Does Your Butt…Wink?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What is a Butt Wink?
A “butt wink” is a common issue that occurs during squatting exercises.
Now, we’ve talked about the benefits of squatting countless times (see here or here for just a few examples). As with all exercises, using the correct technique is imperative, helping to both reduce injury and maximize gain.
Given butt winks are a common issue when squatting, we thought it natural to devote an article to it.
So, a butt wink happens when, at the bottom of your squat position, your pelvis tucks rotates backward (otherwise known as a “posterior pelvic tilt”) and the lower back rounds. This motion looks like a slight ‘wink’, hence the name.
How to Avoid Butt Winking
When the pelvis tucks under and the spine rounds, it can put undue pressure on the lumbar discs. This is especially risky when squatting with weights, as it can exacerbate the stress on the spine.
To avoid a butt wink, it’s important to maintain a neutral spine throughout the squat and to work on flexibility and strength in the hips, glutes, and hamstrings. Adjusting the stance width or foot angle during squats can also help in maintaining proper form.
A visual representation would likely work better than our attempt at describing what to do, so without further ado, here’s today’s video:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Half of Australians in aged care have depression. Psychological therapy could help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
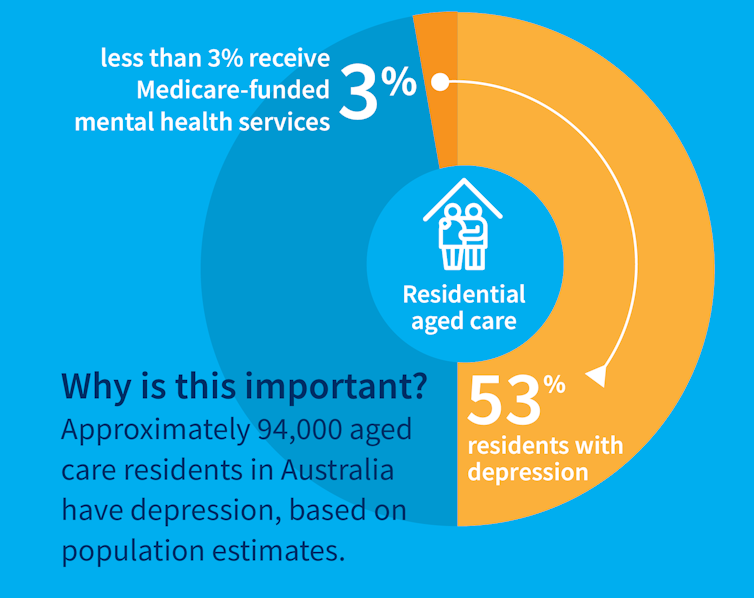
While many people maintain positive emotional wellbeing as they age, around half of older Australians living in residential aged care have significant levels of depression. Symptoms such as low mood, lack of interest or pleasure in life and difficulty sleeping are common.
Rates of depression in aged care appear to be increasing, and without adequate treatment, symptoms can be enduring and significantly impair older adults’ quality of life.
But only a minority of aged care residents with depression receive services specific to the condition. Less than 3% of Australian aged care residents access Medicare-subsidised mental health services, such as consultations with a psychologist or psychiatrist, each year.
Cochrane AustraliaInstead, residents are typically prescribed a medication by their GP to manage their mental health, which they often take for several months or years. A recent study found six in ten Australian aged care residents take antidepressants.
While antidepressant medications may help many people, we lack robust evidence on whether they work for aged care residents with depression. Researchers have described “serious limitations of the current standard of care” in reference to the widespread use of antidepressants to treat frail older people with depression.
Given this, we wanted to find out whether psychological therapies can help manage depression in this group. These treatments address factors contributing to people’s distress and provide them with skills to manage their symptoms and improve their day-to-day lives. But to date researchers, care providers and policy makers haven’t had clear information about their effectiveness for treating depression among older people in residential aged care.
The good news is the evidence we published today suggests psychological therapies may be an effective approach for people living in aged care.
We reviewed the evidence
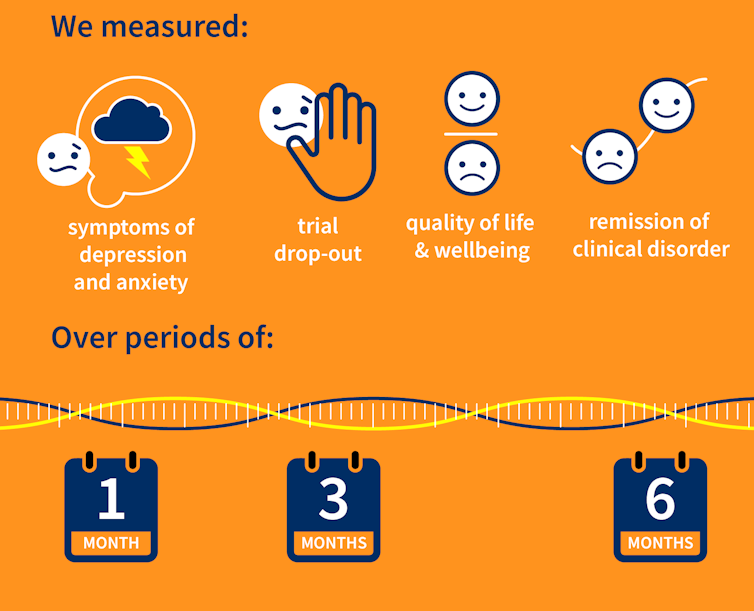
Our research team searched for randomised controlled trials published over the past 40 years that were designed to test the effectiveness of psychological therapies for depression among aged care residents 65 and over. We identified 19 trials from seven countries, including Australia, involving a total of 873 aged care residents with significant symptoms of depression.
The studies tested several different kinds of psychological therapies, which we classified as cognitive behavioural therapy (CBT), behaviour therapy or reminiscence therapy.
CBT involves teaching practical skills to help people re-frame negative thoughts and beliefs, while behaviour therapy aims to modify behaviour patterns by encouraging people with depression to engage in pleasurable and rewarding activities. Reminiscence therapy supports older people to reflect on positive or shared memories, and helps them find meaning in their life history.
The therapies were delivered by a range of professionals, including psychologists, social workers, occupational therapists and trainee therapists.
Cochrane AustraliaIn these studies, psychological therapies were compared to a control group where the older people did not receive psychological therapy. In most studies, this was “usual care” – the care typically provided to aged care residents, which may include access to antidepressants, scheduled activities and help with day-to-day tasks.
In some studies psychological therapy was compared to a situation where the older people received extra social contact, such as visits from a volunteer or joining in a discussion group.
What we found
Our results showed psychological therapies may be effective in reducing symptoms of depression for older people in residential aged care, compared with usual care, with effects lasting up to six months. While we didn’t see the same effect beyond six months, only two of the studies in our review followed people for this length of time, so the data was limited.
Our findings suggest these therapies may also improve quality of life and psychological wellbeing.
Psychological therapies mostly included between two and ten sessions, so the interventions were relatively brief. This is positive in terms of the potential feasibility of delivering psychological therapies at scale. The three different therapy types all appeared to be effective, compared to usual care.
However, we found psychological therapy may not be more effective than extra social contact in reducing symptoms of depression. Older people commonly feel bored, lonely and socially isolated in aged care. The activities on offer are often inadequate to meet their needs for stimulation and interest. So identifying ways to increase meaningful engagement day-to-day could improve the mental health and wellbeing of older people in aged care.
Some limitations
Many of the studies we found were of relatively poor quality, because of small sample sizes and potential risk of bias, for example. So we need more high-quality research to increase our confidence in the findings.
Many of the studies we reviewed were also old, and important gaps remain. For example, we are yet to understand the effectiveness of psychological therapies for people from diverse cultural or linguistic backgrounds.
Separately, we need better research to evaluate the effectiveness of antidepressants among aged care residents.
What needs to happen now?
Depression should not be considered a “normal” experience at this (or any other) stage of life, and those experiencing symptoms should have equal access to a range of effective treatments. The royal commission into aged care highlighted that Australians living in aged care don’t receive enough mental health support and called for this issue to be addressed.
While there have been some efforts to provide psychological services in residential aged care, the unmet need remains very high, and much more must be done.
The focus now needs to shift to how to implement psychological therapies in aged care, by increasing the competencies of the aged care workforce, training the next generation of psychologists to work in this setting, and funding these programs in a cost-effective way.
Tanya Davison, Adjunct professor, Health & Ageing Research Group, Swinburne University of Technology and Sunil Bhar, Professor of Clinical Psychology, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Black Pepper’s Impressive Anti-Cancer Arsenal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
Piperine, a compound found in Piper nigrum (black pepper, to its friends), has many health benefits. It’s included as a minor ingredient in some other supplements, because it boosts bioavailability. In its form as a kitchen spice, it’s definitely a superfood.
What does it do?
First, three things that generally go together:
These things often go together for the simple reason that oxidative stress, inflammation, and cancer often go together. In each case, it’s a matter of cellular wear-and-tear, and what can mitigate that.
For what it’s worth, there’s generally a fourth pillar: anti-aging. This is again for the same reason. That said, black pepper hasn’t (so far as we could find) been studied specifically for its anti-aging properties, so we can’t cite that here as an evidence-based claim.
Nevertheless, it’s a reasonable inference that something that fights oxidation, inflammation, and cancer, will often also slow aging.
Special note on the anti-cancer properties
We noticed two very interesting things while researching piperine’s anti-cancer properties. It’s not just that it reduces cancer risk and slows tumor growth in extant cancers (as we might expect from the above-discussed properties). Let’s spotlight some studies:
It is selectively cytotoxic (that’s a good thing)
Piperine was found to be selectively cytotoxic to cancerous cells, while not being cytotoxic to non-cancerous cells. To this end, it’s a very promising cancer-sniper:
Piperine as a Potential Anti-cancer Agent: A Review on Preclinical Studies
It can reverse multi-drug resistance in cancer cells
P-glycoprotein, found in our body, is a drug-transporter that is known for “washing out” chemotherapeutic drugs from cancer cells. To date, no drug has been approved to inhibit P-glycoprotein, but piperine has been found to do the job:
Targeting P-glycoprotein: Investigation of piperine analogs for overcoming drug resistance in cancer
What’s this about piperine analogs, though? Basically the researchers found a way to “tweak” piperine to make it even more effective. They called this tweaked version “Pip1”, because calling it by its chemical name,
((2E,4E)-5-(benzo[d][1,3]dioxol-5-yl)-1-(6,7-dimethoxy-3,4-dihydroisoquinolin-2(1 H)-yl)penta-2,4-dien-1-one)
…got a bit unwieldy.
The upshot is: Pip1 is better, but piperine itself is also good.
Other benefits
Piperine does have other benefits too, but the above is what we were most excited to talk about today. Its other benefits include:
- Neuroprotective effects (against Alzheimer’s, Parkinson’s, and more)
- Blood-sugar balancing / antidiabetic effect
- Good for gut microbiome diversity
- Heart health benefits, including cholesterol-balancing
- Boosts bioavailability of other nutrients/drugs
Enjoy!
Share This Post
-
Capsaicin For Weight Loss And Against Inflammation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Capsaicin’s Hot Benefits
Capsaicin, the compound in hot peppers that makes them spicy, is a chemical irritant and a neurotoxin. However, humans being humans, we decided to eat them for fun.
In contrast to many other ways in which humans recreationally enjoy things that are objectively poisonous, consuming capsaicin (in moderation) is considered to have health benefits, such as aiding weight loss (by boosting metabolism) and reducing inflammation.
Let’s see what the science says…
First: is it safe?
Capsaicin is classified as “Generally Recognized As Safe”. That said, the same mechanism that causes them to boost metabolism, does increase blood pressure:
Mechanisms underlying the hypertensive response induced by capsaicin
If you are in good cardiovascular health, this increase should be slight and not pose any threat, unless for example you enter a chili-eating contest when not acclimated to such:
Capsaicin and arterial hypertensive crisis
As ever, if unsure, do check with your doctor first, especially if you are taking any blood pressure medications, or otherwise have known blood pressure issues.
Does it really boost metabolism?
It certainly does; it works by increasing oxygen consumption and raising body temperature, both of which mean more calories will be burned for the same amount of work:
Dietary capsaicin and its anti-obesity potency: from mechanism to clinical implications
This means, of course, that chili peppers enjoy the status of being functionally a “negative calorie” food, and a top-tier one at that:
Chili pepper as a body weight-loss food
Here’s a good quality study that showed a statistically significant* fat loss improvement over placebo:
*To put it in numbers, the benefit was:
- 5.91 percentage points lower body fat percentage than placebo
- 6.68 percentage points greater change in body fat mass than placebo
See also: Difference between percentages and percentage points
For those who prefer big reviews than single studies, we’ve got you covered:
Does it really reduce inflammation?
Counterintuitive as it may seem, yes. By means of reducing oxidative stress. Given that things that reduce oxidative stress tend to reduce inflammation, and in turn tend to reduce assorted disease risks (from diabetes to cancer to Alzheimer’s), this probably has more knock-on benefits too, but we don’t have room to explore all of those today.
Fresh peppers are best for this, but dried peppers (such as when purchased as a ground spice in the supermarket, or when purchased as a capsule-based supplement) still have a very respectable anti-inflammatory effect:
- Capsaicinoids, Polyphenols and Antioxidant Activities of Capsicum annuum: Comparative Study of the Effect of Ripening Stage and Cooking Methods
- A Review on the Effect of Drying on Antioxidant Potential of Fruits and Vegetables
How much should we take?
It’s recommended to start at a low dose and gradually increase it, but 2–6mg of capsaicin per day is the standard range used in studies.
If you’re getting this from peppers, then for example cayenne pepper (a good source of capsaicin) contains around 2.5mg of capsaicin per 1 gram of cayenne.
In the case of capsules, if for example you don’t like eating hot pepper, this will usually mean taking 2–6 capsules per day, depending on dosage.
Make sure to take it with plenty of water!
Where can we get it?
Fresh peppers or ground spice from your local grocery store is fine. Your local health food store probably sells the supplements, too.
If you’d like to buy it online, here is an example product on Amazon.
Note: options on Amazon were more limited than usual, so this product is not vegan, and probably not halal or kosher, as the capsule contains an unspecified gelatin.
Share This Post
Related Posts
-
How To Rebuild Your Neurons’ Myelin Sheaths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PS: We Love You
Phosphatidylserine, or “PS” for short, is a phospholipid found in the brain. In other words, a kind of fatty compound that is such stuff as our brains are made of.
In particular, it’s required for healthy nerve cell membranes and myelin (the protective sheath that neurons live in—basically, myelin sheaths do for neurons what telomere caps do for DNA).
For an overview that’s more comprehensive than we have room for here, check out:
Phosphatidylserine and the human brain
Many people take it as a supplement.
Does taking it as a supplement work?
This is a valid question, as a lot of supplements can’t be absorbed well, and/or can’t pass the blood-brain barrier. But, as the above-linked study notes:
❝Exogenous PS (300-800 mg/d) is absorbed efficiently in humans, crosses the blood-brain barrier, and safely slows, halts, or reverses biochemical alterations and structural deterioration in nerve cells. It supports human cognitive functions, including the formation of short-term memory, the consolidation of long-term memory, the ability to create new memories, the ability to retrieve memories, the ability to learn and recall information, the ability to focus attention and concentrate, the ability to reason and solve problems, language skills, and the ability to communicate. It also supports locomotor functions, especially rapid reactions and reflexes.❞
(“Exogenous” means “coming from outside of the body”, as opposed to “endogenous”, meaning “made inside the body”. Effectively, in this context “exogenous” means “taken as a supplement”.)
Why do people take it?
The health claims for phosphatidylserine fall into two main categories:
- Neuroprotection (helping your brain to avoid age-related decline in the long term)
- Cognitive enhancement (helping your brain work better in the short term)
What does the science say?
There’s a lot of science that’s been done on the neuroprotective properties of PS, and there are thousands of studies we could draw from here. The upshot is that regular phosphatidylserine supplementation (most often 300mg/day, but studies are also found for 100–500mg/day) is strongly associated with a reduction in cognitive decline over the course of 12 weeks (a common study duration). Here are a some spotlight studies showing this:
- Effects of phosphatidylserine in Alzheimer’s disease
- Double-blind cross-over study of phosphatidylserine vs. placebo in patients with early dementia of the Alzheimer type
- Effect of Phosphatidylserine on Cerebral Glucose Metabolism in Alzheimer’s Disease
- The effect of soybean-derived phosphatidylserine on cognitive performance in elderly with subjective memory complaints
Note: PS can be derived from various sources, with the two most common forms being bovine (i.e., from cow brains) or soy-derived.
There is no established difference in the efficacy of these.
There have been some concerns raised about the risk of CJD (the human form of BSE, as in “mad cow disease”) from consuming brain matter from cows, but studies have not found any evidence of this actually happening.
There is also some evidence that phosphatidyserine significantly boosts cognitive performance, even in young people with no extant cognitive decline, for example:
(as the title suggests, they did also test for its effect on mood and endocrine response, but found it made no difference to those, just the cognitive function—which enjoyed a boost before exercise, as well as after it, meaning that the boost wasn’t dependent on the exercise)
PS for cognitive enhancement in the young and healthy is not nearly so well-explored as its use as a later-life guard against age-related cognitive decline. However, just because the studies in younger people are dwarfed in number by the studies in older people, doesn’t detract from the validity of the studies in younger people.
Basically: its use in older people has been studied the most, but all available evidence points to it being beneficial to brain health at all ages.
Where can we get it?
We don’t sell it (or anything else), but for your convenience, here’s an example product on Amazon.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I can’t afford olive oil. What else can I use?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you buy your olive oil in bulk, you’ve likely been in for a shock in recent weeks. Major supermarkets have been selling olive oil for up to A$65 for a four-litre tin, and up to $26 for a 750 millilitre bottle.
We’ve been hearing about the health benefits of olive oil for years. And many of us are adding it to salads, or baking and frying with it.
But during a cost-of-living crisis, these high prices can put olive oil out of reach.
Let’s take a look at why olive oil is in demand, why it’s so expensive right now, and what to do until prices come down.
Joyisjoyful/Shutterstock Remind me, why is olive oil so good for you?
Including olive oil in your diet can reduce your risk of developing type 2 diabetes and improve heart health through more favourable blood pressure, inflammation and cholesterol levels.
This is largely because olive oil is high in monounsaturated fatty acids and polyphenols (antioxidants).
Some researchers have suggested you can get these benefits from consuming up to 20 grams a day. That’s equivalent to about five teaspoons of olive oil.
Why is olive oil so expensive right now?
A European heatwave and drought have limited Spanish and Italian producers’ ability to supply olive oil to international markets, including Australia.
This has been coupled with an unusually cold and short growing season for Australian olive oil suppliers.
The lower-than-usual production and supply of olive oil, together with heightened demand from shoppers, means prices have gone up.
We’ve seen unfavourable growing conditions in Europe and Australia. KaMay/Shutterstock How can I make my olive oil go further?
Many households buy olive oil in large quantities because it is cheaper per litre. So, if you have some still in stock, you can make it go further by:
- storing it correctly – make sure the lid is on tightly and it’s kept in a cool, dark place, such as a pantry or cabinet. If stored this way, olive oil can typically last 12–18 months
- using a spray – sprays distribute oil more evenly than pourers, using less olive oil overall. You could buy a spray bottle to fill from a large tin, as needed
- straining or freezing it – if you have leftover olive oil after frying, strain it and reuse it for other fried dishes. You could also freeze this used oil in an airtight container, then thaw and fry with it later, without affecting the oil’s taste and other characteristics. But for dressings, only use fresh oil.
I’ve run out of olive oil. What else can I use?
Here are some healthy and cheaper alternatives to olive oil:
- canola oil is a good alternative for frying. It’s relatively low in saturated fat so is generally considered healthy. Like olive oil, it is high in healthy monounsaturated fats. Cost? Up to $6 for a 750mL bottle (home brand is about half the price)
- sunflower oil is a great alternative to use on salads or for frying. It has a mild flavour that does not overwhelm other ingredients. Some studies suggest using sunflower oil may help reduce your risk of heart disease by lowering LDL (bad) cholesterol and raising HDL (good) cholesterol. Cost? Up to $6.50 for a 750mL bottle (again, home brand is about half the price)
- sesame oil has a nutty flavour. It’s good for Asian dressings, and frying. Light sesame oil is typically used as a neutral cooking oil, while the toasted type is used to flavour sauces. Sesame oil is high in antioxidants and has some anti-inflammatory properties. Sesame oil is generally sold in smaller bottles than canola or sunflower oil. Cost? Up to $5 for a 150mL bottle.
There are plenty of alternative oils you can use in salads or for frying. narai chal/Shutterstock How can I use less oil, generally?
Using less oil in your cooking could keep your meals healthy. Here are some alternatives and cooking techniques:
- use alternatives for baking – unless you are making an olive oil cake, if your recipe calls for a large quantity of oil, try using an alternative such as apple sauce, Greek yoghurt or mashed banana
- use non-stick cookware – using high-quality, non-stick pots and pans reduces the need for oil when cooking, or means you don’t need oil at all
- steam instead – steam vegetables, fish and poultry to retain nutrients and moisture without adding oil
- bake or roast – potatoes, vegetables or chicken can be baked or roasted rather than fried. You can still achieve crispy textures without needing excessive oil
- grill – the natural fats in meat and vegetables can help keep ingredients moist, without using oil
- use stock – instead of sautéing vegetables in oil, try using vegetable broth or stock to add flavour
- try vinegar or citrus – use vinegar or citrus juice (such as lemon or lime) to add flavour to salads, marinades and sauces without relying on oil
- use natural moisture – use the natural moisture in ingredients such as tomatoes, onions and mushrooms to cook dishes without adding extra oil. They release moisture as they cook, helping to prevent sticking.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Shame and blame can create barriers to vaccination
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Understanding the stigma surrounding infectious diseases like HIV and mpox may help community health workers break down barriers that hinder access to care.
Looking back in history can provide valuable lessons to confront stigma in health care today, especially toward Black, Latine, LGBTQ+, and other historically underserved communities disproportionately affected by COVID-19 and HIV.
Public Good News spoke with Sam Brown, HIV prevention and wellness program manager at Civic Heart, a community-based organization in Houston’s historic Third Ward, to understand the effects of stigma around sexual health and vaccine uptake.
Brown shared more about Civic Heart’s efforts to provide free confidential testing for sexually transmitted infections, counseling and referrals, and information about COVID-19, flu, and mpox vaccinations, as well as the lessons they’re learning as they strive for vaccine equity.
Here’s what Brown said.
[Editor’s note: This content has been edited for clarity and length.]
PGN: Some people on social media have spread the myth that vaccines cause AIDS or other immune deficiencies when the opposite is true: Vaccines strengthen our immune systems to help protect against disease. Despite being frequently debunked, how do false claims like these impact the communities you serve?
Sam Brown: Misinformation like that is so hard to combat. And it makes the work and the path to overall community health hard because people will believe it. In the work that we do, 80 percent of it is changing people’s perspective on something they thought they knew.
You know, people don’t even transmit AIDS. People transmit HIV. So, a vaccine causing immunodeficiency doesn’t make sense.
With the communities we serve, we might have a person that will believe the myth, and because they believe it, they won’t get vaccinated. Then later, they may test positive for COVID-19.
And depending on social determinants of health, it can impact them in a whole heap of ways: That person is now missing work, they’re not able to provide for their family—if they have a family. It’s this mindset that can impact a person’s life, their income, their ability to function.
So, to not take advantage of something like a vaccine that’s affordable, or free for the most part, just because of misinformation or a misunderstanding—that’s detrimental, you know.
For example, when we talk to people in the community, many don’t know that they can get mpox from their pet, or that it’s zoonotic—that means that it can be transferred between different species or different beings, from animals to people. I see a lot of surprise and shock [when people learn this].
It’s difficult because we have to fight the misinformation and the stigma that comes with it. And it can be a big barrier.
People misunderstand. [They] think that “this is something that gay people or the LGBTQ+ community get,” which is stigmatizing and comes off as blaming. And blaming is the thing that leads us to be misinformed.
PGN: In the last couple years, your organization’s HIV Wellness program has taken on promoting COVID-19, flu, and mpox vaccines to the communities you serve. How do you navigate conversations between sexual health and infectious diseases? Can you share more about your messaging strategies?
S.B.: As we promoted positive sexual health and HIV prevention, we saw people were tired of hearing about HIV. They were tired of hearing about how PrEP works, or how to prevent HIV.
But, when we had an outbreak of syphilis in Houston just last year, people were more inclined to test because of the severity of the outbreak.
So, what our team learned is that sometimes you have to change the message to get people what they need.
We changed our message to highlight more syphilis information and saw that we were able to get more people tested for HIV because we correlated how syphilis and HIV are connected and how a person can be susceptible to both.
Using messages that the community wants and pairing them with what the community needs has been better for us. And we see that same thing with COVID-19, the flu, and RSV. Sometimes you just can’t be married to a message. We’ve had to be flexible to meet our clients where they are to help them move from unsafe practices to practices that are healthy and good for them and their communities.
PGN: You’ve mentioned how hard it is to combat stigma in your work. How do you effectively address it when talking to people one-on-one?
S.B.: What I understand is that no one wants to feel shame. What I see people respond to is, “Here’s an opportunity to do something different. Maybe there was information that you didn’t know that caused you to make a bad decision. And now here’s an opportunity to gain information so that you can make a better decision.”
People want to do what they want to do; they want to live how they want to live. And we all should be able to do that as long as it’s not hurting anyone, but also being responsible enough to understand that, you know, COVID-19 is here.
So, instead of shaming and blaming, it’s best to make yourself aware and understand what it is and how to treat it. Because the real enemy is the virus—it’s the infection, not the people.
When we do our work, we want to make sure that we come from a strengths-based approach. We always look at what a client can do, what that client has. We want to make sure that we’re empowering them from that point. So, even if they choose not to prioritize our message right now, we can’t take that personally. We’ll just use it as a chance to try a new way of framing it to help people understand what we’re trying to say.
And sometimes that can be difficult, even for organizations. But getting past that difficulty comes with a greater opportunity to impact someone else.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: