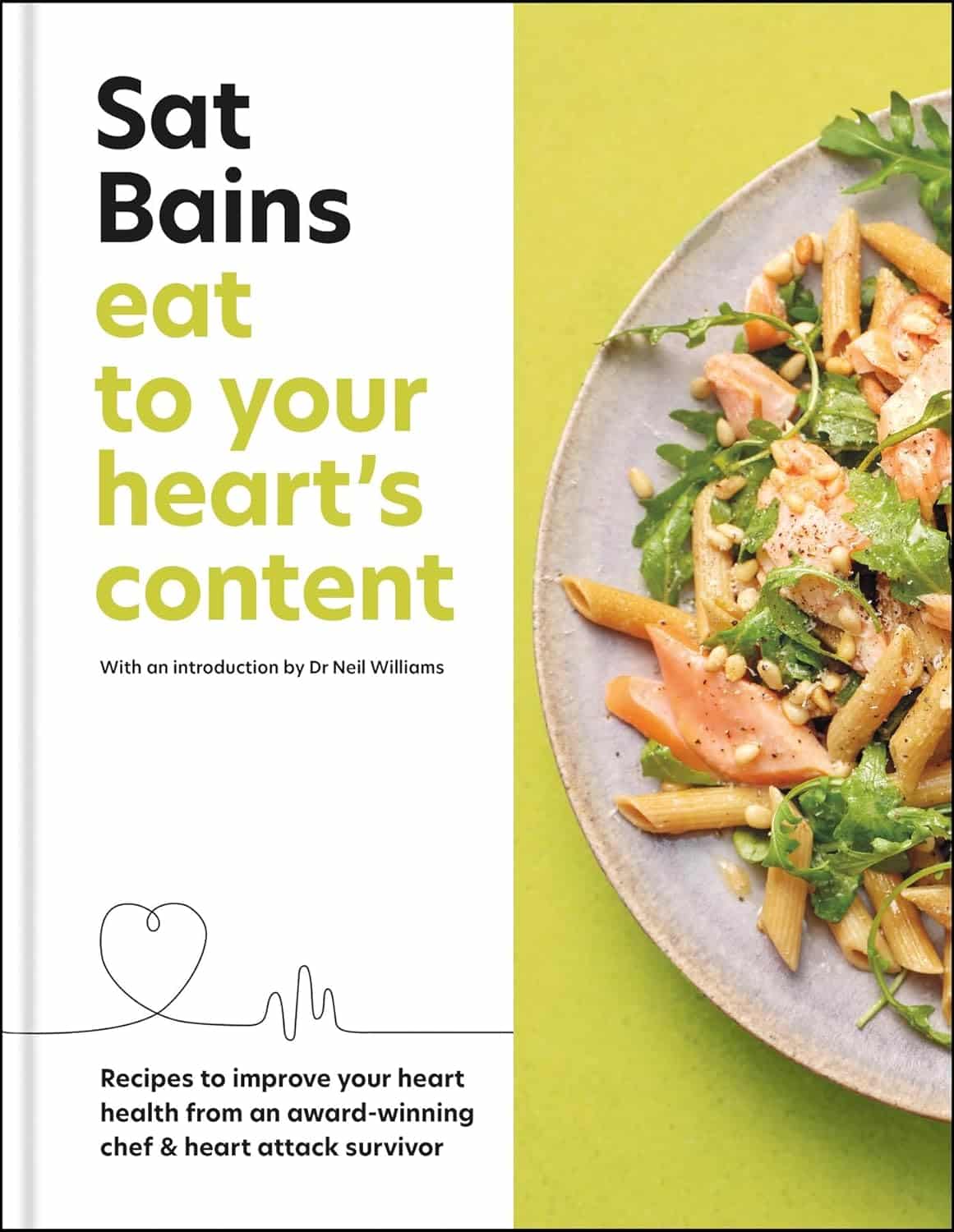
Eat to Your Heart’s Content – by Dr. Sat Bains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Making food heart-healthy and tasty is a challenge that vexes many, but it doesn’t have to be so difficult.
Dr. Sat Bains, a professional chef with multiple Michelin stars to his name, is an expert on “tasty”, and after surviving a heart attack himself, he’s become an expert on “heart-healthy” since then.
The book contains not only the recipes (of which there are 68, by the way), but also large sections of explanation of what makes various ingredients or methods heart-healthy or heart-unhealthy.
There’s science in there too, and these sections were written under the guidance of Dr. Neil Williams, a lecturer in physiology and nutrition.
You may be wondering as to why the author himself has a doctorate too; in fact he has three, none of which are relevant:
- Doctor of Arts
- Doctor of Laws
- Doctor of Hospitality (Honorary)
…but we prefix “Dr.” when people are that and he is that. The expertise we’re getting here though is really his culinary skill and extracurricular heart-healthy learning, plus Dr. Williams’ actual professional health guidance.
Bottom line: if you’d like heart-healthy recipes with restaurant-level glamour, this book is a fine choice.
Click here to check out Eat To Your Heart’s Content, and look after yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Scattered Minds – by Dr. Gabor Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This was not the first book that Dr. Maté sat down to write, by far. But it was the first that he actually completed. Guess why.
Writing from a position of both personal and professional experience and understanding, Dr. Maté explores the inaptly-named Attention Deficit Disorder (if anything, there’s often a surplus of attention, just, to anything and everything rather than necessarily what would be most productive in the moment), its etiology, its presentation, and its management.
This is a more enjoyable book than some others by the same author, as while this condition certainly isn’t without its share of woes (often, for example, a cycle of frustration and shame re “why can’t I just do the things; this is ruining my life and it would be so easy if I could just do the things!”), it’s not nearly so bleak as entire books about trauma, addiction, and so forth (worthy as those books also are).
Dr. Maté frames it specifically as a development disorder, and one whereby with work, we can do the development later that (story of an ADHDer’s life) we should have done earlier but didn’t. In terms of practical advice, he includes a program for effecting this change, including as an adult.
The style is easy-reading, in small chapters, with ADHD’d-up readers in mind, giving a strong sense of speeding pleasantly through the book.
Bottom line: when it’s a book by Dr. Gabor Maté, you know it’s going to be good, and this is no exception. Certainly read it if you, anyone you care about, or even anyone you just spend a lot of time around, has ADHD or similar.
Click here to check out Scattered Minds, and unscatter yours!
Share This Post
-
The “Five Tibetan Rites” & Why To Do Them!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Spinning Around
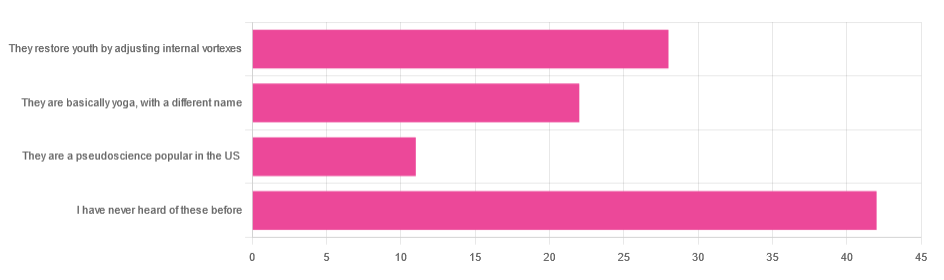
In Tuesday’s newsletter, we asked you for your opinion of the “Five Tibetan Rites”, and got the above-depicted, below-described, set of responses:
- About 41% said “I have never heard of these before”
- About 27% said “they restore youth by adjusting internal vortexes”
- About 22% said “they are basically yoga, by a different name”
- About 11% said “they are a pseudoscience popular in the US”
So what does the science say?
The Five Tibetan Rites are five Tibetan rites: True or False?
False, though this is more question of social science than of health science, so we’ll not count it against them for having a misleading name.
The first known mentioning of the “Five Tibetan Rites” is by an American named Peter Kelder, who in 1939 published, through a small LA occult-specialized publishing house, a booklet called “The Eye of Revelation”. This work was then varyingly republished, repackaged, and occasionally expanded upon by Kelder or other American authors, including Chris Kilham’s popular 1994 book “The Five Tibetans”.
The “Five Tibetan Rites” are unknown as such in Tibet, except for what awareness of them has been raised by people asking about them in the context of the American phenomenon.
Here’s a good history book, for those interested:
The author didn’t originally set out to “debunk” anything, and is himself a keen spiritualist (and practitioner of the five rites), but he was curious about the origins of the rites, and ultimately found them—as a collection of five rites, and the other assorted advices given by Kelder—to be an American synthesis in the whole, each part inspired by various different physical practices (some of them hatha yoga, some from the then-popular German gymnastics movement, some purely American spiritualism, all available in books that were popular in California in the early 1900s).
You may be wondering: why didn’t Kelder just say that, then, instead of telling stories of an ancient Tibetan tradition that empirically does not exist? The answer to this lies again in social science not health science, but it’s been argued that it’s common for Westerners to “pick ‘n’ mix” ideas from the East, champion them as inscrutably mystical, and (since they are inscrutable) then simply decide how to interpret and represent them. Here’s an excellent book on this, if you’re interested:
(in Kelder’s case, this meant that “there’s a Tibetan tradition, trust me” was thus more marketable in the West than “I read these books in LA”)
They are at least five rites: True or False?
True! If we use the broad definition of “rite” as “something done repeatedly in a solemn fashion”. And there are indeed five of them:
- Spinning around (good for balance)
- Leg raises (this one’s from German gymnastics)
- Kneeling back bend (various possible sources)
- Tabletop (hatha yoga, amongst others)
- Pendulum (hatha yoga, amongst others) ← you may recognize this one from the Sun Salutation
You can see them demonstrated here:
Click Here If The Embedded Video Doesn’t Load Automatically
Kelder also advocated for what was basically the Hay Diet (named not for the substance but for William Hay; it involved separating foods into acid and alkali, not necessarily according to the actual pH of the foods, and combining only “acid” foods or only “alkali” foods at a time), which was popular at the time, but has since been rejected as without scientific merit. Kelder referred to this as “the sixth rite”.
The Five Rites restore youth by adjusting internal vortexes: True or False?
False, in any scientific sense of that statement. Scientifically speaking, the body does not have vortexes to adjust, therefore that is not the mechanism of action.
Spiritually speaking, who knows? Not us, a humble health science publication.
The Five Rites are a pseudoscience popular in the US: True or False?
True, if 27% of those who responded of our mostly North American readership can be considered as representative of what is popular.
However…
“Pseudoscience” gets thrown around a lot as a bad word; it’s often used as a criticism, but it doesn’t have to be. Consider:
A small child who hears about “eating the rainbow” and mistakenly understands that we are all fuelled by internal rainbows that need powering-up by eating fruits and vegetables of different colors, and then does so…
…does not hold a remotely scientific view of how things are happening, but is nevertheless doing the correct thing as recommended by our best current science.
It’s thus a little similar with the five rites. Because…
The Five Rites are at least good for our health: True or False?
True! They are great for the health.
The first one (spinning around) is good for balance. Science would recommend doing it both ways rather than just one way, but one is not bad. It trains balance, trains our stabilizing muscles, and confuses our heart a bit (in a good way).
See also: Fall Special (How To Not Fall, And Not Get Injured If You Do)
The second one (leg raises) is excellent for core strength, which in turn helps keep our organs where they are supposed to be (this is a bigger health issue than most people realise, because “out of sight, out of mind”), which is beneficial for many aspects of our health!
See also: Visceral Belly Fat & How To Lose It ← visceral fat is the fat that surrounds your internal organs; too much there becomes a problem!
The third, fourth, and fifth ones stretch our spine (healthily), strengthen our back, and in the cases of the fourth and fifth ones, are good full-body exercises for building strength, and maintaining muscle mass and mobility.
See also: Building & Maintaining Mobility
So in short…
If you’ve been enjoying the Five Rites, by all means keep on doing them; they might not be Tibetan (or an ancient practice, as presented), and any mystical aspect is beyond the scope of our health science publication, but they are great for the health in science-based ways!
Take care!
Share This Post
-
Dates vs Grapes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dates to grapes, we picked the dates.
Why?
It’s not close:
In terms of macros, dates have 4x the carbs and/but 8x the fiber, making for the lower glycemic index. Also, for what it’s worth, they have nearly 4x the protein, but probably nobody is eating either of these fruits for the protein. In any case, it’s an easy and clear win for dates in the category of macros.
In the category of vitamins, dates have more of vitamins B2, B3, B5, B6, B9, and choline, while grapes have more of vitamins B1, C, E, and K, making for a 6:4 win for dates.
When it comes to minerals, it’s more one-sided: dates have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while grapes have more manganese. An easy win for dates here.
Of course, enjoy either or both (diversity is good), but if you’re looking for nutrient density, dates are where it’s at.
Want to learn more?
You might like:
Can We Drink To Good Health? ← while there are polyphenols such as resveratrol in red wine that per se would boost heart health, there’s so little per glass that you may need 100–1000 glasses per day to get the dosage that provides benefits in mouse studies.
If you’re not a mouse, you might even need more than that!
To this end, many people prefer resveratrol supplementation ← link is to an example product on Amazon, but there are plenty more so feel free to shop around 😎
Enjoy!
Share This Post
Related Posts
-
The Checklist Manifesto – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gawande, himself a general surgeon, uses checklists a lot. He is, unequivocally, an expert in his field. He “shouldn’t” need a checklist to tell him to do such things as “Check you have the correct patient”. But checklists are there as a safety net. And, famously, “safety regulations are written in blood”, after all.
And, who amongst us has never made such a “silly” error? From forgetting to turn the oven on, to forgetting to take the handbrake off, it takes only a momentary distraction to think we’ve done something we haven’t.
You may be wondering: why a whole book on this? Is it just many examples of the usefulness of checklists? Because I’m already sold on that, so, what else am I going to get out of it?
Dr. Gawande also explains in clear terms:
- How to optimize “all necessary steps” with “as few steps as possible”
- The important difference between read-do checklists and do-confirm checklists
- To what extent we should try to account for the unexpected
- How to improve compliance (i.e., making sure you actually use it, no matter how tempting it will be to go “yeah this is automatic for me now” and gloss over it)
- The role of checklists in teams, and in passing on knowledge
…and more.
Bottom line: if you’ve ever tried to make tea without putting the tea-leaves in the pot, this is the book that will help you avoid making more costly mistakes—whatever your area of activity or interest.
Click here to check out the Checklist Manifesto, and make fewer mistakes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Non-Alcoholic Drinker – by James Ellison
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A mere few decades ago, it was often considered antisocial not to smoke. These days, it’s antisocial if you do. The same social change is starting to happen now with alcohol—Millennials are drinking much less than they did in decades past, and Gen Z are hardly drinking at all.
The author, himself a Baby Boomer, champions the cause of mindful, and/but joyful, abstemiousness. Which latter two words don’t often go together, but in this case, he really has put in a lot of work to make non-alcoholic drinking as exciting, fun, and sophisticated as alcoholic drinking always marketed itself to be.
The mocktail recipes in this book are an order of magnitude better than any others this reviewer has encountered before, and did you know they have non-alcoholic bitters now? As in, the cocktail ingredient. Nor is it the only non-alcoholic botanical used, and the ingredients in general are as varied and flavorful, if not sometimes more so, than many that get used in alcoholic mixes.
This book is a very far cry from “rum and coke without the rum”, and instead will have you excited to go ingredient-shopping, and even more excited when you find out how great non-alcoholic things can taste if given the right attention.
As a convenient extra touch, all the ingredients he mentions are available from Amazon, which takes away the fear of “ok, but where do I get…” when it comes to getting things in.
The book does cover things besides just the recipes themselves though, and also talks the reader through navigating non-alcoholism when friends of your own age (unless you’re one of our younger readers) are probably mostly still partying with alcohol.
Really, the biggest value of this book is the recipes, though.
Bottom line: if you’d like to entertain with sophistication and grace and/but not with alcohol, or even just take up a fun new healthy hobby, this book is by far the best book on non-alcoholic mixology that this reviewer has seen to date.
Click here to check out The Non-Alcoholic Drinker, and get mixing non-alcoholically!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get Better Sleep: Beyond “Sleep Hygiene”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Better Sleep, Better Life!
This is Arianna Huffington. Yes, that Huffington, of the Huffington Post. But! She’s also the CEO of Thrive Global, a behavior change tech company with the mission of changing the way we work and live—in particular, by challenging the idea that burnout is the required price of success.
The power of better sleep
Sleep is a very important, but most often neglected, part of good health. Here are some of Huffington’s top insights from her tech company Thrive, and as per her “Sleep Revolution” initiative.
Follow your circadian rhythm
Are you a night owl or a morning lark? Whichever it is, roll with it, and plan around that if your lifestyle allows for such. While it is possible to change from one to the other, we do have a predisposition towards one or the other, and will generally function best when not fighting it.
This came about, by the way, because we evolved to have half of us awake in the mornings and half in the evenings, to keep us all safe. Socially we’ve marched onwards from that point in evolutionary history, but our bodies are about a hundred generations behind the times, and that’s just what we have to work with!
Don’t be afraid (or ashamed!) to take naps
Naps, done right, can be very good for the health—especially if we had a bad night’s sleep the previous night.
Thrive found that workers are more productive when they have nap rooms, and (following on a little from the previous point) are allowed to sleep in or work from home.
See also: How To Nap Like A Pro (No More “Sleep Hangovers”!)
Make sure you have personal space available in bed
The correlation between relationship satisfaction and sleeping close to one’s partner has been found to be so high that it’s even proportional: the further away a couple sleeps from each other, the less happy they are. But…
Partners who got good sleep the previous night, will be more likely to want intimacy on any given night—at a rate of an extra 14% per extra hour of sleep the previous night. So, there’s a trade-off, as having more room in bed tends to result in better sleep. Time to get a bigger bed?
What gets measured, gets done
This goes for sleep, too! Not only does dream-journaling in the morning cue your subconscious to prepare to dream well the following night, but also, sleep trackers and sleep monitoring apps go a very long way to improving sleep quality, even if no extra steps are consciously taken to “score better”.
We’ve previously reviewed some of the most popular sleep apps; you can check out for yourself how they measured up:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: