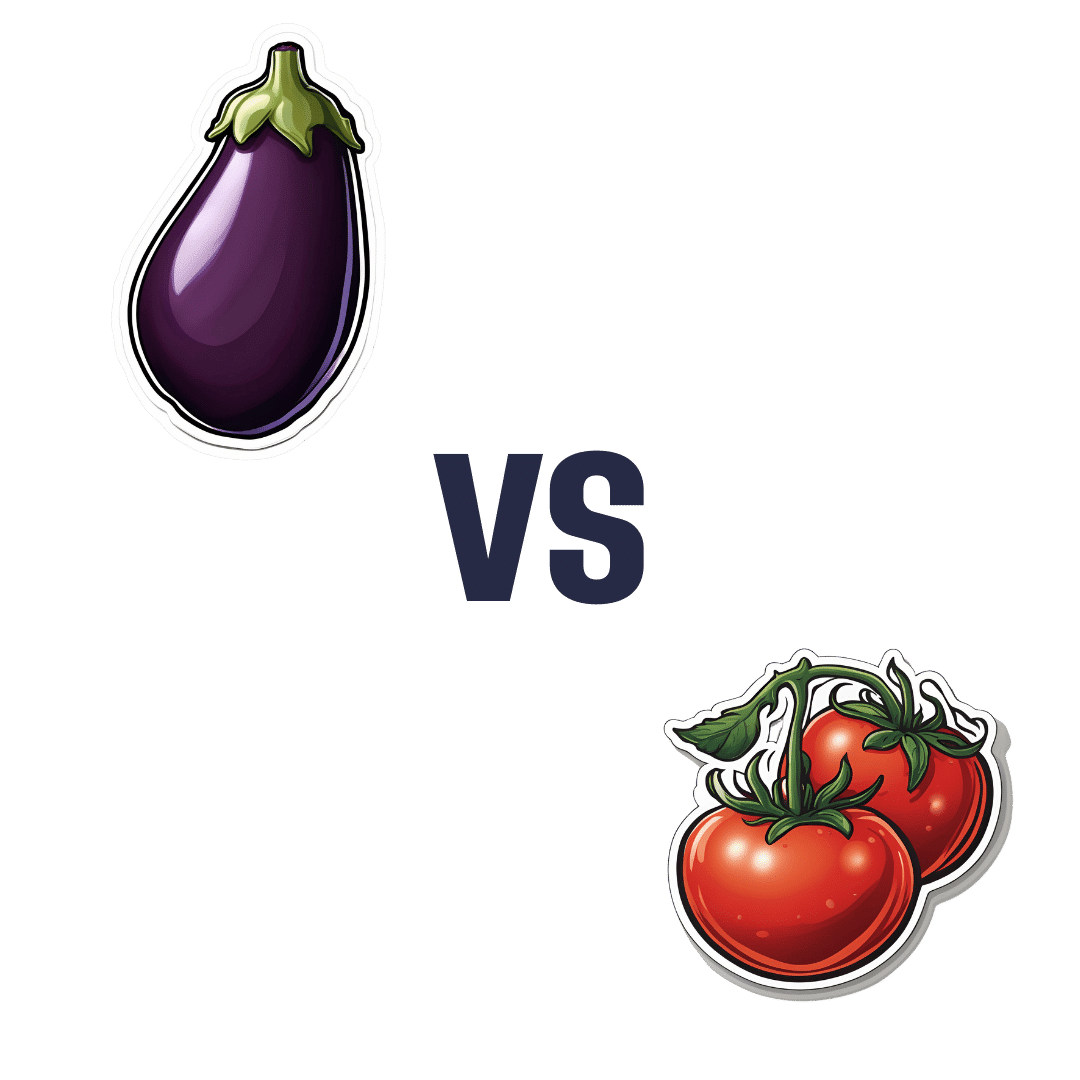
Eggplant vs Tomato – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing eggplant to tomato, we picked the eggplant.
Why?
Both have their merits! But…
In terms of macros, eggplant has nearly 3x the fiber, as well as slightly more carbs and protein, making it the most nutritionally dense option in the macros category.
In the category of vitamins, eggplant has more of vitamins B1, B2, B3, B5, B6, B9, and choline, while tomatoes have more of vitamins A, C, E, and K. So, very different vitamin coverage from each one, and/but by the numbers, eggplant wins.
When it comes to minerals, eggplant has more copper, magnesium, manganese, and selenium, while tomatoes have more calcium and iron. The margins of difference are very small in all cases, and they’re equal in phosphorus, potassium, and zinc. So this one’s very close, but by the numbers, eggplant scrapes a marginal victory.
Looking at phytochemicals, they’re about equal on polyphenols, though it’s worth mentioning that tomatoes are a famously good source of lycopene, which isn’t a polyphenol, but it is a very beneficial carotenoid, so we’ll say tomatoes get the win this round.
Adding up the sections, though, makes for an overall win for eggplant, but tomatoes are great too, and mostly in different ways than eggplant, which makes them extra good to enjoy together (salad, ratatouille, etc) for their very complementary health benefits!
Want to learn more?
You might like:
Lycopene’s Benefits For The Gut, Heart, Brain, & More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Heart Attack: His & Hers (Be Prepared!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Heart attack symptoms vary by sex. This is governed by hormones, so if you are for example a postmenopausal woman and not on HRT, your symptoms might be nearer that of men.
The following symptom list is intended as a rough “most likely” guide. You may not get all of the symptoms you “should”. You could get symptoms from the “wrong” category. So don’t sweat the minutiae, but do be aware of…
Symptoms for everyone:
- Jaw, neck, and/or back pain
- Nausea and/or vomiting
- Shortness of breath
- Feeling of impending doom ← heart attack survivors assure us that you’ll know this one if you experience it
Additional symptoms (mostly) just for men:
- Pressure and/or pain in the upper chest
- Discomfort and/or tingling in the arms
- Sudden cold sweat
Additional symptoms (mostly) just for women:
- Pressure and/or pain in the lower chest and/or abdomen
- Feeling of fullness and/or indigestion
- Fatigue, dizziness, possibly fainting
In the event of experiencing symptoms…
Call 911 or your local equivalent.This is not the time to wait to see if it goes away by itself. If unsure, call. Better safe than sorry/dead.
If you are not alone, or if it is someone with you who is having the suspected heart attack, it may be quicker to go to the Emergency Room by car, than wait for an ambulance.
Even if you choose to do that, you should still call 911 anyway, as the responder will be able to instruct you in real-time, not something we can do in a newsletter.
Note that if available, this means three people in the car is ideal:
Driver, patient, and third person on the phone giving information and following instructions.
Emergency situations rarely go entirely by-the-book, but with a little foreknowledge and at least one person with a calm head, preventable deaths can be avoided.
Share This Post
-
Young Mind Young Body – by Sue Ziang
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a very “healthy mind in a healthy body” book, consistent with the author’s status as a holistic health coach. Sometimes that produces a bit of a catch-22 regarding where to start, but for Ziang, the clear answer is to start with the mind, and specifically, one’s perception of one’s own age.
She advocates for building a young mind in a young body, and yes, that’s mind-building much like body-building. This does not mean any kind of wilful self-delusion, but rather, choosing the things that we do get to choose along the way.
The bridge between mind and body, for Ziang, is meditation—which is reasonable, as it’s very much mind-stuff and also very much neurological and has a very real-world impact on the body’s broader health, even simply by such mechanisms as changing breathing, heart rate, neurotransmitter levels, endocrine functions, and the like.
When it comes to the more physical aspects of health, her dietary advice is completely in line with what we write here at 10almonds. Hydrate well, eat more plants, especially beans and greens and whole grains, get good fats in, enjoy spices, practice mindful eating, skip the refined carbohydrates, be mindful of bio-individuality (e.g. one’s own personal dietary quirks that stem from physiology; some of us react differently to this kind of food or that for genetic reasons, and that’s not something to be overlooked).
In the category of exercise, she’s simply about moving more, which while not comprehensive, is not bad advice either.
Bottom line: if you’re looking for an “in” to holistic health and wondering where to start, this book is a fine and very readable option.
Click here to check out “Young Mind Young Body”, and transform yours!
Share This Post
-
Watermelon vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing watermelon to grapes, we picked the watermelon.
Why?
It was close! And certainly both are very healthy.
Both fruits are (like most fruits) good sources of water, fiber, vitamins, and minerals. Any sugar content (of which grapes are slightly higher) is offset by their fiber content and polyphenols.
See: Which Sugars Are Healthier, And Which Are Just The Same?
While both are good sources of vitamins A and C, watermelon has about 10x as much vitamin A, and about 6x as much vitamin C (give or take individual plants, how they were grown, etc, but the overall balance is clearly in watermelon’s favor).
When it comes to antioxidants, both fruits are good, but again watermelon is the more potent source. Grapes famously contain resveratrol, and they also contain quercetin, albeit you’d have to eat quite a lot of grapes to get a large portion.
Now, having to eat a lot of grapes might not sound like a terrible fate (who else finds that the grapes are gone by the time the groceries are put away?), but we are comparing the fruits here, and on a list of “100 best foods for quercetin”, for example, grapes took 99th place.
Watermelon’s main antioxidant meanwhile is lycopene, and watermelon is one of the best sources of lycopene in existence (better even than tomatoes).
We’ll have to do a main feature about lycopene sometime soon, so watch this space
Take care!
Share This Post
Related Posts
-
5 Steps To Quit Sugar Easily
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sugar is one of the least healthy things that most people consume, yet because it’s so prevalent, it can also be tricky to avoid at first, and the cravings can also be a challenge. So, how to quit it?
Step by step
Dr. Mike Hansen recommends the following steps:
- Be aware: a lot of sugar consumption is without realizing it or thinking about it, because of how common it is for there to be added sugar in things we might purchase ready-made, even supposedly healthy things like yogurts, or easy-to-disregard things like condiments.
- Recognize sugar addiction: a controversial topic, but Dr. Hansen comes down squarely on the side of “yes, it’s an addiction”. He wants us to understand more about the mechanics of how this happens, and what it does to us.
- Reduce gradually: instead of going “cold turkey”, he recommends we avoid withdrawal symptoms by first cutting back on liquid sugars like sodas, juices, and syrups, before eliminating solid sugar-heavy things like candy, sugar cookies, etc, and finally the more insidious “why did they put sugar in this?” added-sugar products.
- Find healthy alternatives: simple like-for-like substitutions; whole fruits instead of juices/smoothies, for example. 10almonds tip: stuffing dates with an almond each makes it very much like eating chocolate, experientially!
- Manage cravings: Dr. Hansen recommends distraction, and focusing on upping other healthy habits such as hydration, exercise, and getting more vegetables.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Which Sugars Are Healthier, And Which Are Just The Same?
- Mythbusting The Not-So-Sweet Science Of Sugar Addiction
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’ve been given opioids after surgery to take at home. What do I need to know?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Opioids are commonly prescribed when you’re discharged from hospital after surgery to help manage pain at home.
These strong painkillers may have unwanted side effects or harms, such as constipation, drowsiness or the risk of dependence.
However, there are steps you can take to minimise those harms and use opioids more safely as you recover from surgery.
Flystock/Shutterstock Which types of opioids are most common?
The most commonly prescribed opioids after surgery in Australia are oxycodone (brand names include Endone, OxyNorm) and tapentadol (Palexia).
In fact, about half of new oxycodone prescriptions in Australia occur after a recent hospital visit.
Most commonly, people will be given immediate-release opioids for their pain. These are quick-acting and are used to manage short-term pain.
Because they work quickly, their dose can be easily adjusted to manage current pain levels. Your doctor will provide instructions on how to adjust the dosage based on your pain levels.
Then there are slow-release opioids, which are specially formulated to slowly release the dose over about half to a full day. These may have “sustained-release”, “controlled-release” or “extended-release” on the box.
Slow-release formulations are primarily used for chronic or long-term pain. The slow-release form means the medicine does not have to be taken as often. However, it takes longer to have an effect compared with immediate-release, so it is not commonly used after surgery.
Controlling your pain after surgery is important. This allows you get up and start moving sooner, and recover faster. Moving around sooner after surgery prevents muscle wasting and harms associated with immobility, such as bed sores and blood clots.
Everyone’s pain levels and needs for pain medicines are different. Pain levels also decrease as your surgical wound heals, so you may need to take less of your medicine as you recover.
But there are also risks
As mentioned above, side effects of opioids include constipation and feeling drowsy or nauseous. The drowsiness can also make you more likely to fall over.
Opioids prescribed to manage pain at home after surgery are usually prescribed for short-term use.
But up to one in ten Australians still take them up to four months after surgery. One study found people didn’t know how to safely stop taking opioids.
Such long-term opioid use may lead to dependence and overdose. It can also reduce the medicine’s effectiveness. That’s because your body becomes used to the opioid and needs more of it to have the same effect.
Dependency and side effects are also more common with slow-release opioids than immediate-release opioids. This is because people are usually on slow-release opioids for longer.
Then there are concerns about “leftover” opioids. One study found 40% of participants were prescribed more than twice the amount they needed.
This results in unused opioids at home, which can be dangerous to the person and their family. Storing leftover opioids at home increases the risk of taking too much, sharing with others inappropriately, and using without doctor supervision.
Don’t stockpile your leftover opioids in your medicine cupboard. Take them to your pharmacy for safe disposal. Archer Photo/Shutterstock How to mimimise the risks
Before using opioids, speak to your doctor or pharmacist about using over-the-counter pain medicines such as paracetamol or anti-inflammatories such as ibuprofen (for example, Nurofen, Brufen) or diclofenac (for example, Voltaren, Fenac).
These can be quite effective at controlling pain and will lessen your need for opioids. They can often be used instead of opioids, but in some cases a combination of both is needed.
Other techniques to manage pain include physiotherapy, exercise, heat packs or ice packs. Speak to your doctor or pharmacist to discuss which techniques would benefit you the most.
However, if you do need opioids, there are some ways to make sure you use them safely and effectively:
- ask for immediate-release rather than slow-release opioids to lower your risk of side effects
- do not drink alcohol or take sleeping tablets while on opioids. This can increase any drowsiness, and lead to reduced alertness and slower breathing
- as you may be at higher risk of falls, remove trip hazards from your home and make sure you can safely get up off the sofa or bed and to the bathroom or kitchen
- before starting opioids, have a plan in place with your doctor or pharmacist about how and when to stop taking them. Opioids after surgery are ideally taken at the lowest possible dose for the shortest length of time.
A heat pack may help with pain relief, so you end up using fewer painkillers. New Africa/Shutterstock If you’re concerned about side effects
If you are concerned about side effects while taking opioids, speak to your pharmacist or doctor. Side effects include:
- constipation – your pharmacist will be able to give you lifestyle advice and recommend laxatives
- drowsiness – do not drive or operate heavy machinery. If you’re trying to stay awake during the day, but keep falling asleep, your dose may be too high and you should contact your doctor
- weakness and slowed breathing – this may be a sign of a more serious side effect such as respiratory depression which requires medical attention. Contact your doctor immediately.
If you’re having trouble stopping opioids
Talk to your doctor or pharmacist if you’re having trouble stopping opioids. They can give you alternatives to manage the pain and provide advice on gradually lowering your dose.
You may experience withdrawal effects, such as agitation, anxiety and insomnia, but your doctor and pharmacist can help you manage these.
How about leftover opioids?
After you have finished using opioids, take any leftovers to your local pharmacy to dispose of them safely, free of charge.
Do not share opioids with others and keep them away from others in the house who do not need them, as opioids can cause unintended harms if not used under the supervision of a medical professional. This could include accidental ingestion by children.
For more information, speak to your pharmacist or doctor. Choosing Wisely Australia also has free online information about managing pain and opioid medicines.
Katelyn Jauregui, PhD Candidate and Clinical Pharmacist, School of Pharmacy, Faculty of Medicine and Health, University of Sydney; Asad Patanwala, Professor, Sydney School of Pharmacy, University of Sydney; Jonathan Penm, Senior lecturer, School of Pharmacy, University of Sydney, and Shania Liu, Postdoctoral Research Fellow, Faculty of Medicine and Dentistry, University of Alberta
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Health Insurers Limit Coverage of Prosthetic Limbs, Questioning Their Medical Necessity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Michael Adams was researching health insurance options in 2023, he had one very specific requirement: coverage for prosthetic limbs.
Adams, 51, lost his right leg to cancer 40 years ago, and he has worn out more legs than he can count. He picked a gold plan on the Colorado health insurance marketplace that covered prosthetics, including microprocessor-controlled knees like the one he has used for many years. That function adds stability and helps prevent falls.
But when his leg needed replacing last January after about five years of everyday use, his new marketplace health plan wouldn’t authorize it. The roughly $50,000 leg with the electronically controlled knee wasn’t medically necessary, the insurer said, even though Colorado law leaves that determination up to the patient’s doctor, and his has prescribed a version of that leg for many years, starting when he had employer-sponsored coverage.
“The electronic prosthetic knee is life-changing,” said Adams, who lives in Lafayette, Colorado, with his wife and two kids. Without it, “it would be like going back to having a wooden leg like I did when I was a kid.” The microprocessor in the knee responds to different surfaces and inclines, stiffening up if it detects movement that indicates its user is falling.
People who need surgery to replace a joint typically don’t encounter similar coverage roadblocks. In 2021, 1.5 million knee or hip joint replacements were performed in United States hospitals and hospital-owned ambulatory facilities, according to the federal Agency for Healthcare Research and Quality, or AHRQ. The median price for a total hip or knee replacement without complications at top orthopedic hospitals was just over $68,000 in 2020, according to one analysis, though health plans often negotiate lower rates.
To people in the amputee community, the coverage disparity amounts to discrimination.
“Insurance covers a knee replacement if it’s covered with skin, but if it’s covered with plastic, it’s not going to cover it,” said Jeffrey Cain, a family physician and former chair of the board of the Amputee Coalition, an advocacy group. Cain wears two prosthetic legs, having lost his after an airplane accident nearly 30 years ago.
AHIP, a trade group for health plans, said health plans generally provide coverage when the prosthetic is determined to be medically necessary, such as to replace a body part or function for walking and day-to-day activity. In practice, though, prosthetic coverage by private health plans varies tremendously, said Ashlie White, chief strategy and programs officer at the Amputee Coalition. Even though coverage for basic prostheses may be included in a plan, “often insurance companies will put caps on the devices and restrictions on the types of devices approved,” White said.
An estimated 2.3 million people are living with limb loss in the U.S., according to an analysis by Avalere, a health care consulting company. That number is expected to as much as double in coming years as people age and a growing number lose limbs to diabetes, trauma, and other medical problems.
Fewer than half of people with limb loss have been prescribed a prosthesis, according to a report by the AHRQ. Plans may deny coverage for prosthetic limbs by claiming they aren’t medically necessary or are experimental devices, even though microprocessor-controlled knees like Adams’ have been in use for decades.
Cain was instrumental in getting passed a 2000 Colorado law that requires insurers to cover prosthetic arms and legs at parity with Medicare, which requires coverage with a 20% coinsurance payment. Since that measure was enacted, about half of states have passed “insurance fairness” laws that require prosthetic coverage on par with other covered medical services in a plan or laws that require coverage of prostheses that enable people to do sports. But these laws apply only to plans regulated by the state. Over half of people with private coverage are in plans not governed by state law.
The Medicare program’s 80% coverage of prosthetic limbs mirrors its coverage for other services. Still, an October report by the Government Accountability Office found that only 30% of beneficiaries who lost a limb in 2016 received a prosthesis in the following three years.
Cost is a factor for many people.
“No matter your coverage, most people have to pay something on that device,” White said. As a result, “many people will be on a payment plan for their device,” she said. Some may take out loans.
The federal Consumer Financial Protection Bureau has proposed a rule that would prohibit lenders from repossessing medical devices such as wheelchairs and prosthetic limbs if people can’t repay their loans.
“It is a replacement limb,” said White, whose organization has heard of several cases in which lenders have repossessed wheelchairs or prostheses. Repossession is “literally a punishment to the individual.”
Adams ultimately owed a coinsurance payment of about $4,000 for his new leg, which reflected his portion of the insurer’s negotiated rate for the knee and foot portion of the leg but did not include the costly part that fits around his stump, which didn’t need replacing. The insurer approved the prosthetic leg on appeal, claiming it had made an administrative error, Adams said.
“We’re fortunate that we’re able to afford that 20%,” said Adams, who is a self-employed leadership consultant.
Leah Kaplan doesn’t have that financial flexibility. Born without a left hand, she did not have a prosthetic limb until a few years ago.
Growing up, “I didn’t want more reasons to be stared at,” said Kaplan, 32, of her decision not to use a prosthesis. A few years ago, the cycling enthusiast got a prosthetic hand specially designed for use with her bike. That device was covered under the health plan she has through her county government job in Spokane, Washington, helping developmentally disabled people transition from school to work.
But when she tried to get approval for a prosthetic hand to use for everyday activities, her health plan turned her down. The myoelectric hand she requested would respond to electrical impulses in her arm that would move the hand to perform certain actions. Without insurance coverage, the hand would cost her just over $46,000, which she said she can’t afford.
Working with her doctor, she has appealed the decision to her insurer and been denied three times. Kaplan said she’s still not sure exactly what the rationale is, except that the insurer has questioned the medical necessity of the prosthetic hand. The next step is to file an appeal with an independent review organization certified by the state insurance commissioner’s office.
A prosthetic hand is not a luxury device, Kaplan said. The prosthetic clinic has ordered the hand and made the customized socket that will fit around the end of her arm. But until insurance coverage is sorted out, she can’t use it.
At this point she feels defeated. “I’ve been waiting for this for so long,” Kaplan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: