Here’s how to help protect babies and kids from RSV
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- RSV is a respiratory virus that is especially dangerous for babies and young children.
- There are two ways to help protect babies from RSV: vaccination during pregnancy and giving babies nirsevimab, an RSV antibody shot.
- If someone in your household has RSV, watch for signs of severe illness and take steps to help prevent it from spreading.
Respiratory syncytial virus, or RSV, is a very contagious seasonal respiratory illness that is especially dangerous for infants and young children. Cases rose dramatically last month, and an increasing number of kids and older adults with RSV are being hospitalized across the United States.
Fortunately, pregnant people can get vaccinated during pregnancy or get their infants and young children an RSV antibody shot to help them stay healthy.
Read on to learn about symptoms of RSV, how to help prevent infants and children from getting very sick, and what families should do if someone in their household is sick with the virus.
What are the symptoms of RSV in babies and young children?
RSV symptoms in young children may include a runny nose, decreased eating and drinking, and coughing, which may lead to wheezing and difficulty breathing.
Infants with RSV may show symptoms like irritability, decreased activity and appetite, and life-threatening pauses in breathing (apnea) that last for more than 10 seconds. Most infants with RSV will not develop a fever, but babies who are born prematurely, have weakened immune systems, or have chronic lung disease are more likely to become very sick.
Who is eligible for an RSV antibody shot?
The Centers for Disease Control and Prevention recommends that babies younger than 8 months whose gestational parent did not receive an RSV vaccine during pregnancy receive nirsevimab between October and March, when RSV typically peaks. This antibody shot delivers proteins that can help protect them against RSV.
Nirsevimab is also recommended for children between 8 and 19 months who are at increased risk of severe RSV, including children who are born prematurely, have chronic lung disease or severe cystic fibrosis, are immunocompromised, or are American Indians or Alaska Natives.
Nirsevimab is typically covered by insurance or costs $495 out of pocket. Children who are eligible for the CDC’s Vaccines for Children Program can receive nirsevimab at no cost.
How can families help prevent RSV from spreading?
It’s recommended that children and adults who are sick with RSV stay home and away from others. If your infant or child has difficulty breathing or develops blue or gray skin, take them to an emergency room right away.
People who are infected with RSV can spread the disease when they cough or sneeze; have close contact with others; or touch, cough, or sneeze on shared surfaces. Help protect your family from catching and spreading RSV at home and in public places by ensuring that everyone covers their mouths during coughing and sneezing, washes their hands often, and wears a high-quality, well-fitting mask.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Creamy Fortifying Cauliflower Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As delicious as it is super-easy to make, this one is full of protein, fiber, healthy fats, and some of the most health-giving spices around.
You will need
- 1 quart low-sodium vegetable stock
- 1 large cauliflower, cut into florets
- 1 large onion, finely chopped
- 2 cans cannellini (or other white) beans, drained and rinsed
- 1 cup raw cashews, soaked in hot water for at least 5 minutes, and drained (if allergic, substitute chickpeas)
- 1 bulb (yes, a whole bulb) garlic, roughly chopped
- 5 tbsp nutritional yeast
- 10 fresh sprigs of thyme (keep them whole!)
- 1 large fresh sprig of rosemary (keep this whole too!)
- zest of 1 lemon
- 1 tbsp red chili flakes
- 1 tbsp black pepper, coarse ground
- 1 tsp MSG or 2 tsp low-sodium salt
- ½ tsp ground turmeric
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Tightly tie up the sprigs of rosemary and thyme with kitchen twine (shining a bright light on it and asking it invasive questions is optional)
2) Heat some olive oil to a medium heat in your biggest sauté pan or similar. Add the onions, and cook for about 10 minutes, stirring as necessary. We are not trying to outright caramelize them here, but we do want them browned a little.
3) Add the garlic and cook for another 2 minutes, stirring frequently.
4) Add the vegetable stock, and stir, ensuring no onion is stuck to the base of the pan. Add the cauliflower, cashews, beans, nooch, pepper, turmeric, and MSG/salt, stirring to combine. Don’t worry if the cauliflower isn’t all submerged; it’ll be fine in a little while.
5) Add the herbs, submerging them in the soup (still tied up bouquet garni style).
6) Bring to a boil, reduce to a simmer and cook for 15–20 minutes; the cauliflower will be soft when it’s ready.
7) Remove the bouquet garni, and blend the soup until thick and creamy. You can do this with an immersion blender, but to get the smoothest soup, you’ll need to use a stand blender. Either ensure yours is safe for hot liquids, or else allow to cool, blend, and reheat later. This is important, as otherwise your blender could explode.
8) Serve, using the lemon zest and chili for the garnish:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Some Surprising Truths About Hunger And Satiety
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
Captivate – by Vanessa van Edwards
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book isn’t just for one area of human interactions. It covers everything from the boardroom to the bedroom (not necessarily a progression with the same person!), business associates, friends, partners, kids, and more.
She presents information in a layered manner, covering for example, chapter-by-chapter:
- the first five minutes
- the first five hours
- the first five days
She also covers such things as:
- starting conversations in a way that makes you memorable (without making it weird!)
- the importance of really listening (and how to do that)
- collecting like-minded people appropriately
- introducing other people! Because a) it’s not all about you, but also b) you’re the person who knows everybody now
- where to stand at parties / networking events!
- dating and early-days dating messages
- reading the room, reading the people
All in all, a great resource for anyone who wants to make (and maintain!) meaningful relationships with those around you.
Share This Post
-
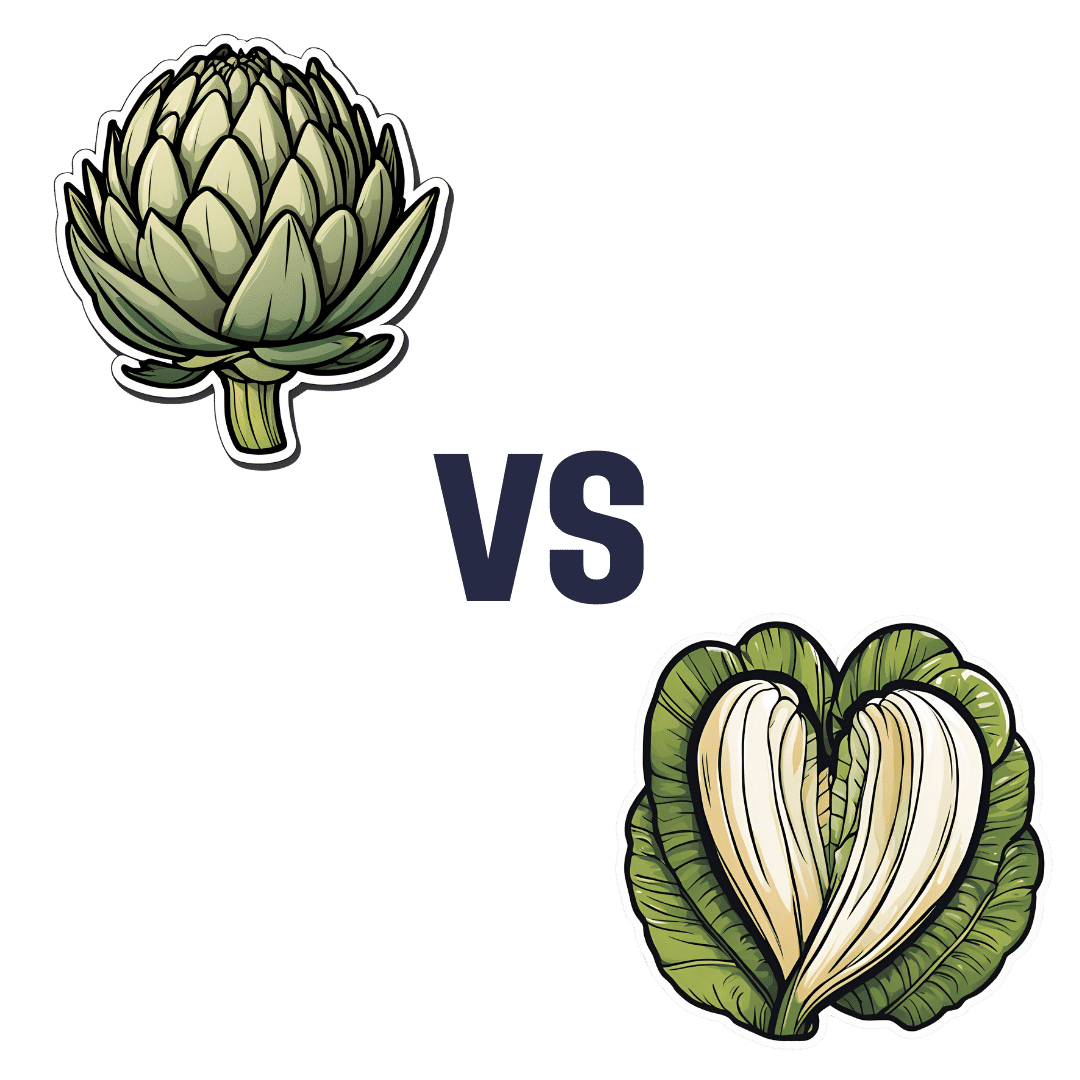
Artichoke vs Heart of Palm– Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to heart of palm, we picked the artichoke.
Why?
If you were thinking “isn’t heart of palm full of saturated fat?” then no… Palm oil is, but heart of palm itself has 0.62g/100g fat, of which, 0.13g saturated fat. So, negligible.
As for the rest of the macros, artichoke has more protein, carbs, and fiber, thus being the “more food per food” option. Technically heart of palm has the lower glycemic index, but they are both low-GI foods, so it’s really not a factor here.
Vitamins are where artichoke shines; artichoke has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline, while heart of palm is not higher in any vitamins.
The minerals situation is more balanced: artichoke has more copper, magnesium, phosphorus, and potassium, while heart of palm has more iron, manganese, selenium, and zinc.
Adding up the categories, the winner of this “vegetables with a heart” face-off is clearly artichoke.
Fun fact: in French, “to have the heart of an artichoke” (avoir le coeur d’un artichaut) means to fall in love easily. Perfect vegetable for a romantic dinner, perhaps (especially with all those generous portions of B-vitamins)!
Want to learn more?
You might like to read:
Artichoke vs Cabbage – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Ouch. That ‘Free’ Annual Checkup Might Cost You. Here’s Why.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kristy Uddin, 49, went in for her annual mammogram in Washington state last year, she assumed she would not incur a bill because the test is one of the many preventive measures guaranteed to be free to patients under the 2010 Affordable Care Act. The ACA’s provision made medical and economic sense, encouraging Americans to use screening tools that could nip medical problems in the bud and keep patients healthy.
So when a bill for $236 arrived, Uddin — an occupational therapist familiar with the health care industry’s workings — complained to her insurer and the hospital. She even requested an independent review.
“I’m like, ‘Tell me why am I getting this bill?’” Uddin recalled in an interview. The unsatisfying explanation: The mammogram itself was covered, per the ACA’s rules, but the fee for the equipment and the facility was not.
That answer was particularly galling, she said, because, a year earlier, her “free” mammogram at the same health system had generated a bill of about $1,000 for the radiologist’s reading. Though she fought that charge (and won), this time she threw in the towel and wrote the $236 check. But then she dashed off a submission to the KFF Health News-NPR “Bill of the Month” project:
“I was really mad — it’s ridiculous,” she later recalled. “This is not how the law is supposed to work.”
The ACA’s designers might have assumed that they had spelled out with sufficient clarity that millions of Americans would no longer have to pay for certain types of preventive care, including mammograms, colonoscopies, and recommended vaccines, in addition to doctor visits to screen for disease. But the law’s authors didn’t reckon with America’s ever-creative medical billing juggernaut.
Over the past several years, the medical industry has eroded the ACA’s guarantees, finding ways to bill patients in gray zones of the law. Patients going in for preventive care, expecting that it will be fully covered by insurance, are being blindsided by bills, big and small.
The problem comes down to deciding exactly what components of a medical encounter are covered by the ACA guarantee. For example, when do conversations between doctor and patient during an annual visit for preventive services veer into the treatment sphere? What screenings are needed for a patient’s annual visit?
A healthy 30-year-old visiting a primary care provider might get a few basic blood tests, while a 50-year-old who is overweight would merit additional screening for Type 2 diabetes.
Making matters more confusing, the annual checkup itself is guaranteed to be “no cost” for women and people age 65 and older, but the guarantee doesn’t apply for men in the 18-64 age range — though many preventive services that require a medical visit (such as checks of blood pressure or cholesterol and screens for substance abuse) are covered.
No wonder what’s covered under the umbrella of prevention can look very different to medical providers (trying to be thorough) and billers (intent on squeezing more dollars out of every medical encounter) than it does to insurers (who profit from narrower definitions).
For patients, the gray zone has become a billing minefield. Here are a few more examples, gleaned from the Bill of the Month project in just the past six months:
Peter Opaskar, 46, of Texas, went to his primary care doctor last year for his preventive care visit — as he’d done before, at no cost. This time, his insurer paid $130.81 for the visit, but he also received a perplexing bill for $111.81. Opaskar learned that he had incurred the additional charge because when his doctor asked if he had any health concerns, he mentioned that he was having digestive problems but had already made an appointment with his gastroenterologist. So, the office explained, his visit was billed as both a preventive physical and a consultation. “Next year,” Opasker said in an interview, if he’s asked about health concerns, “I’ll say ‘no,’ even if I have a gunshot wound.”
Kevin Lin, a technology specialist in Virginia in his 30s, went to a new primary care provider to take advantage of the preventive care benefit when he got insurance; he had no physical complaints. He said he was assured at check-in that he wouldn’t be charged. His insurer paid $174 for the checkup, but he was billed an additional $132.29 for a “new patient visit.” He said he has made many calls to fight the bill, so far with no luck.
Finally, there’s Yoori Lee, 46, of Minnesota, herself a colorectal surgeon, who was shocked when her first screening colonoscopy yielded a bill for $450 for a biopsy of a polyp — a bill she knew was illegal. Federal regulations issued in 2022 to clarify the matter are very clear that biopsies during screening colonoscopies are included in the no-cost promise. “I mean, the whole point of screening is to find things,” she said, stating, perhaps, the obvious.
Though these patient bills defy common sense, room for creative exploitation has been provided by the complex regulatory language surrounding the ACA. Consider this from Ellen Montz, deputy administrator and director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare & Medicaid Services, in an emailed response to queries and an interview request on this subject: “If a preventive service is not billed separately or is not tracked as individual encounter data separately from an office visit and the primary purpose of the office visit is not the delivery of the preventive item or service, then the plan issuer may impose cost sharing for the office visit.”
So, if the doctor decides that a patient’s mention of stomach pain does not fall under the umbrella of preventive care, then that aspect of the visit can be billed separately, and the patient must pay?
And then there’s this, also from Montz: “Whether a facility fee is permitted to be charged to a consumer would depend on whether the facility usage is an integral part of performing the mammogram or an integral part of any other preventive service that is required to be covered without cost sharing under federal law.”
But wait, how can you do a mammogram or colonoscopy without a facility?
Unfortunately, there is no federal enforcement mechanism to catch individual billing abuses. And agencies’ remedies are weak — simply directing insurers to reprocess claims or notifying patients they can resubmit them.
In the absence of stronger enforcement or remedies, CMS could likely curtail these practices and give patients the tools to fight back by offering the sort of clarity the agency provided a few years ago regarding polyp biopsies — spelling out more clearly what comes under the rubric of preventive care, what can be billed, and what cannot.
The stories KFF Health News and NPR receive are likely just the tip of an iceberg. And while each bill might be relatively small compared with the stunning $10,000 hospital bills that have become all too familiar in the United States, the sorry consequences are manifold. Patients pay bills they do not owe, depriving them of cash they could use elsewhere. If they can’t pay, those bills might end up with debt-collection agencies and, ultimately, harm their credit score.
Perhaps most disturbing: These unexpected bills might discourage people from seeking preventive screenings that could be lifesaving, which is why the ACA deemed them “essential health benefits” that should be free.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lies I Taught in Medical School – by Dr. Robert Lufkin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There seems to be a pattern of doctors who practice medicine one way, get a serious disease personally, and then completely change their practice of medicine afterwards. This is one of those cases.
Dr. Lufkin here presents, on a chapter-by-chapter basis, the titularly promised “lies” or, in more legally compliant speak (as he acknowledges in his preface), flawed hypotheses that are generally taught as truths. In many cases, the “lie” is some manner of “xyz is normal and nothing to worry about”, and/or “there is nothing to be done about xyz; suck it up”.
The end result of the information is not complicated—enjoy a plants-forward whole foods low-carb diet to avoid metabolic diseases and all the other things to branch off from same (Dr. Lufkin makes a fair case for metabolic disease leading to a lot of secondary diseases that aren’t considered metabolic diseases per se). But, the journey there is actually important, as it answers a lot of questions that are much less commonly understood, and often not even especially talked-about, despite their great import and how they may affect health decisions beyond the dietary. Things like understanding the downsides of statins, or the statistical models that can be used to skew studies, per relative risk reduction and so forth.
Bottom line: this book gives the ins and outs of what can go right or wrong with metabolic health and why, and how to make sure you don’t sabotage your health through missing information.
Click here to check out Lies I Taught In Medical School, and arm yourself with knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pasteurization: What It Does And Doesn’t Do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pasteurization’s Effect On Risks & Nutrients
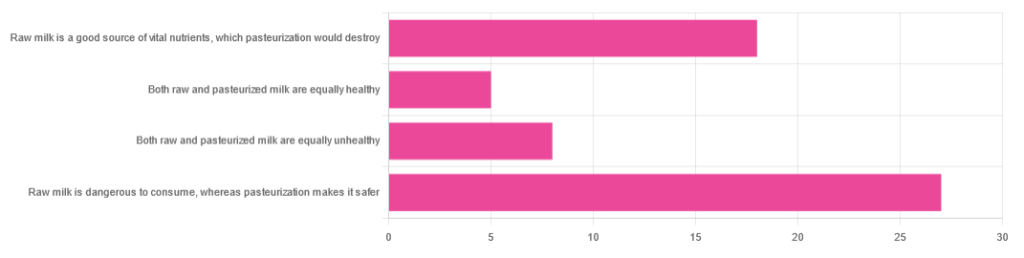
In Wednesday’s newsletter, we asked you for your health-related opinions of raw (cow’s) milk, and got the above-depicted, below-described, set of responses:
- About 47% said “raw milk is dangerous to consume, whereas pasteurization makes it safer”
- About 31% said “raw milk is a good source of vital nutrients which pasteurization would destroy”
- About 14% said “both raw milk and pasteurized milk are equally unhealthy”
- About 9% said “both raw milk and pasteurized milk are equally healthy”
Quite polarizing! So, what does the science say?
“Raw milk is dangerous to consume, whereas pasteurization makes it safer: True or False?”
True! Coincidentally, the 47% who voted for this are mirrored by the 47% of the general US population in a similar poll, deciding between the options of whether raw milk is less safe to drink (47%), just as safe to drink (15%), safer to drink (9%), or not sure (30%):
Public Fails to Appreciate Risk of Consuming Raw Milk, Survey Finds
As for what those risks are, by the way, unpasteurized dairy products are estimated to cause 840x more illness and 45x more hospitalizations than pasteurized products.
This is because unpasteurized milk can (and often does) contain E. coli, Listeria, Salmonella, Cryptosporidium, and other such unpleasantries, which pasteurization kills.
Source for both of the above claims:
(we know the title sounds vague, but all this information is easily visible in the abstract, specifically, the first two paragraphs)
Raw milk is a good source of vital nutrients which pasteurization would destroy: True or False?
False! Whether it’s a “good” source can be debated depending on other factors (e.g., if we considered milk’s inflammatory qualities against its positive nutritional content), but it’s undeniably a rich source. However, pasteurization doesn’t destroy or damage those nutrients.
Incidentally, in the same survey we linked up top, 16% of the general US public believed that pasteurization destroys nutrients, while 41% were not sure (and 43% knew that it doesn’t).
Note: for our confidence here, we are skipping over studies published by, for example, dairy farming lobbies and so forth. Those do agree, by the way, but nevertheless we like sources to be as unbiased as possible. The FDA, which is not completely unbiased, has produced a good list of references for this, about half of which we would consider biased, and half unbiased; the clue is generally in the journal names. For example, Food Chemistry and the Journal of Food Science and Journal of Nutrition are probably less biased than the International Dairy Association and the Journal of Dairy Science:
FDA | Raw Milk Misconceptions and the Danger of Raw Milk Consumption
this page covers a lot of other myths too, more than we have room to “bust” here, but it’s very interesting reading and we recommend to check it out!
Notably, we also weren’t able to find any refutation by counterexample on PubMed, with the very slight exception that some studies sometimes found that in the case of milks that were of low quality, pasteurization can reduce the vitamin E content while increasing the vitamin A content. For most milks however, no significant change was found, and in all cases we looked at, B-vitamins were comparable and vitamin D, popularly touted as a benefit of cow’s milk, is actually added later in any case. And, importantly, because this is a common argument, no change in lipid profiles appears to be findable either.
In science, when something has been well-studied and there aren’t clear refutations by counterexample, and the weight of evidence is clearly very much tipped into one camp, that usually means that camp has it right.
Milk generally is good/bad for the health: True or False?
True or False, depending on what we want to look at. It’s definitely not good for inflammation, but the whole it seems to be cancer-neutral and only increases heart disease risk very slightly:
- Keep Inflammation At Bay ← short version is milk is bad, fermented milk products are fine in moderation
- Is Dairy Scary? ← short version is that milk is neither good nor terrible; fermented dairy products however are health-positive in numerous ways when consumed in moderation
You may be wondering…
…how this goes for the safety of dairy products when it comes to the bird flu currently affecting dairy cows, so:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: