Gentle Nutrition – by Rachel Hartley, RD, LD
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle here claims “a non-diet approach”, but doesn’t everything, nowadays? Even books titled “The such-and-such Diet” tend to also assure us “it’s not actually a diet; it’s just a way of eating”, as if a diet is not—by definition—a way of eating. Usually what they want to communicate is that it’s not a restrictive diet, usually meaning not restrictive in quantity, or not restrictive in food type (rarely both).
This book is about intuitive eating, which is about as non-restrictive as any dietary approach can be, since it doesn’t restrict food type at at all, and it doesn’t restrict quantity in advance—rather, we learn to pay closer attention to our full signals.
No wait, we don’t. This time, it’s not about “full”, it’s about “satisfied”. This comes in two forms:
- A principle somewhat akin to the “eat until 80% full” idea
- A principle of ensuring the good is culinarily satisfying
This latter is important, if we want to have a good relationship with eating, and it also helps reduce portion sizes, when we truly take the time to mindfully savor a tasty morsel, rather than wolf down a plate of mediocre food.
The style is one that balance being encouraging with delivering science to back up that encouragement. This not only means encouragement to take up this dietary approach, but also, encouragement to let go of things like calorie-counting and BMI.
The recipes arranged per meal type, and indeed include things not found in many healthy eating books, such as gyoza dumplings, gnocchi, wontons, and shortbread. The recipes are mostly not, by default, vegan, vegetarian, gluten-free, dairy-free, or such. So if you have your own food restriction(s), the number of usable recipes will be diminished, barring any substitutions you can make yourself.
Bottom line: this is more about about how to go about intuitive eating, than it is a book with a lot of nutritional information (though there is some of that too). If you’d like to get going with intuitive eating, then this book can help.
Click here to check out Gentle Nutrition, and nourish gently!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could ADHD drugs reduce the risk of early death? Unpacking the findings from a new Swedish study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Attention-deficit hyperactivity disorder (ADHD) can have a considerable impact on the day-to-day functioning and overall wellbeing of people affected. It causes a variety of symptoms including difficulty focusing, impulsivity and hyperactivity.
For many, a diagnosis of ADHD, whether in childhood or adulthood, is life changing. It means finally having an explanation for these challenges, and opens up the opportunity for treatment, including medication.
Although ADHD medications can cause side effects, they generally improve symptoms for people with the disorder, and thereby can significantly boost quality of life.
Now a new study has found being treated for ADHD with medication reduces the risk of early death for people with the disorder. But what can we make of these findings?
A large study from Sweden
The study, published this week in JAMA (the prestigious journal of the American Medical Association), was a large cohort study of 148,578 people diagnosed with ADHD in Sweden. It included both adults and children.
In a cohort study, a group of people who share a common characteristic (in this case a diagnosis of ADHD) are followed over time to see how many develop a particular health outcome of interest (in this case the outcome was death).
For this study the researchers calculated the mortality rate over a two-year follow up period for those whose ADHD was treated with medication (a group of around 84,000 people) alongside those whose ADHD was not treated with medication (around 64,000 people). The team then determined if there were any differences between the two groups.
What did the results show?
The study found people who were diagnosed and treated for ADHD had a 19% reduced risk of death from any cause over the two years they were tracked, compared with those who were diagnosed but not treated.
In understanding this result, it’s important – and interesting – to look at the causes of death. The authors separately analysed deaths due to natural causes (physical medical conditions) and deaths due to unnatural causes (for example, unintentional injuries, suicide, or accidental poisonings).
The key result is that while no significant difference was seen between the two groups when examining natural causes of death, the authors found a significant difference for deaths due to unnatural causes.
So what’s going on?
Previous studies have suggested ADHD is associated with an increased risk of premature death from unnatural causes, such as injury and poisoning.
On a related note, earlier studies have also suggested taking ADHD medicines may reduce premature deaths. So while this is not the first study to suggest this association, the authors note previous studies addressing this link have generated mixed results and have had significant limitations.
In this new study, the authors suggest the reduction in deaths from unnatural causes could be because taking medication alleviates some of the ADHD symptoms responsible for poor outcomes – for example, improving impulse control and decision-making. They note this could reduce fatal accidents.
The authors cite a number of studies that support this hypothesis, including research showing ADHD medications may prevent the onset of mood, anxiety and substance use disorders, and lower the risk of accidents and criminality. All this could reasonably be expected to lower the rate of unnatural deaths.
Strengths and limitations
Scandinavian countries have well-maintained national registries that collect information on various aspects of citizens’ lives, including their health. This allows researchers to conduct excellent population-based studies.
Along with its robust study design and high-quality data, another strength of this study is its size. The large number of participants – almost 150,000 – gives us confidence the findings were not due to chance.
The fact this study examined both children and adults is another strength. Previous research relating to ADHD has often focused primarily on children.
One of the important limitations of this study acknowledged by the authors is that it was observational. Observational studies are where the researchers observe and analyse naturally occurring phenomena without intervening in the lives of the study participants (unlike randomised controlled trials).
The limitation in all observational research is the issue of confounding. This means we cannot be completely sure the differences between the two groups observed were not either partially or entirely due to some other factor apart from taking medication.
Specifically, it’s possible lifestyle factors or other ADHD treatments such as psychological counselling or social support may have influenced the mortality rates in the groups studied.
Another possible limitation is the relatively short follow-up period. What the results would show if participants were followed up for longer is an interesting question, and could be addressed in future research.
What are the implications?
Despite some limitations, this study adds to the evidence that diagnosis and treatment for ADHD can make a profound difference to people’s lives. As well as alleviating symptoms of the disorder, this study supports the idea ADHD medication reduces the risk of premature death.
Ultimately, this highlights the importance of diagnosing ADHD early so the appropriate treatment can be given. It also contributes to the body of evidence indicating the need to improve access to mental health care and support more broadly.
Hassan Vally, Associate Professor, Epidemiology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Somatic Exercises For Nervous System Regulation – by Rose Kilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the vagus nerve, its importance, and how to make use of it, but it’s easy to let it slip from one’s mind when it comes to exercises. This book fixes that!
The promised 35 exercises are quite a range, and are organized into sections:
- Revitalizing through breath
- Stress and tension release
- Spinal and postural health
- Mindfulness and grounding
- Movements for flexibility
- Graceful balance and focus
While it’s not necessary to do all 35 exercises, it’s recommended to do at least some from each section, to “cover one’s bases”, and enjoy the best of all worlds.
The exercises are drawn from many sources, but tai chi and yoga are certainly the most well-represented. Others, meanwhile, are straight from physiotherapy or are things one might expect to be advised at a neurology consultation.
Bottom line: if you’d like to take better care of your vagus nerve, the better for it to take care of you, this book can certainly help with that.
Click here to check out Somatic Exercises For Nervous System Regulation, and take care of yourself!
Share This Post
-
4 Ways Vaccine Skeptics Mislead You on Measles and More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Measles is on the rise in the United States. In the first quarter of this year, the number of cases was about 17 times what it was, on average, during the same period in each of the four years before, according to the Centers for Disease Control and Prevention. Half of the people infected — mainly children — have been hospitalized.
It’s going to get worse, largely because a growing number of parents are deciding not to get their children vaccinated against measles as well as diseases like polio and pertussis. Unvaccinated people, or those whose immunization status is unknown, account for 80% of the measles cases this year. Many parents have been influenced by a flood of misinformation spouted by politicians, podcast hosts, and influential figures on television and social media. These personalities repeat decades-old notions that erode confidence in the established science backing routine childhood vaccines. KFF Health News examined the rhetoric and explains why it’s misguided:
The No-Big-Deal Trope
A common distortion is that vaccines aren’t necessary because the diseases they prevent are not very dangerous, or too rare to be of concern. Cynics accuse public health officials and the media of fear-mongering about measles even as 19 states report cases.
For example, an article posted on the website of the National Vaccine Information Center — a regular source of vaccine misinformation — argued that a resurgence in concern about the disease “is ‘sky is falling’ hype.” It went on to call measles, mumps, chicken pox, and influenza “politically incorrect to get.”
Measles kills roughly 2 of every 1,000 children infected, according to the CDC. If that seems like a bearable risk, it’s worth pointing out that a far larger portion of children with measles will require hospitalization for pneumonia and other serious complications. For every 10 measles cases, one child with the disease develops an ear infection that can lead to permanent hearing loss. Another strange effect is that the measles virus can destroy a person’s existing immunity, meaning they’ll have a harder time recovering from influenza and other common ailments.
Measles vaccines have averted the deaths of about 94 million people, mainly children, over the past 50 years, according to an April analysis led by the World Health Organization. Together with immunizations against polio and other diseases, vaccines have saved an estimated 154 million lives globally.
Some skeptics argue that vaccine-preventable diseases are no longer a threat because they’ve become relatively rare in the U.S. (True — due to vaccination.) This reasoning led Florida’s surgeon general, Joseph Ladapo, to tell parents that they could send their unvaccinated children to school amid a measles outbreak in February. “You look at the headlines and you’d think the sky was falling,” Ladapo said on a News Nation newscast. “There’s a lot of immunity.”
As this lax attitude persuades parents to decline vaccination, the protective group immunity will drop, and outbreaks will grow larger and faster. A rapid measles outbreak hit an undervaccinated population in Samoa in 2019, killing 83 people within four months. A chronic lack of measles vaccination in the Democratic Republic of the Congo led to more than 5,600 people dying from the disease in massive outbreaks last year.
The ‘You Never Know’ Trope
Since the earliest days of vaccines, a contingent of the public has considered them bad because they’re unnatural, as compared with nature’s bounty of infections and plagues. “Bad” has been redefined over the decades. In the 1800s, vaccine skeptics claimed that smallpox vaccines caused people to sprout horns and behave like beasts. More recently, they blame vaccines for ailments ranging from attention-deficit/hyperactivity disorder to autism to immune system disruption. Studies don’t back the assertions. However, skeptics argue that their claims remain valid because vaccines haven’t been adequately tested.
In fact, vaccines are among the most studied medical interventions. Over the past century, massive studies and clinical trials have tested vaccines during their development and after their widespread use. More than 12,000 people took part in clinical trials of the most recent vaccine approved to prevent measles, mumps, and rubella. Such large numbers allow researchers to detect rare risks, which are a major concern because vaccines are given to millions of healthy people.
To assess long-term risks, researchers sift through reams of data for signals of harm. For example, a Danish group analyzed a database of more than 657,000 children and found that those who had been vaccinated against measles as babies were no more likely to later be diagnosed with autism than those who were not vaccinated. In another study, researchers analyzed records from 805,000 children born from 1990 through 2001 and found no evidence to back a concern that multiple vaccinations might impair children’s immune systems.
Nonetheless, people who push vaccine misinformation, like candidate Robert F. Kennedy Jr., dismiss massive, scientifically vetted studies. For example, Kennedy argues that clinical trials of new vaccines are unreliable because vaccinated kids aren’t compared with a placebo group that gets saline solution or another substance with no effect. Instead, many modern trials compare updated vaccines with older ones. That’s because it’s unethical to endanger children by giving them a sham vaccine when the protective effect of immunization is known. In a 1950s clinical trial of polio vaccines, 16 children in the placebo group died of polio and 34 were paralyzed, said Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia and author of a book on the first polio vaccine.
The Too-Much-Too-Soon Trope
Several bestselling vaccine books on Amazon promote the risky idea that parents should skip or delay their children’s vaccines. “All vaccines on the CDC’s schedule may not be right for all children at all times,” writes Paul Thomas in his bestselling book “The Vaccine-Friendly Plan.” He backs up this conviction by saying that children who have followed “my protocol are among the healthiest in the world.”
Since the book was published, Thomas’ medical license was temporarily suspended in Oregon and Washington. The Oregon Medical Board documented how Thomas persuaded parents to skip vaccines recommended by the CDC, and reported that he “reduced to tears” a mother who disagreed. Several children in his care came down with pertussis and rotavirus, diseases easily prevented by vaccines, wrote the board. Thomas recommended fish oil supplements and homeopathy to an unvaccinated child with a deep scalp laceration, rather than an emergency tetanus vaccine. The boy developed severe tetanus, landing in the hospital for nearly two months, where he required intubation, a tracheotomy, and a feeding tube to survive.
The vaccination schedule recommended by the CDC has been tailored to protect children at their most vulnerable points in life and minimize side effects. The combination measles, mumps, and rubella vaccine isn’t given for the first year of a baby’s life because antibodies temporarily passed on from their mother can interfere with the immune response. And because some babies don’t generate a strong response to that first dose, the CDC recommends a second one around the time a child enters kindergarten because measles and other viruses spread rapidly in group settings.
Delaying MMR doses much longer may be unwise because data suggests that children vaccinated at 10 or older have a higher chance of adverse reactions, such as a seizure or fatigue.
Around a dozen other vaccines have discrete timelines, with overlapping windows for the best response. Studies have shown that MMR vaccines may be given safely and effectively in combination with other vaccines.
’They Don’t Want You to Know’ Trope
Kennedy compares the Florida surgeon general to Galileo in the introduction to Ladapo’s new book on transcending fear in public health. Just as the Roman Catholic inquisition punished the renowned astronomer for promoting theories about the universe, Kennedy suggests that scientific institutions oppress dissenting voices on vaccines for nefarious reasons.
“The persecution of scientists and doctors who dare to challenge contemporary orthodoxies is not a new phenomenon,” Kennedy writes. His running mate, lawyer Nicole Shanahan, has campaigned on the idea that conversations about vaccine harms are censored and the CDC and other federal agencies hide data due to corporate influence.
Claims like “they don’t want you to know” aren’t new among the anti-vaccine set, even though the movement has long had an outsize voice. The most listened-to podcast in the U.S., “The Joe Rogan Experience,” regularly features guests who cast doubt on scientific consensus. Last year on the show, Kennedy repeated the debunked claim that vaccines cause autism.
Far from ignoring that concern, epidemiologists have taken it seriously. They have conducted more than a dozen studies searching for a link between vaccines and autism, and repeatedly found none. “We have conclusively disproven the theory that vaccines are connected to autism,” said Gideon Meyerowitz-Katz, an epidemiologist at the University of Wollongong in Australia. “So, the public health establishment tends to shut those conversations down quickly.”
Federal agencies are transparent about seizures, arm pain, and other reactions that vaccines can cause. And the government has a program to compensate individuals whose injuries are scientifically determined to result from them. Around 1 to 3.5 out of every million doses of the measles, mumps, and rubella vaccine can cause a life-threatening allergic reaction; a person’s lifetime risk of death by lightning is estimated to be as much as four times as high.
“The most convincing thing I can say is that my daughter has all her vaccines and that every pediatrician and public health person I know has vaccinated their kids,” Meyerowitz-Katz said. “No one would do that if they thought there were serious risks.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
Seven Things To Do For Good Lung Health!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
YouTube Channel Wellness Check is challenging us all to do the following things. They’re framing it as a 30-day challenge, but honestly, there’s nothing here that isn’t worth doing for life
Here’s the list:
- Stop smoking (of course, smoking is bad for everything, but the lungs are one of its main areas of destruction)
- Good posture (a scrunched up chest is not the lungs’ best operating conditions!)
- Regular exercise (exercising your body in different ways exercises your lungs in different ways!)
- Monitor air quality (some environments are much better/worse than others, but don’t underestimate household air quality threats either)
- Avoid respiratory infections (shockingly, COVID is not great for your lungs, nor are the various other respiratory infections available)
- Check your O2 saturation levels (pulse oximeters like this one are very cheap to buy and easy to use)
- Prevent mucus and phlegm from accumulating (these things are there for reasons; the top reason is trapping pathogens, allergens, and general pollutants/dust etc; once those things are trapped, we don’t want that mucus there any more!)
Check out the video itself for more detail on each of these items:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might like our article about COPD:
Why Chronic Obstructive Pulmonary Disease (COPD) Is More Likely Than You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cupping: How It Works (And How It Doesn’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good Health By The Cup?
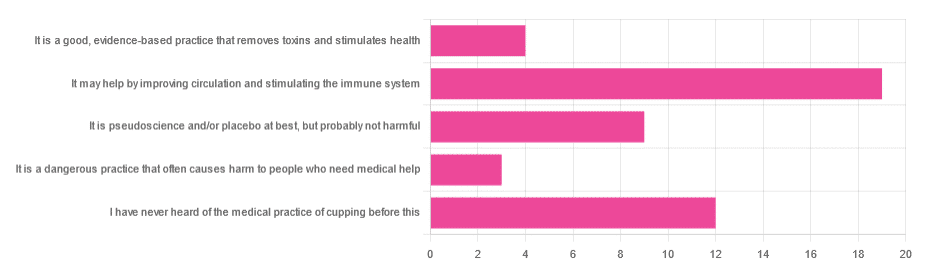
In Tuesday’s newsletter, we asked you for your opinion of cupping (the medical practice), and got the above-depicted, below-described, set of responses:
- About 40% said “It may help by improving circulation and stimulating the immune system”
- About 26% said “I have never heard of the medical practice of cupping before this”
- About 19% said “It is pseudoscience and/or placebo at best, but probably not harmful
- About 9% said “It is a good, evidence-based practice that removes toxins and stimulates health”
- About 6% said “It is a dangerous practice that often causes harm to people who need medical help”
So what does the science say?
First, a quick note for those unfamiliar with cupping: it is the practice of placing a warmed cup on the skin (open side of the cup against the skin). As the warm air inside cools, it reduces the interior air pressure, which means the cup is now (quite literally) a suction cup. This pulls the skin up into the cup a little. The end result is visually, and physiologically, the same process as what happens if someone places the nozzle of a vacuum cleaner against their skin. For that matter, there are alternative versions that simply use a pump-based suction system, instead of heated cups—but the heated cups are most traditional and seem to be most popular. See also:
National Center for Complementary and Integrative Health | Cupping
It is a dangerous practice that often causes harm to people who need medical help: True or False?
False, for any practical purposes.
- Directly, it can (and usually does) cause minor superficial harm, much like many medical treatments, wherein the benefits are considered to outweigh the harm, justifying the treatment. In the case of cupping, the minor harm is usually a little bruising, but there are other risks; see the link we gave just above.
- Indirectly, it could cause harm by emboldening a person to neglect a more impactful treatment for their ailment.
But, there’s nothing for cupping akin to the “the most common cause of death is when someone gets a vertebral artery fatally severed” of chiropractic, for example.
It is a good, evidence-based practice that removes toxins and stimulates health: True or False?
True and False in different parts. This one’s on us; we included four claims in one short line. But let’s look at them individually:
- Is it good? Well, those who like it, like it. It legitimately has some mild health benefits, and its potential for harm is quite small. We’d call this a modest good, but good nonetheless.
- Is it evidence-based? Somewhat, albeit weakly; there are some papers supporting its modest health claims, although the research is mostly only published in journals of alternative medicine, and any we found were in journals that have been described by scientists as pseudoscientific.
- Does it remove toxins? Not directly, at least. There is also a version that involves making a small hole in the skin before applying the cup, the better to draw out the toxins (called “wet cupping”). This might seem a little medieval, but this is because it is from early medieval times (wet cupping’s first recorded use being in the early 7th century). However, the body’s response to being poked, pierced, sucked, etc is to produce antibodies, and they will do their best to remove toxins. So, indirectly, there’s an argument.
- Does it stimulate health? Yes! We’ll come to that shortly. But first…
It is pseudoscience and/or placebo at best, but probably not harmful: True or False?
True in that its traditionally-proposed mechanism of action is a pseudoscience and placebo almost certainly plays a strong part, and also in that it’s generally not harmful.
On it being a pseudoscience: we’ve talked about this before, but it bears repeating; just because something’s proposed mechanism of action is pseudoscience, doesn’t necessarily mean it doesn’t work by some other mechanism of action. If you tell a small child that “eating the rainbow” will improve their health, and they believe this is some sort of magical rainbow power imbuing them with health, then the mechanism of action that they believe in is a pseudoscience, but eating a variety of colorful fruit and vegetables will still be healthy.
In the case of cupping, its proposed mechanism of action has to do withbalancing qi, yin and yang, etc (for which scientific evidence does not exist), in combination with acupuncture lore (for which some limited weak scientific evidence exists). On balancing qi, yin and yang etc, this is a lot like Europe’s historically popular humorism, which was based on the idea of balancing the four humors (blood, yellow bile, black bile, phlegm). Needless to say, humorism was not only a pseudoscience, but also eventually actively disproved with the advent of germ theory and modern medicine. Cupping therapy is not more scientifically based than humorism.
On the placebo side of things, there probably is a little more to it than that; much like with acupuncture, a lot of it may be a combination of placebo and using counter-irritation, a nerve-tricking method to use pain to reduce pain (much like pressing with one’s nail next to an insect bite).
Here’s one of the few studies we found that’s in what looks, at a glance, to be a reputable journal:
Cupping therapy and chronic back pain: systematic review and meta-analysis
It may help by improving circulation and stimulating the immune system: True or False?
True! It will improve local circulation by forcing blood into the area, and stimulate the immune system by giving it a perceived threat to fight.
Again, this can be achieved by many other means; acupuncture (or just “dry needling”, which is similar but without the traditional lore), a cold shower, and/or exercise (and for that matter, sex—which combines exercise, physiological arousal, and usually also foreign bodies to respond to) are all options that can improve circulation and stimulate the immune system.
You can read more about using some of these sorts of tricks for improving health in very well-evidenced, robustly scientific ways here:
The Stress Prescription (Against Aging!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Live Long, Die Short – by Dr. Roger Landry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First know: “die short” is not about your height—although on average, short people do live longer, partly because insulin-like growth factor (IGF-1) promotes both tallness and accelerated DNA damage (thus, aging and cancer), and partly because if someone is very tall, it can cause circulatory problems, and without a nice easy flow of blood through the brain, bad things happen (such as accumulation of harmful detritus in the brain, and increased stroke risk too).
Next know: “die short” is, in this book, actually about shortening the decline at the end of life. Sometimes people say “I don’t want to live 10 years longer; they’ll be the 10 most miserable years”, but in fact if we look after our health, we will be healthy for perhaps >9.5 of our last 10 years, while an unhealthy person may just get their expected “10 most miserable years” 10 or 20 years earlier (and then die).
So, in short (so to speak), it’s about increasing healthspan.
To enjoy the longest and healthiest healthspan, Dr. Landry offers 10 tips. We’ll not keep them a secret; they are:
- Use it or lose it
- Keep moving
- Challenge your brain
- Stay connected
- Lower your risks
- Never act your age
- Wherever you are, be fully there
- Find your purpose
- Have children in your life
- Laugh to a better life
Each of these has a chapter devoted to them, in section 2 of the book (section 1 is about what we know about healthy aging, and section 3 is about where we go from here).
You’ll notice that one item not generally found on such lists is “have children in your life”; to be clear, they don’t have to be your children, and/but they do have to be actual current children; any now-grown-up progeny aren’t what’s being talked about here (wonderful as they may be, any support role they may play gets filed under “stay connected” instead).
The style is mostly impersonal pop-science with occasional personal anecdotes, and the book’s formatting (many subheadings within chapters) makes it easy to read a bit at a time, if that’s your preference. There’s a modest, but extant, bibliography.
Bottom line: if you’d like to stay younger as you get older, this book goes into a lot of detail about 10 ways to do just that.
Click here to check out Live Long, Die Short, and live long, die short!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: