Stop Sabotaging Your Gut
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
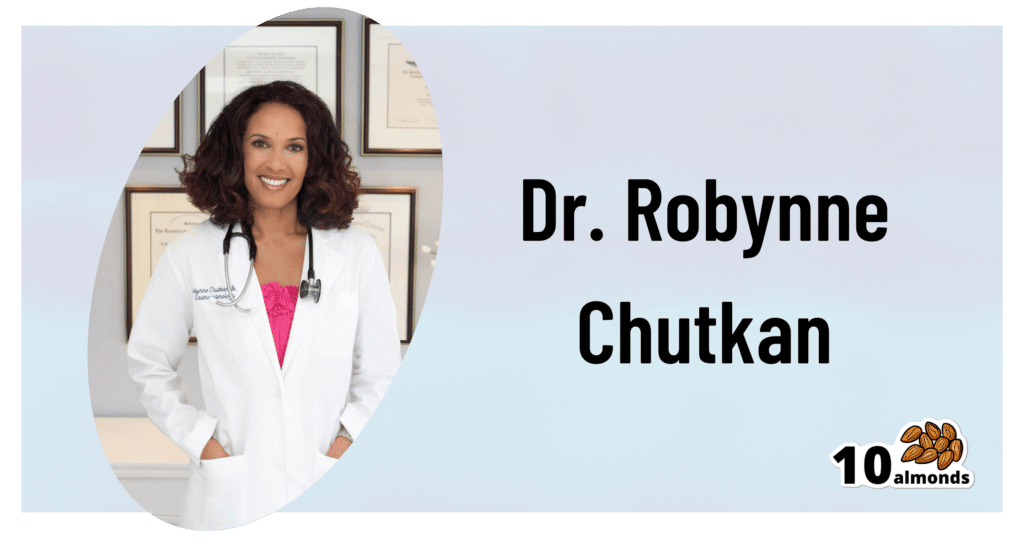
This is Dr. Robynne Chutkan. She’s an integrative gastroenterologist, and founder of the Digestive Center for Wellness, in Washington DC, which for the past 20 years has been dedicated to uncovering the root causes of gastrointestinal disorders, while the therapeutic side of things has been focused on microbial optimization, nutritional therapy, mind-body techniques, and lifestyle changes.
In other words, maximal health for minimal medicalization.
So… What does she want us to know?
Live dirty
While attentive handwashing is important to avoid the spread of communicable diseases*, excessive cleanliness in general can result in an immune system that has no idea how to deal with pathogens when exposure does finally occur.
*See also: The Truth About Handwashing
This goes doubly for babies: especially those who were born by c-section and thus missed out on getting colonized by vaginal bacteria, and especially those who are not breast-fed, and thus miss out on nutrients given in breast milk that are made solely for the benefit of certain symbiotic bacteria (humans can’t even digest those particular nutrients, we literally evolved to produce some nutrients solely for the bacteria).
See also: Breast Milk’s Benefits That Are (So Far) Not Replicable
However, it still goes for the rest of us who are not babies, too. We could, Dr. Chutkan tells us, stand to wash less in general, and definitely ease up on antibacterial soaps and so forth.
See also: Should You Shower Daily?
Take antibiotics only if absolutely necessary (and avoid taking them by proxy)
Dr. Chutkan describes antibiotics as the single biggest threat to our microbiome, not just because of overprescription, but also the antibiotics that are used in animal agriculture and thus enter the food chain (and thus, enter us, if we eat animal products).
Still, while the antibiotics meat/dairy-enjoyers will get from food are better avoided, antibiotics actually taken directly are even worse, and are absolutely a “scorched earth” tactic against whatever they’re being prescribed for.
See also: Antibiotics? Think Thrice ← which also brings up “Four Ways Antibiotics Can Kill You”; seriously, the risks of antibiotics are not to be underestimated, including the risks associated only with them working exactly as intended—let alone if something goes wrong.
Probiotics won’t save you
While like any gastroenterologist (or really, almost any person in general), she notes that probiotics can give a boost to health. However, she wants us to know about two shortcomings that are little-discussed:
1) Your body has a collection of microbiomes each with their own needs, and while it is possible to take “generally good” bacteria in probiotics and assume they’ll do good, taking Lactobacillus sp. will do nothing for a shortage of Bifidobacteria sp, and even taking the correct genus can have similar shortcomings if a different species of that genus is needed, e.g. taking L. acidophilus will do nothing for a shortage of L. reuteri.
It’d be like a person with a vitamin D deficiency taking vitamin B12 supplements and wondering why they’re not getting better.
2) Probiotics are often wasted if not taken mindfully of their recipient environment. For example, most gut bacteria only live for about 20 minutes in the gut. They’re usually inactive in the supplement form, they’re activated in the presence of heat and moisture and appropriate pH etc, and then the clock is ticking for them to thrive or die.
This means that if you take a supplement offering two billion strains of good gut bacteria, and you take it on an empty stomach, then congratulations, 20 minutes later, they’re mostly dead, because they had nothing to eat. Or if you take it after drinking a soda, congratulations, they’re mostly dead because not only were they starved, but also their competing “bad” microbes weren’t starved and changed the environment to make it worse for the “good” ones.
For this reason, taking probiotics with (or immediately after) plenty of fiber is best.
This is all accentuated if you’re recovering from using antibiotics, by the way.
Imagine: a nuclear war devastates the population of the Earth. Some astronauts manage to safely return, finding a mostly-dead world covered in nuclear winter. Is the addition of a few astronauts going to quickly repopulate the world? No, of course not. They are few, the death toll is many, and the environment is very hostile to life. A hundred years later, the population will be pretty much the same—a few straggling survivors.
It’s the same after taking antibiotics, just, generations pass in minutes instead of decades. You can’t wipe out almost everything beneficial in the gut, create a hostile environment there, throw in a couple of probiotic gummies, and expect the population to bounce back.
That said, although “probiotics will not save you”, they can help provided you give them a nice soft bed of fiber to land on, some is better than none, and guessing at what strains are needed is better than giving nothing.
See also: How Much Difference Do Probiotic Supplements Make, Really?
What she recommends
So to recap, we’ve had:
- Wash less, and/or with less harsh chemicals
- Avoid antibiotics like the plague, unless you literally have The Plague, for which the treatment is indeed antibiotics
- Avoid antibiotic-contaminated foods, which in the US is pretty much all animal products unless it’s, for example, your own back-yard hens whom you did not give antibiotics. Do not fall for greenwashing aesthetics in the packaging of “happy cows” and their beef, milk, etc, “happy hens” and their meat, eggs, etc… If it doesn’t explicitly claim to be free from the use of antibiotics, then antibiotics were almost certainly used.
- Dr. Chutkan herself is not even vegan, by the way, but very much wants us to be able to make informed choices about this, and does recommend at least a “plants-forward” diet, for the avoiding-antibiotics reason and for the plenty-of-fiber reason, amongst others.
- Consider probiotics, but don’t expect them to work miracles by themselves; you’ve got to help them to help you.
- Dr. Chutkan also recommends getting microbiome tests done if you think something might be amiss, and then you can supplement with probiotics in a more targetted fashion instead of guessing at what species is needed where.
She also recommends, of course, a good gut-healthy diet in general, especially “leafy green things that were recently alive; not powders”, beans, and nuts, while avoiding gut-unhealthy things such as sugars-without-fiber, alcohol, or some gut-harmful additives (such as most artificial sweeteners, although stevia is a gut-healthy exception, and sucralose is ok in moderation).
For more on gut-healthy eating, check out:
Make Friends With Your Gut (You Can Thank Us Later)
Want to know more from Dr. Chutkan?
We recently reviewed an excellent book of hers:
The Anti-Viral Gut: Tackling Pathogens From The Inside Out – by Dr. Robynne Chutkan
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Staring At The Sun – by Dr. Irvin Yalom
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note first: there are two editions of this book; the content is the same, but the cover is different. So if in your region it has a bright yellow cover and the subtitle is the excitable “Overcoming The Terror Of Death” rather than the more measured “Being At Peace With Your Own Mortality”, that is why; different regional publishers made different choices.
For most of us, dying is the last thing we want to do. We may fear it; we may ignore it; we may try to beat it—but it’s a constant existential threat whether we want it or not.
This book is about “death anxiety”, either direct (conscious fear of impending death) or sublimated (not necessarily realising what we’re avoiding thinking about it). In its broadest sense, the fear of death can be described as rational. But angst about it probably won’t help, so this book looks to help us overcome that.
The style of the book is largely anecdotal, in which the author uses examples from his therapeutic practice to illustrate ways in which the fear of death can manifest, and ways in which it can be managed healthily.
Subjective criticism: while this author developed existential therapy, many of the ideas in this book lean heavily on the psychodynamic approach derived from Freud, and this reviewer isn’t a fan of that. But nevertheless, many of the examples here are thought-provoking and useful, so it is not too strong a criticism.
Bottom line: there are many ways to manage one’s mortality, and this book brings attention to a range of possibilities.
Click here to check out Staring At The Sun, and manage your mortality!
Share This Post
-
PlantYou: Scrappy Cooking – by Carleigh Bodrug
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a book that took “whole foods plant-based diet” and ran with it.
“Whole foods”, you say? Carleigh Bodrug has you covered in this guide to using pretty much everything.
One of the greatest strengths of the book is its “Got this? Make that” section, for using up those odds and ends that you’d normally toss.
You may be thinking: “ok, but if to use this unusual ingredient I have to buy four other ingredients to make this recipe, generating waste from those other ingredients, then this was a bad idea”, but fear not.
Bodrug covers that too, and in many cases leftover “would get wasted” ingredients can get turned into stuff that can go into longer-term storage one way or another, to use at leisure.
Which also means that on the day “there’s nothing in the house to eat” and you don’t want to go grocery-shopping, or if some global disaster causes the supply lines to fail and the stores become empty (that could never happen though, right?), you will have the mystical ability to conjure a good meal out of assorted odds and ends that you stored because of this book.
Bottom line: if you love food and hate food waste, this is a great book for you.
Click here to check out Scrappy Cooking, and do domestic magic!
Share This Post
-
HBD: The Human Being Diet – by Petronella Ravenshear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t often review diet books, so why did this one catch our attention? The answer lies in its comprehensive nature without being excessively long and complex.
Ravenshear (a nutritionist) brings a focus on metabolic balance, and what will and won’t work for keeping it healthy.
The first part of the book is mostly informational; covering such things as blood sugar balance, gut health, hormones, and circadian rhythm considerations, amongst others.
The second, larger part of the book is mostly instructional; do this and that, don’t do the other, guidelines on quantities and timings, and what things may be different for some people, and what to do about those.
The style is conversational and light, but well-grounded in good science.
Bottom line: if you’d like a “one-stop shop” for giving your diet an overhaul, this book is a fine choice.
Click here to check out the Human Being Diet, and enjoy the best of health!
Share This Post
Related Posts
-
Felt Time – by Dr. Marc Wittmann
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book goes far beyond the obvious “time flies when you’re having fun / passes slowly when bored”, or “time seems quicker as we get older”. It does address those topics too, but even in doing so, unravels deeper intricacies within.
The author, a research psychologist, includes plenty of reference to actual hard science here, and even beyond subjective self-reports. For example, you know how time seems to slow down upon immediate apparent threat of violent death (e.g. while crashing, while falling, or other more “violent human” options)? We learn of an experiment conducted in an amusement park, where during a fear-inducing (but actually safe) plummet, subjective time slows down yes, but measures of objective perception and cognition remained the same. So much for adrenal superpowers when it comes to the brain!
We also learn about what we can change, to change our perception of time—in either direction, which is a neat collection of tricks to know.
The style is on the dryer end of pop-sci; we suspect that being translated from German didn’t help its levity. That said, it’s not scientifically dense either (i.e. not a lot of jargon), though it does have many references (which we like to see).
Bottom line: if you’ve ever wished time could go more quickly or more slowly, this book can help with that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Understanding Cellulitis: Skin And Soft Tissue Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference between a minor passing skin complaint, and a skin condition that’s indicative of something more serious? Dr. Thomas Watchman explains:
More than skin-deep
Cellulitis sounds benign enough, like having a little cellulite perhaps, but in fact it means an infection of the skin and—critically—the underlying soft tissues.
Normally, the skin acts as a barrier against infections, but this barrier can be breached by physical trauma (i.e. an injury that broke the skin), eczema, fungal nail infections, skin ulcers, and other similar things that disrupt the skin’s ability to protect us.
Things to watch out for: Dr. Watchman advises we keep an eye out for warm, reddened skin, swelling, and blisters. Specifically, a golden-yellow crust to these likely indicates a Staphylococcus aureus infection (hence the name).
There’s a scale of degrees of severity:
- Class 1: No systemic toxicity or comorbidities
- Class 2: Systemic toxicity or comorbidities present
- Class 3: Significant systemic toxicity or comorbidities with risk of significant deterioration
- Class 4: Sepsis or life-threatening infection
…with antibiotics being recommended in the latter two cases there, or in other cases for frail, young, old, or immunocompromised patients. Given the rather “scorched earth” results of antibiotics (they cause a lot of collateral iatrogenic damage), this can be taken as a sign of how seriously such infections should be taken.
For more about all this, including visual guides, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Of Brains & Breakouts: The Brain-Skin Doctor
- Beyond Supplements: The Real Immune-Boosters!
- Antibiotics? You Might Want To Think Thrice
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Non-Sleep Deep Rest: A Neurobiologist’s Take
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to get many benefits of sleep, while awake!
Today we’re talking about Dr. Andrew Huberman, a neuroscientist and professor in the department of neurobiology at Stanford School of Medicine.
He’s also a popular podcaster, and as his Wikipedia page notes:
❝In episodes lasting several hours, Huberman talks about the state of research in a specific topic, both within and outside his specialty❞
Today, we won’t be taking hours, and we will be taking notes from within his field of specialty (neurobiology). Specifically, in this case:
Non-Sleep Deep Rest (NSDR)
What is it? To quote from his own dedicated site on the topic:
❝What is NSDR (Yoga Nidra)? Non-Sleep Deep Rest, also known as NSDR, is a method of deep relaxation developed by Dr. Andrew Huberman, a neuroscientist at Stanford University School of Medicine.
It’s a process that combines controlled breathing and detailed body scanning to bring you into a state of heightened awareness and profound relaxation. The main purpose of NSDR is to reduce stress, enhance focus, and improve overall well-being.❞
While it seems a bit bold of Dr. Huberman to claim that he developed yoga nidra, it is nevertheless reassuring to get a neurobiologist’s view on this:
How it works, by science
Dr. Huberman says that by monitoring EEG readings during NSDR, we can see how the brain slows down. Measurably!
- It goes from an active beta range of 13–30 Hz (normal waking) to a conscious meditation state of an alpha range of 8–13 Hz.
- However, with practice, it can drop further, into a theta range of 4–8 Hz.
- Ultimately, sustained SSDR practice can get us to 0.5–3 Hz.
This means that the brain is functioning in the delta range, something that typically only occurs during our deepest sleep.
You may be wondering: why is delta lower than theta? That’s not how I remember the Greek alphabet being ordered!
Indeed, while the Greek alphabet goes alpha beta gamma delta epsilon zeta eta theta (and so on), the brainwave frequency bands are:
- Gamma = concentrated focus, >30 Hz
- Beta = normal waking, 13–30 Hz
- Alpha = relaxed state, 8–13 Hz
- Theta = light sleep, 4–8 Hz
- Delta = deep sleep, 1–4 Hz
Source: Sleep Foundation ← with a nice infographic there too
NSDR uses somatic cues to engage our parasympathetic nervous system, which in turn enables us to reach those states. The steps are simple:
- Pick a time and place when you won’t be disturbed
- Lie on your back and make yourself comfortable
- Close your eyes as soon as you wish, and now that you’ve closed them, imagine closing them again. And again.
- Slowly bring your attention to each part of your body in turn, from head to toe. As your attention goes to each part, allow it to relax more.
- If you wish, you can repeat this process for another wave, or even a third.
- Find yourself well-rested!
Note: this engagement of the parasympathetic nervous system and slowing down of brain activity accesses restorative states not normally available while waking, but 10 minutes of NSDR will not replace 7–9 hours of sleep; nor will it give you the vital benefits of REM sleep specifically.
So: it’s an adjunct, not a replacement
Want to try it, but not sure where/how to start?
When you’re ready, let Dr. Huberman himself guide you through it in this shortish (10:49) soundtrack:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to try it, but not right now? Bookmark it for later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: