues to rise into the new year, especially in Southern states and California. Last season’s shot appeared to reduce adults’ risk of visits to the emergency room and urgent care by almost half and hospitalization by more than a third. Meanwhile, another seasonal illness with a fresh set of vaccines released last year, respiratory syncytial virus, appears to be waning this month.
Another powerful way to prevent covid, influenza, common colds, and other airborne infections is by wearing an N95 mask. Many researchers say they’ve returned to socializing without one but opt for the masks in crowded, indoor places when wearing one would not be particularly burdensome. Karan, for example, wears his favorite N95 masks on airplanes. And don’t forget good, old-fashioned hand-washing, which helps prevent infections as well.
If you do all that and still feel sick? Researchers say they reach for rapid covid tests. While they’ve never been perfect, they’re often quite helpful in guiding a person’s next steps.
When President Joe Biden declared the end of the public health emergency last year, many federally funded testing sites that sent samples to laboratories shut their doors. As a result, people now mainly turn to home covid tests that signal an infection within 15 minutes and cost around $6 to $8 each at many pharmacies. The trick is to use these tests correctly by taking more than one when there’s reason for concern. They miss early infections more often than tests processed in a lab, because higher levels of the coronavirus are required for detection — and the virus takes time to multiply in the body. For this reason, Karan considers other information. “If I ran into someone who turned out to be sick, and then I get symptoms a few days later,” he said, “the chance is high that I have whatever they had, even if a test is negative.”
A negative result with a rapid test might mean simply that an infection hasn’t progressed enough to be detected, that the test had expired, or that it was conducted wrong. To be sure the culprit behind symptoms like a sore throat isn’t covid, researchers suggest testing again in a day or two. It often takes about three days after symptoms start for a test to register as positive, said Karan, adding that such time estimates are based on averages and that individuals may deviate from the norm.
If a person feels healthy and wants to know their status because they were around someone with covid, Karan recommends testing two to four days after the exposure. To protect others during those uncertain days, the person can wear an N95 mask that blocks the spread of the virus. If tests remain negative five days after an exposure and the person still feels fine, Chu said, they’re unlikely to be infected — and, if they are, viral levels would be so low that they would be unlikely to pass the disease to others.
Positive tests, on the other hand, reliably flag an infection. In this case, people can ask a doctor whether they qualify for the antiviral drug Paxlovid. The pills work best when taken immediately after symptoms begin so that they slash levels of the virus before it damages the body. Some studies suggest the medicine reduces a person’s risk of long covid, too, but the evidence is mixed. Another note on tests: Don’t worry if they continue to turn out positive for longer than symptoms last; the virus may linger even if it’s no longer replicating. After roughly a week since a positive test or symptoms, studies suggest, a person is unlikely to pass the virus to others.
If covid is ruled out, Karan recommends tests for influenza because they can guide doctors on whether to prescribe an antiviral to fight it — or if instead it’s a bacterial infection, in which case antibiotics may be in order. (One new home test diagnoses covid and influenza at the same time.) Whereas antivirals and antibiotics target the source of the ailment, over-the-counter medications may soothe congestion, coughs, fevers, and other symptoms. That said, the FDA recently determined that a main ingredient in versions of Sudafed, NyQuil, and other decongestants, called phenylephrine, is ineffective.
Jobs complicate a personal approach to staying healthy. Emergency-era business closures have ended, and mandates on vaccination and wearing masks have receded across the country. Some managers take precautions to protect their staff. Chu, for example, keeps air-purifying devices around her lab, and she asks researchers to stay home when they feel sick and to test themselves for covid before returning to work after a trip.
However, occupational safety experts note that many employees face risks they cannot control because decisions on if and how to protect against outbreaks, such as through ventilation, testing, and masking, are left to employers. Notably, people with low-wage and part-time jobs — occupations disproportionately held by people of color — are often least able to control their workplace environments.
Jessica Martinez, co-executive director of the National Council for Occupational Safety and Health, said the lack of national occupational standards around airborne disease protection represents a fatal flaw in the Biden administration’s decision to relinquish its control of the pandemic.
“Every workplace needs to have a plan for reducing the threat of infectious disease,” she said. “If you only focus on the individual, you fail workers.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
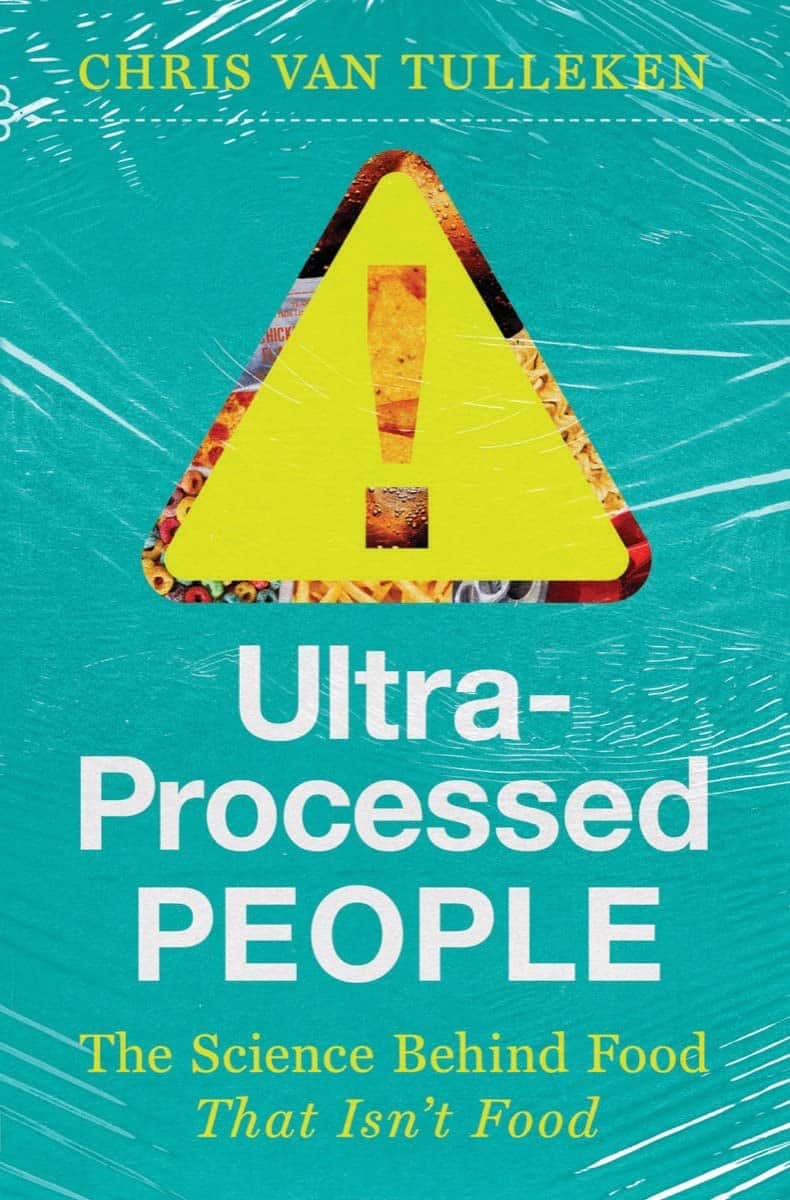
Ultra-Processed People – by Dr. Chris van Tulleken
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It probably won’t come as a great surprise to any of our readers that ultra-processed food is—to make a sweeping generalization—not fabulous for the health. So, what does this book offer beyond that?
Perhaps this book’s greatest strength is in showing not just what ultra-processed foods are, but why they are. In principle, food being highly processed should be neither good nor bad by default. Much like GMOs, if a food is modified to be more nutritious, that should be good, right?
Only, that’s mostly not what happens. What happens instead is that food is modified (be it genetically or by ultra-processing) to be cheaper to produce, and thus maximise the profit margin.
The addition of a compound that increases shelf-life but harms the health, increases sales and is a net positive for the manufacturer, for instance. Dr. van Tulleken offers us many, many, examples and explanations of such cost-cutting strategies at our expense.
In terms of qualifications, the author has an MD from Oxford, and also a PhD, but the latter is in molecular virology; not so relevant here. Yet, we are not expected to take an “argument from authority”, and instead, Dr. van Tulleken takes great pains to go through a lot of studies with us—the good, the bad, and the misleading.
If the book has a downside, then this reviewer would say it’s in the format; it’s less a reference book, and more a 384-page polemic. But, that’s a subjective criticism, and for those who like that sort of thing, that is the sort of thing that they like.
Share This Post
Related Posts
-
Can apps and digital resources support your child with autism or ADHD?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Neurodevelopmental conditions such as attention deficit hyperactivity disorder (ADHD) and autism affect about one in ten children. These conditions impact development, behaviour and wellbeing.
But children with these conditions and their caregivers often can’t get the support they need. Families report difficulties accessing health-care providers and experience long wait lists to receive care.
Digital tools, such as apps and websites, are often viewed as a solution to these gaps. With a single click or a download, families might be able to access information to support their child.
There are lots of digital tools available, but it’s hard to know what is and isn’t useful. Our new study evaluated freely available digital resources for child neurodevelopment and mental health to understand their quality and evidence base.
We found many resources were functional and engaging. However, resources often lacked evidence for the information provided and the claimed positive impact on children and families.
This is a common problem in the digital resource field, where the high expectations and claims of impact from digital tools to change health care have not yet been realised.
Fabio Principe/Shutterstock What type of resources?
Our study identified 3,435 separate resources, of which 112 (43 apps and 69 websites) met our criteria for review. These resources all claimed to provide information or supports for child neurodevelopment, mental health or wellbeing.
Resources had to be freely available, in English and have actionable information for children and families.
The most common focus was on autism, representing 17% of all resources. Resources suggested they provided strategies to promote speech, language and social development, and to support challenging behaviours.
Other common areas included language and communication (14%), and ADHD (10%).
Resources had various purposes, including journalling and providing advice, scheduling support, and delivering activities and strategies for parents. Resources delivered information interactively, with some apps organising content into structured modules.
Resources also provided options for alternative and assistive communication for people with language or communication challenges.
Most apps were functional and accessible
Our first question was about how engaging and accessible the information was. Resources that are hard to use aren’t used frequently, regardless of the information quality.
We evaluated aesthetics, including whether digital tools were easy to use and navigate, stylistically consistent, with clean and appealing graphics for users.
Most resources were rated as highly engaging, with strong accessibility and functionality.
Most apps and websites we evaluated were engaging. jamesteohart/Shutterstock But many lacked quality information
We ranked resources on various features from 1 (inadequate) to 5 (excellent), with a ranking of 3 considered acceptable. These ratings looked at how credible the resource was and whether there was evidence supporting it.
Despite their functionality, 37% of reviewed apps did not meet the minimum acceptable standards for information quality. This means many apps could not be recommended. Most websites fared better than apps.
There also wasn’t a lot of scientific evidence to suggest using either apps or digital resources actually helped families. Studies show long-term engagement with digital tools is rare, and downloads don’t correspond to frequent usage or benefits.
Digital tools are often viewed as a panacea to health-care gaps, but the evidence is yet to show they fill such gaps. Digital health is a fast-moving field and resources are often made available before they have been properly evaluated.
What should you look for in digital resources?
We found the highest quality resources were developed in collaboration with institutions, such as health, university or government groups.
One highly rated resource was the Raising Children’s Network and the associated app, Raising Healthy Minds. These are co-developed with a university and hospital, and by people with appropriate qualifications.
This resource provides information to support children’s overall health, development and wellbeing, with dedicated sections addressing neurodevelopmental needs and concerns.
The Raising Children Network provides resources for child health, including neurodevelopmental needs. Raising Children Network screenshot Our research shows parents can assess whether digital resources are high quality by checking they are:
- factually correct. Look for where the app or resource is getting its information. Does the author have the qualifications and training to provide the information? Are they a registered health expert who is accountable to a regulatory body (such as AHPRA, the Australian Health Practitioners Regulation Agency) for providing information that does not cause harm?
- consistent across multiple credible sources, such as health institutions.
- linked to supporting information. Look for reliable links to reputable institutions. Links to peer-reviewed scientific journals are often helpful as those articles will also usually describe the limitations of the research presented.
- up-to-date. Apps should be frequently updated. For websites, dates of update are usually found on the homepage or at the bottom of individual pages.
Check when information was last updated. fizkes/Shutterstock Beware of red flags
Some things to watch out for are:
- testimonials and anecdotes without evidence and scientific links to back the anecdotes up. If it sounds too good to be true, it probably is.
- no information provided about conflicts of interest. Organisations gain when you click on their links or take their advice (financial, reputation and brand development). Think about what they gain when you use their information to help keep a balanced perspective.
Remember, the app’s star rating doesn’t mean it will contain factual information from a reliable source or be helpful for you and your child.
The role of digital tools
Digital tools won’t usually replace a health professional, but they can support care in many different ways. They may be used to help to educate and prepare for meetings, and to collaborate with health providers.
They may also be used to collect information about daily needs. Studies show reporting on sleep in children can be notoriously difficult, for example. But tracking sleep behaviour with actigraphy, where movement and activity patterns are measured using a wearable device, can provide information to support clinical care. With the promise of artificial intelligence, there will also be new opportunities to support daily living.
Our findings reflect a broader problem for digital health, however. Much investment is often made in developing products to drive use, with spurious claims of health benefits.
What’s needed is a system that prioritises the funding, implementation and evaluation of tools to demonstrate benefits for families. Only then may we realise the potential of digital tools to benefit those who use them.
Kelsie Boulton, Senior Research Fellow in Child Neurodevelopment, Brain and Mind Centre, University of Sydney and Adam Guastella, Professor and Clinical Psychologist, Michael Crouch Chair in Child and Youth Mental Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
You can thaw and refreeze meat: five food safety myths busted
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This time of year, most fridges are stocked up with food and drinks to share with family and friends. Let’s not make ourselves and our guests sick by getting things wrong when preparing and serving food.
As the weather warms up, so does the environment for micro-organisms in foods, potentially allowing them to multiply faster to hazardous levels. So put the drinks on ice and keep the fridge for the food.
But what are some of those food safety myths we’ve long come to believe that aren’t actually true?
Myth 1: if you’ve defrosted frozen meat or chicken you can’t refreeze it
From a safety point of view, it is fine to refreeze defrosted meat or chicken or any frozen food as long as it was defrosted in a fridge running at 5°C or below. Some quality may be lost by defrosting then refreezing foods as the cells break down a little and the food can become slightly watery.
Another option is to cook the defrosted food and then divide into small portions and refreeze once it has stopped steaming. Steam in a closed container leads to condensation, which can result in pools of water forming. This, combined with the nutrients in the food, creates the perfect environment for microbial growth. So it’s always best to wait about 30 minutes before refrigerating or freezing hot food.
Plan ahead so food can be defrosted in the fridge, especially with large items such as a frozen turkey or roll of meat. If left on the bench, the external surface could be at room temperature and micro-organisms could be growing rapidly while the centre of the piece is still frozen!
Myth 2: Wash meat before you prepare and/or cook it
It is not a good idea to wash meats and poultry when preparing for cooking. Splashing water that might contain potentially hazardous bacteria around the kitchen can create more of a hazard if those bacteria are splashed onto ready-to-eat foods or food preparation surfaces.
It is, however, a good idea to wash fruits and vegetables before preparing and serving, especially if they’re grown near or in the ground as they may carry some dirt and therefore micro-organisms.
This applies particularly to foods that will be prepared and eaten without further cooking. Consuming foods raw that traditionally have been eaten cooked or otherwise processed to kill pathogenic micro-organisms (potentially deadly to humans) might increase the risk of food poisoning.
Fruit, salad, vegetables and other ready-to-eat foods should be prepared separately, away from raw meat, chicken, seafood and other foods that need cooking.
Myth 3: Hot food should be left out to cool completely before putting it in the fridge
It’s not OK to leave perishable food out for an extended time or overnight before putting it in the fridge.
Micro-organisms can grow rapidly in food at temperatures between 5° and 60°C. Temperature control is the simplest and most effective way of controlling the growth of bacteria. Perishable food should spend as little time as possible in the 5-60°C danger zone. If food is left in the danger zone, be aware it is potentially unsafe to eat.
Hot leftovers, and any other leftovers for that matter, should go into the fridge once they have stopped steaming to reduce condensation, within about 30 minutes.
Large portions of hot food will cool faster if broken down into smaller amounts in shallow containers. It is possible that hot food such as stews or soup left in a bulky container, say a two-litre mixing bowl (versus a shallow tray), in the fridge can take nearly 24 hours to cool to the safe zone of less than 5°C.
Myth 4: If it smells OK, then it’s OK to eat
This is definitely not always true. Spoilage bacteria, yeasts and moulds are the usual culprits for making food smell off or go slimy and these may not make you sick, although it is always advisable not to consume spoiled food.
Pathogenic bacteria can grow in food and not cause any obvious changes to the food, so the best option is to inhibit pathogen growth by refrigerating foods.
Myth 5: Oil preserves food so it can be left at room temperature
Adding oil to foods will not necessarily kill bugs lurking in your food. The opposite is true for many products in oil if anaerobic micro-organisms, such as Clostridium botulinum (botulism), are present in the food. A lack of oxygen provides perfect conditions for their growth.
Outbreaks of botulism arising from consumption of vegetables in oil – including garlic, olives, mushrooms, beans and hot peppers – have mostly been attributed to the products not being properly prepared.
Vegetables in oil can be made safely. In 1991, Australian regulations stipulated that this class of product (vegetables in oil) can be safely made if the pH (a measure of acid) is less than 4.6. Foods with a pH below 4.6 do not in general support the growth of food-poisoning bacteria including botulism.
So keep food out of the danger zone to reduce your guests’ risk of getting food poisoning this summer. Check out other food safety tips and resources from CSIRO and the Food Safety Information Council, including testing your food safety knowledge.
Cathy Moir, Team leader, Microbial and chemical sciences, Food microbiologist and food safety specialist, CSIRO
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Science of Pilates – by Tracy Ward
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other books in this series, “Science of Yoga” and “Science of HIIT” (they’re great too; check them out!). What does this one add to the mix?
Pilates is a top-tier “combination exercise” insofar as it checks a lot of boxes, e.g:
- Strength—especially core strength, but also limbs
- Mobility—range of motion and resultant reduction in injury risk
- Stability—impossible without the above two things, but Pilates trains this too
- Fitness—many dynamic Pilates exercises can be performed as cardio and/or HIIT.
The author, a physiotherapist, explains (as the title promises!) the science of Pilates, with:
- the beautifully clear diagrams we’ve come to expect of this series,
- equally clear explanations, with a great balance of simplicity of terms and depth where necessary, and
- plenty of citations for the claims made, linking to lots of the best up-to-date science.
Bottom line: if you are in a position to make a little time for Pilates (if you don’t already), then there is nobody who would not benefit from reading this book.
Click here to check out Science of Pilates, and keep your body well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: