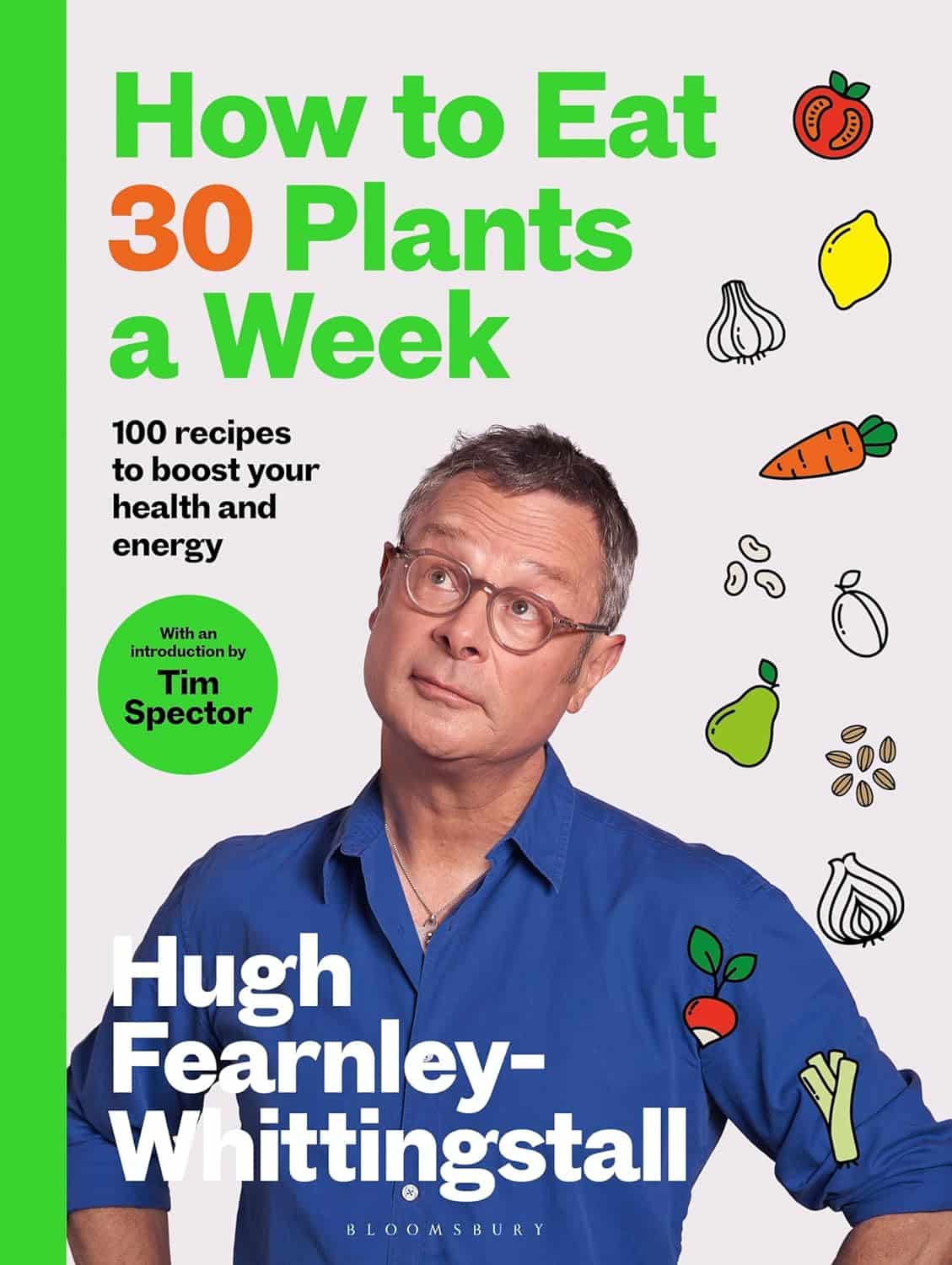
How to Eat 30 Plants a Week – by Hugh Fearnley-Whittingstall
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re used to eating the same two fruits and three vegetables in rotation, the “gold standard” evidence-based advice to “eat 30 different plants per week” can seem a little daunting.
Where this book excels is in reminding the reader to use a lot of diverse plants that are readily available in any well-stocked supermarket, but often get forgotten just because “we don’t buy that”, so it becomes invisible on the shelf.
It’s not just a recipe book (though yes, there are plenty of recipes here); it’s also advice about stocking up and maintaining that stock, advice on reframing certain choices to inject a little diversity into every meal without it become onerous, meal-planning rotation advice, and a lot of recipes that are easy but plant-rich, for example “this soup that has these six plants in it”, etc.
He also gives, for those eager to get started, “10 x 3 recipes per week to guarantee your 30”, in other words, 10 sets of 3 recipes, wherein each set of 3 recipes uses >30 different plants between them, such that if we have each of these set-of-three meals over the course of the week, then what we do in the other 4–18 meals (depending on how many meals per day you like to have) is all just a bonus.
The latter is what makes this book an incredibly stress-free approach to more plant-diverse eating for life.
Bottom line: if you want to be able to answer “do you get your five-a-day?” with “you mean breakfast?” because you’ve already hit five by breakfast each day, then this is the book for you.
Click here to check out How To Eat 30 Plants A Week, and indeed eat 30+ different plants per week!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Millet vs Rye – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing millet to rye, we picked the rye.
Why?
In terms of macros, they’re about equal on protein, and rye has more carbs and fiber, the ratio of which give it the lower glycemic index, so we say rye wins this category.
In the category of vitamins, millet has more of vitamins B1, B2, B6, and B9, while rye has more of vitamins A, B5, E, and K. Notionally, that’s a 4:4 tie, though rye’s margins of difference are an order of magnitude greater, so we say rye takes a marginal victory on this one.
When it comes to minerals, there’s nothing to debate here: millet has more copper, while rye has more calcium, manganese, phosphorus, potassium, selenium, and zinc. An easy win for rye on this one.
Adding up the sections gives the overall win to rye, but there is one other thing worth mentioning: millet is naturally gluten-free, but rye is not, so if you are avoiding gluten for any reason, you’ll want to pick the millet in this case.
See also: Gluten: What’s The Truth?
Aside from that, by all means enjoy either or both, in moderation! Diversity is good.
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Enjoy!
Share This Post
-
Fast Exercise – by Dr. Michael Mosley & Peta Bee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the benefits of High-Intensity Interval Training (HIIT), but there’s more to say than we can fit in a short article!
Dr. Michael Mosley, who hates exercise but knows his stuff when it comes to the benefits, teamed up with Peta Bee, who loves exercise and is a science journalist with degrees in sports science and nutrition, to bring us this book.
In it, we learn a lot about:
- the science of HIIT
- what makes it so different from most kinds of exercise
- exactly what benefits one can expect
…in a very detailed clinical fashion (while still remaining very readable).
By “very detailed clinical fashion”, here we mean “one minute of this kind of exercise this many times per week over this period of time will give this many extra healthy life-years”, for example, along with lots of research to back numbers, and explanations of the mechanisms of action (e.g. reducing inflammatory biomarkers of aging, increasing cellular apoptosis, improving cardiometabolic stats for reduced CVD risk, and many things)
There’s also time/space given over to exactly what to do and how to do it, giving enough options to suit personal tastes/circumstances.
Bottom line: if you’d like to make your exercise work a lot harder for you while you spend a lot less time working out, then this book will help you do just that!
Click here to check out Fast Exercise, and enjoy the benefits!
Share This Post
-
The Modern Art and Science of Mobility – by Aurélien Broussal-Derval
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed mobility books before, so what makes this one stand out?
We’ll be honest: the illustrations are lovely.
The science, the information, the exercises, the routines, the programs… All these things are excellent too, but these can be found in many a book.
What can’t usually be found is very beautiful (yet no less clear) watercolor paintings and charcoal sketches as anatomical illustrations.
There are photos too (also of high quality), but the artistry of the paintings and sketches is what makes the reader want to spend time perusing the books.
At least, that’s what this reviewer found! Because it’s all very well having access to a lot of information (and indeed, I read so much), but making it enjoyable increases the chances of rereading it much more often.
As for the rest of the content, the book’s information is divided in categories:
- Pain (what causes it, what it means, and how to manage it)
- Breathing (yes, a whole section devoted to this, and it is aligned heavily to posture also, as well as psychological state and the effect of stress on tension, inflammation, and more)
- Movement (this is mostly about kinds of movement and ranges of movement)
- Mobility (this is about aggregating movements as a fully mobile human)
So, each builds on from the previous because any pain needs addressing before anything else, breathing (and with it, posture) comes next, then we learn about movement, then we bring it all together for mobility.
Bottom line: this is a beautiful and comprehensive book that will make learning a joy
Click here to check out The Modern Art and Science of Mobility, and learn and thrive!
Share This Post
Related Posts
-
Pomegranate vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pomegranate to cherries, we picked the pomegranate.
Why?
In terms of macros, pomegranate is slightly higher in carbs, and/but 4x higher in fiber. That’s already a good start for pomegranates. Lest we be accused of cherry-picking, though, we’ll mention that pomegranate is also slightly higher in protein and fat, for what it’s worth—which is not a lot. As with most fruits, the protein and fat numbers are low importance next to the carb:fiber ratio.
When it comes to vitamins, pomegranate has more of vitamins B1, B2, B5, B6, B9. E. K, and choline. On the other hand, cherries have more of vitamins A and B3. The two fruits are equal in vitamin C. This all makes for a clear win for pomegranate.
In the category of minerals, pomegranate boasts more copper, magnesium, phosphorus, potassium, selenium, and zinc. In contrast, cherries have slightly more calcium. Another win for pomegranate.
Both of these fruits have beneficial polyphenols, each with a slightly different profile, but neither pressingly better than the other.
In short: as ever with healthy foods, enjoy both—diversity is good! But if you’re going to pick on, we recommend the pomegranate.
Want to learn more?
You might like to read:
- Pomegranate Peel’s Potent Potential ← so don’t throw it away!
- Cherries’ Very Healthy Wealth Of Benefits!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Asparagus vs Eggplant – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing asparagus to eggplant, we picked the asparagus.
Why?
In terms of macros, they’re very similar. Technically asparagus has twice the protein, but it’s at 2.2g/100g compared to eggplant’s 0.98g/100g, so it’s not too meaningful. They’re both mostly water, low in carbs, with a little fiber, and negligible fat (though eggplant technically has more fat, but again, these numbers are miniscule). For practical purposes, the two vegetables are even in this category, or if you really want decisive answers, a tiny margin of a win for asparagus.
In the category of vitamins, asparagus is much higher in vitamins A, B1, B2, B3, B5, B6, B9, E, & K, as well as choline. Eggplant is not higher in any vitamins. A clear win for asparagus.
When it comes to minerals, asparagus is much higher in calcium, copper, iron, phosphorus, selenium, and zinc, while eggplant is a little higher in manganese. Another easy win for asparagus.
Lastly, asparagus wins on polyphenols too, with its high quercetin content. Eggplant does contain some polyphenols, but in such tiny amounts that even added up they’re less than 7% of what asparagus has to offer in quercetin alone.
Obviously, enjoy both, though! Diversity is healthy.
Want to learn more?
You might like to read:
Fight Inflammation & Protect Your Brain, With Quercetin
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Toe-Tapping Tip For Better Balance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Balance is critical for health especially in older age, since it’s amazing how much else can go dramatically and suddenly wrong after a fall. So, here’s an exercise to give great balance and stability:
How to do it
You will need:
- Something to hold onto, such as a countertop
- A target on the floor, such as a mark or a coin
The steps:
- Lift one leg up, bring your foot forward, and tap the object in front of you.
- Then, bring that foot back to where it started.
- Next, switch to the other leg and tap.
- Alternate between your right and left legs, shifting back and forth.
- Your goal is to do this for 10 repetitions on each leg without holding on.
How it works:
Whenever you tap, you have to lift one leg up and reach it out in front of you. Doing this requires you to stand on one leg while moving a weight (namely: your other leg), which is something many people, especially upon getting older, are hesitant to do. If you’re unable to stand on one leg, let alone move your center of gravity (per the counterbalance of the other leg) while doing so, you may end up shuffling and walking with your feet sliding across the ground—something you really want to avoid.
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fall Special ← this is about not falling, or, failing that, minimizing injury if you do
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: