How to Think Like Leonardo da Vinci – by Michael J. Gelb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Authors often try to bring forward the best minds of the distant past, and apply them to today’s world. One could fill a library with business advice adaptations from Sun Tzu’s Art of War alone, same goes for Miyamoto Musashi’s Book of Five Rings, and let’s not get started on Niccolò Machiavelli. What makes this book different?
Michael Gelb explores the principles codified and used by the infamous Renaissance Man to do exactly what he did: pretty much everything. Miyamoto Musashi had no interest in business, but Leonardo da Vinci really did care a lot about learning, creating, problem-solving, human connections, and much more. And best of all, he took notes. So many notes, for himself, of which we now enjoy the benefit.
How To Think Like Leonardo da Vinci explores these notes and their application by the man himself, and gives real, practical examples of how you can (and why you should) put them into action in your daily life, no matter whether you are a big business CEO or a local line cook or a reclusive academic, Leonardo has lessons for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Good Life – by Robert Waldinger, MD, and Marc Schulz, PhD
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For any who have thought “there must be some middle-ground between entirely subjective self-help books advising how to feel better, and sifting through clinical data on what actually affects people’s moods“, this book is exactly that middle-ground!
Drs. Waldinger and Schultz went through the 80-year-long Harvard Study of Adult Development with a fine-toothed comb, and this book details—more readably—what they found.
There are frequent references to data from the study. Not just numbers, though, people’s answers to questions, too. And how different factors about people’s lives affected their answers to the same questions.
We hear from all ages, from young adults to octagenarians, and learn how attitudes (including: of the same people) change over time. Not because people are fickle, but because people grow… or become disillusioned. Or sometimes, both.
We learn about the importance of money… And where that importance ends.
We learn importance of relationships of various kinds, and this is certainly a recurring theme throughout the study—and thus, throughout the book.
The book doesn’t just present data, though, it also presents actionable insights along the way.
Bottom line: the combined wisdom and life-experiences of a lot of people provide a very “big picture” view of life, and what makes us happy, really. We highly recommend it!
Share This Post
-
8 Signs Of Iodine Deficiency You Might Not Expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Coach Kait (BSc Nutrition & Exercise) is a certified health and nutrition coach, and today she’s here to talk about iodine—which is important for many of our body functions, from thyroid hormone production to metabolic regulation to heart rate management, as well as more superficial-but-important-too things like our skin and hair.
Kait’s hitlist
Here’s what she recommends we look out for:
- Swollen neck: even a slightly swollen neck might indicate low iodine levels (this is because that’s where the thyroid glands are)
- Hair loss: iodine is needed for healthy hair growth, so a deficiency can lead to hair loss / thinning hair
- Dry and flaky skin: with iodine’s role in our homeostatic system not being covered, our skin can dry out as a result
- Feeling cold all the time: because of iodine’s temperature-regulating activities
- Slow heart rate: A metabolic slump due to iodine deficiency can slow down the heart rate, leading to fatigue and weakness (and worse, if it persists)
- Brain fog: trouble focusing can be a symptom of the same metabolic slump
- Fatigue: this is again more or less the same thing, but she said eight signs, so we’re giving you the eight!
- Irregular period (if you normally have such, of course): because iodine affects reproductive hormones too, an imbalance can disrupt menstrual cycles.
For more on each of these, as well as how to get more iodine in your diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might also like to read:
- A Fresh Take On Hypothyroidism
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Eat To Beat Hyperthyroidism!
Take care!
Share This Post
-
Functional Exercise For Seniors – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of exercises books are tailored to 20-year-old athletes training for their first Tough Mudder. Others, that the only thing standing between us and a perfect Retroflex Countersupine Divine Pretzel position is a professionally-lit Instagrammable photo.
This one’s not like that.
But! Nor does it think being over a certain age is a reason to not have genuinely robust health, of the kind that may make some younger people envious. So, it lays out, in progressive format, guidelines for exercises targeted at everything we need to build and maintain as we get older.
The writing style is clear, and the illustrations too (the cover art is the same style as the illustrations inside).
Bottom line: if you’re looking for a workout guide that understands you are nearer 80 than 18, and/but also doesn’t assume your age limits your exercise potential to “wrist exercises in chair”, then this book is a fine pick.
Share This Post
Related Posts
-
Junk Food Turns Public Villain as Power Shifts in Washington
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The new Trump administration could be coming for your snacks.
For years, the federal government has steered clear of regulating junk food, fast food, and ultra-processed food.
Now attitudes are changing. Some members of President-elect Donald Trump’s inner circle are gearing up to battle “Big Food,” or the companies that make most of the food and beverages consumed in the United States. Nominees for top health agencies are taking aim at ultra-processed foods that account for an estimated 70% of the nation’s food supply. Based on recent statements, a variety of potential politically charged policy options to regulate ultra-processed food may land on the Trump team menu, including warning labels, changes to agribusiness subsidies, and limits on which products consumers can buy with government food aid.
The push to reform the American diet is being driven largely by conservatives who have taken up the cause that has long been a darling of the left. Trump supporters such as Robert F. Kennedy Jr., whose controversial nomination to lead the Department of Health and Human Services still faces Senate confirmation, are embracing a concept that champions natural foods and alternative medicine. It’s a movement they’ve dubbed “MAHA,” or Make America Healthy Again. Their interest has created momentum because their goals have fairly broad bipartisan support even amid a bitterly divided Congress in which lawmakers from both sides of the aisle focused on the issue last year.
It’s likely to be a pitched battle because the food industry wields immense political influence and has successfully thwarted previous efforts to regulate its products or marketing. The category of “food processing and sales companies,” which includes Tyson Foods and Nestle SA, tallied $26.7 million in spending on lobbying in 2024, according to OpenSecrets. That’s up from almost $10 million in 1998.
“They have been absolutely instrumental and highly, highly successful at delaying any regulatory effectiveness in America,” said Laura Schmidt, a health policy professor at the University of California-San Francisco. “It really does feel like there needs to be a moment of reckoning here where people start asking the question, ‘Why do we have to live like this?’”
“Ultra-processed food” is a widely used term that means different things to different people and is used to describe items ranging from sodas to many frozen meals. These products often contain added fats, starches, and sugars, among other things. Researchers say consumption of ultra-processed foods is linked — in varying levels of intensity — to chronic conditions like diabetes, cancer, mental health problems, and early death.
Nutrition and health leaders are optimistic that a reckoning is already underway. Kennedy has pledged to remove processed foods from school lunches, restrict certain food additives such as dyes in cereal, and shift federal agricultural subsidies away from commodity crops widely used in ultra-processed foods.
The intensifying focus in Washington has triggered a new level of interest on the legal front as lawyers explore cases to take on major foodmakers for selling products they say result in chronic disease.
Bryce Martinez, now 18, filed a lawsuit in December against almost a dozen foodmakers such as Kraft Heinz, The Coca-Cola Co., and Nestle USA. He developed diabetes and non-alcoholic fatty liver disease by age 16, and is seeking to hold them accountable for his illnesses. According to the suit, filed in the Philadelphia Court of Common Pleas, the companies knew or should have known ultra-processed foods were harmful and addictive.
The lawsuit noted that Martinez grew up eating heavily advertised, brand-name foods that are staples of the American diet — sugary soft drinks, Cheerios and Lucky Charms, Skittles and Snickers, frozen and packaged dinners, just to name a few.
Nestle, Coca-Cola, and Kraft Heinz didn’t return emails seeking comment for this article. The Consumer Brands Association, a trade association for makers of consumer packaged goods, disputed the allegations.
“Attempting to classify foods as unhealthy simply because they are processed, or demonizing food by ignoring its full nutrient content, misleads consumers and exacerbates health disparities,” said Sarah Gallo, senior vice president of product policy, in a statement.
Other law firms are on the hunt for children or adults who believe they were harmed by consuming ultra-processed foods, increasing the likelihood of lawsuits.
One Indiana personal injury firm says on its website that “we are actively investigating ultra processed food (UPF) cases.” Trial attorneys in Texas also are looking into possible legal action against the federal regulators they say have failed to police ultra-processed foods.
“If you or your child have suffered health problems that your doctor has linked directly to the consumption of ultra-processed foods, we want to hear your story,” they say on their website.
Meanwhile, the FDA on Jan. 14 announced it is proposing to require a front-of-package label to appear on most packaged foods to make information about a food’s saturated fat, sodium, and added sugar content easily visible to consumers.
And on Capitol Hill, Sens. Bernie Sanders (I-Vt.), Ron Johnson (R-Wis.), and Cory Booker (D-N.J.) are sounding the alarm over ultra-processed food. Sanders introduced legislation in 2024 that could lead to a federal ban on junk food advertising to children, a national education campaign, and labels on ultra-processed foods that say the products aren’t recommended for children. Booker cosigned the legislation along with Sens. Peter Welch (D-Vt.) and John Hickenlooper (D-Colo.).
The Senate Committee on Health, Education, Labor and Pensions held a December hearing examining links between ultra-processed food and chronic disease during which FDA Commissioner Robert Califf called for more funding for research.
Food companies have tapped into “the same neural circuits that are involved in opioid addiction,” Califf said at the hearing.
Sanders, who presided over the hearing, said there’s “growing evidence” that “these foods are deliberately designed to be addictive,” and he asserted that ultra-processed foods have driven epidemics of diabetes and obesity, and hundreds of billions of dollars in medical expenses.
Research on food and addiction “has accumulated to the point where it’s reached a critical mass,” said Kelly Brownell, an emeritus professor at Stanford who is one of the editors of a scholarly handbook on the subject.
Attacks from three sides — lawyers, Congress, and the incoming Trump administration, all seemingly interested in taking up the fight — could lead to enough pressure to challenge Big Food and possibly spur better health outcomes in the U.S., which has the lowest life expectancy among high-income countries.
“Maybe getting rid of highly processed foods in some things could actually flip the switch pretty quickly in changing the percentage of the American public that are obese,” said Robert Redfield, a virologist who led the Centers for Disease Control and Prevention during the previous Trump administration, in remarks at a December event hosted by the Heritage Foundation, a conservative think tank.
Claims that Big Food knowingly manufactured and sold addictive and harmful products resemble the claims leveled against Big Tobacco before the landmark $206 billion settlement was reached in 1998.
“These companies allegedly use the tobacco industry’s playbook to target children, especially Black and Hispanic children, with integrated marketing tie-ins with cartoons, toys, and games, along with social media advertising,” Rene Rocha, one of the lawyers at Morgan & Morgan representing Martinez, told KFF Health News.
The 148-page Martinez lawsuit against foodmakers draws from documents made public in litigation against tobacco companies that owned some of the biggest brands in the food industry.
Similar allegations were made against opioid manufacturers, distributors, and retailers before they agreed to pay tens of billions of dollars in a 2021 settlement with states.
The FDA ultimately put restrictions on the labeling and marketing of tobacco, and the opioid epidemic led to legislation that increased access to lifesaving medications to treat addiction.
But the Trump administration’s zeal in taking on Big Food may face unique challenges.
The ability of the FDA to impose regulation is hampered in part by funding. While the agency’s drug division collects industry user fees, its division of food relies on a more limited budget determined by Congress.
Change can take time because the agency moves at what some critics call a glacial pace. Last year, the FDA revoked a regulation allowing brominated vegetable oil in food products. The agency determined in 1970 that the additive was not generally recognized as safe.
Efforts to curtail the marketing of ultra-processed food could spur lawsuits alleging that any restrictions violate commercial speech protected by the First Amendment. And Kennedy — if he is confirmed as HHS secretary — may struggle to get support from a Republican-led Congress that champions less federal regulation and a president-elect who during his previous term served fast food in the White House.
“The question is, will RFK be able to make a difference?” said David L. Katz, a doctor who founded True Health Initiative, a nonprofit group that combats public health misinformation. “No prior administration has done much in this space, and RFK is linked to a particularly anti-regulatory administration.”
Meanwhile, the U.S. population is recognized as among the most obese in the world and has the highest rate of people with multiple chronic conditions among high-income countries.
“There is a big grassroots effort out there because of how sick we are,” said Jerold Mande, who served as deputy undersecretary for food safety at the Department of Agriculture from 2009 to 2011. “A big part of it is people shouldn’t be this sick this young in their lives. You’re lucky if you get to 18 without a chronic disease. It’s remarkable.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brain Power – by Michael Gelb & Kelly Howell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s most important when it comes to brain health? Is it the right diet? Supplements? Brain-training? Attitude? Sleep? Physical exercise? Social connections? Something else?
This book covers a lot of bases, including all of the above and more. The authors are not scientists by training and this is not a book of science, so much as a book of aggregated science-based advice from other sources. The authors did consult with many scientists, and their input is shown throughout.
In the category of criticism, nothing here goes very deeply into the science, and there’s also nothing you wouldn’t find we’ve previously written about in a 10almonds article somewhere. But all the same, it’s good to have a wide variety of brain-healthy advices all in one place.
Bottom line: if you’re looking for a one-stop-shop “look after your brain as you age” guide, then this is a good one.
Click here to check out Brain Power, and improve your mind as you age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
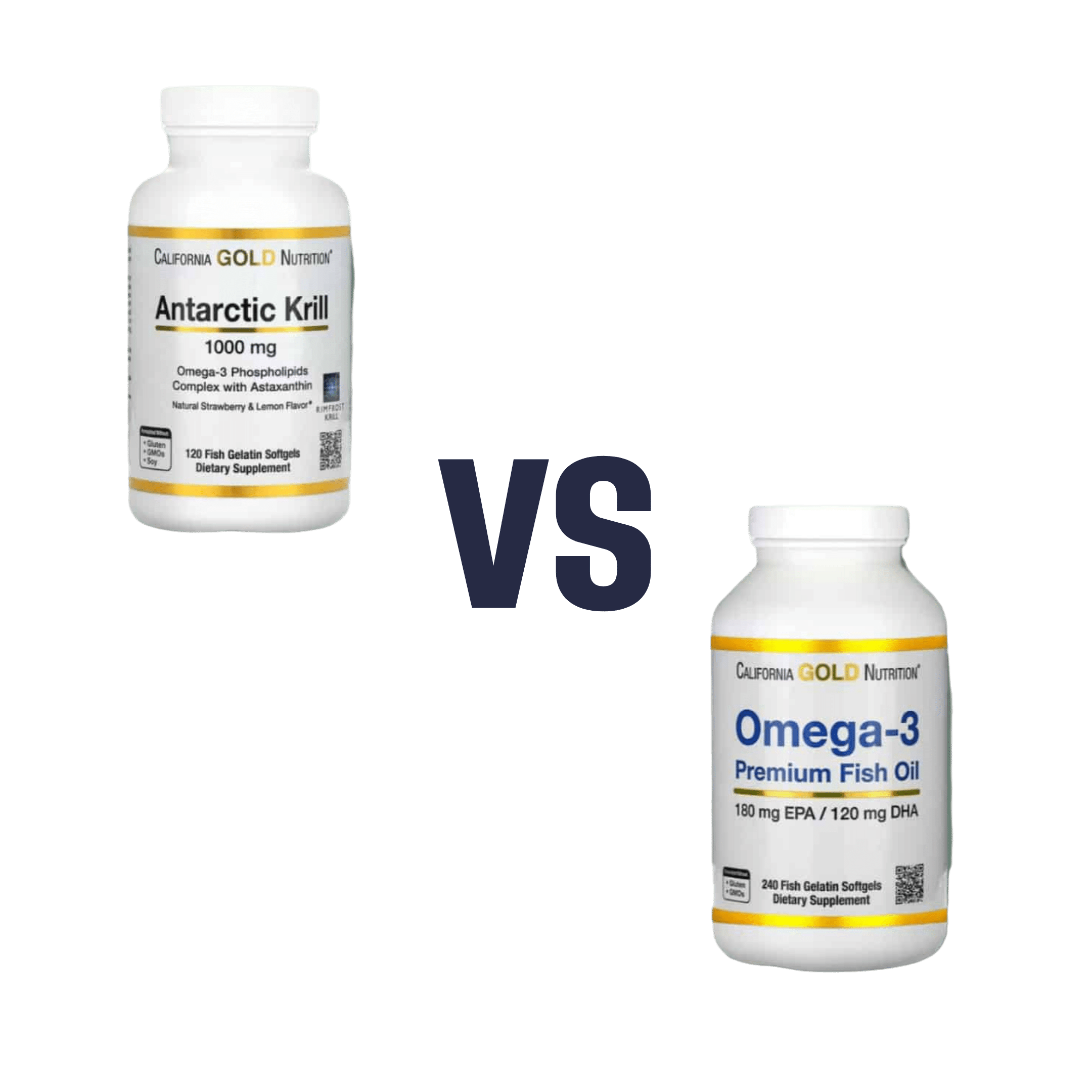
Krill Oil vs Fish Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing krill oil to fish oil, we picked the krill oil.
Why?
Both of these products are good sources of omega-3 fatty acids EPA and DHA, and for the specific brand depicted above, in both cases 2 softgels will give you the recommended daily amount (which is generally held to be 250–500mg combined omega-3s per day).
This brand’s fish oil gives more (640mg combined omega-3s per 2 softgels, to the same brand’s krill oil’s 480mg per 2 softgels), but since the krill oil is already in the high end of RDA territory, the excess beyond the RDA is not helpful, and not a huge factor. More quantity is not always better, when the body can only process so much at a time.
However, the krill oil gives some extra things that the fish oil doesn’t:
- Astaxanthin, a “super-antioxidant”
- and neuroprotectant, heart-healthy phospholipids
Additional considerations
We have declared “the winner” based on health considerations only. That’s a sticking point for us in all our writings; we’ll occasionally look at and mention other factors, but we know that health is what you’re here for, so that’s what we’ll always treat as most critical.
However, in case these factors may interest you and/or influence you to one or the other:
• The fish oil is about 30% cheaper financially
• The krill oil is a lot more sustainable environmentallyBack to the health science…
Read more:
• What Omega-3 Fatty Acids Really Do For Us
• Astaxanthin: Super-Antioxidant & NeuroprotectantWant some? Here for your convenience are some example products on Amazon:
(brands available will vary per region, but now you know what to look out for on the labels!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: