Common Hospital Blood Pressure Mistake (Don’t Let This Happen To You Or A Loved One)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a major issue in healthcare, Dr. Suneel Dhand tells us, pertaining to the overtreatment of hypertension in hospitals. Here’s how to watch out for it and know when to question it:
Under pressure
When patients, particularly from older generations, are admitted to the hospital, their blood pressure often fluctuates due to illness, dehydration, and other factors. Despite this, they are often continued on their usual blood pressure medications, which can lead to dangerously low blood pressure.
Why does this happen? The problem arises from rigid protocols that dictate stopping blood pressure medication only if systolic pressure is below a certain threshold, often 100. However, Dr. Dhand argues that 100 is already low*, and administering medication when blood pressure is close to this can cause it to drop dangerously lower
*10almonds note: low for an adult, anyway, and especially for an older adult. To be clear: it’s not a bad thing! That is the average systolic blood pressure of a healthy teenager and it’s usually the opposite of a problem if we have that when older (indeed, this very healthy writer’s blood pressure averages 100/70, and suffice it to say, it’s been a long time since I was a teenager). But it does mean that we definitely don’t want to take medications to artificially lower it from there.
Low blood pressure from overtreatment can lead to severe consequences, requiring emergency interventions to stabilize the patient.
Dr. Dhand’s advice for patients and families is:
- Ensure medication accuracy: make sure the medical team knows the correct blood pressure medications and dosages for you or your loved one.
- Monitor vital signs: actively check blood pressure readings, especially if they are in the low 100s or even 110s, and discuss any medication concerns with the medical team.
- Watch for symptoms of low blood pressure: be alert for symptoms like dizziness or weakness, which could indicate dangerously low blood pressure.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Insider’s Guide To Making Hospital As Comfortable As Possible
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lychees vs Kumquats – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing lychees to kumquats, we picked the kumquats.
Why?
In terms of macros, everything is comparable except for fiber, of which kumquats have 5–6x as much fiber, which means a very significant win for kumquats in this category.
When it comes to vitamins, lychees have slightly more of vitamins B3, B6, C, and K, while kumquats have a lot more of vitamins A and B1, and moderately more vitamins B2, B9, E, and choline. A fair win for kumquats here.
In the category of minerals, lychees have a little more copper, phosphorus, and selenium, while kumquats have 11x as much calcium, as well as a 2–3x more iron, magnesium, manganese and zinc. An easy win for kumquats.
Both fruits have great phenolic profiles, being both rich in antioxidants.
All in all, enjoy both, but if you’re going to pick one, kumquats easily win the day!
Want to learn more?
You might like to read:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- When Bitter Is Better: Enjoy Bitter Foods For Your Heart & Brain ← kumquats have a bitter citrus taste, while lychees are quite sweet and mellow
Take care!
Share This Post
-
Strong At Every Age: 15 Habits To Level Up Your Health & Fitness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not every increase in health and fitness needs to look like a training montage from the “Rocky” movies!
Making progress every day
We’ll not keep the 15 habits a secret; they are:
- Follow the one-minute rule: commit to just one minute of action—this makes starting easier, and often you’ll end up doing more once you’ve got started.
- Make the habit exciting: add fun elements to make the habit more enjoyable, like using new gear or accessories.
- Do it first: prioritize new habits by doing them early in the day to ensure they get done.
- Share the love: pair new habits with activities you already enjoy, where practical, to do “temptation bundling”.
- Embrace the uncomfortable: get used to discomfort daily to grow and build resilience for bigger changes.
- Do as little as possible: start small with habits, to minimize resistance and focus on consistency.
- Think how to be lazy: simplify processes and use shortcuts; there are no extra prizes for it having been difficult!
- Make the appointment: schedule habits with set dates and times, to increase accountability.
- Let habits evolve: adapt habits to fit current circumstances; that way you can still stay consistent over time.
- Plan ahead: prepare in advance to avoid setbacks—what could stop you from succeeding, and how can you pre-empt that?
- Pause to reflect: regularly evaluate what works and what doesn’t, to adjust and improve.
- Shut off your brain: avoid overthinking and start taking action now, not later, to build momentum.
- Question and learn: stay curious and open to learning, or else you will plateau quickly!
- Ask why: understand the deeper reasons behind any resistance, and make clear for yourself the value of the habit.
- Love your failures: embrace any setbacks as learning opportunities and, as such, stepping stones to success.
For more on all of each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Share This Post
-
5 Steps To Quit Sugar Easily
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sugar is one of the least healthy things that most people consume, yet because it’s so prevalent, it can also be tricky to avoid at first, and the cravings can also be a challenge. So, how to quit it?
Step by step
Dr. Mike Hansen recommends the following steps:
- Be aware: a lot of sugar consumption is without realizing it or thinking about it, because of how common it is for there to be added sugar in things we might purchase ready-made, even supposedly healthy things like yogurts, or easy-to-disregard things like condiments.
- Recognize sugar addiction: a controversial topic, but Dr. Hansen comes down squarely on the side of “yes, it’s an addiction”. He wants us to understand more about the mechanics of how this happens, and what it does to us.
- Reduce gradually: instead of going “cold turkey”, he recommends we avoid withdrawal symptoms by first cutting back on liquid sugars like sodas, juices, and syrups, before eliminating solid sugar-heavy things like candy, sugar cookies, etc, and finally the more insidious “why did they put sugar in this?” added-sugar products.
- Find healthy alternatives: simple like-for-like substitutions; whole fruits instead of juices/smoothies, for example. 10almonds tip: stuffing dates with an almond each makes it very much like eating chocolate, experientially!
- Manage cravings: Dr. Hansen recommends distraction, and focusing on upping other healthy habits such as hydration, exercise, and getting more vegetables.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Which Sugars Are Healthier, And Which Are Just The Same?
- Mythbusting The Not-So-Sweet Science Of Sugar Addiction
Take care!
Share This Post
Related Posts
-
Signs Of Low Estrogen In Women: What Your Skin, Hair, & Nails Are Trying To Tell You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Skin, hair, and nails are often thought of purely as a beauty thing, but in fact they can be indicative of a lot of other aspects of health. Dr. Andrea Suarez takes us through some of them in this video about the systemic (i.e., whole-body, not just related to sex things) effects of estrogen, and/or a deficiency thereof.
Beyond the cosmetic
Low estrogen levels are usual in women during and after untreated menopause, resulting in various changes in the skin, hair, and nails, that reflect deeper issues, down to bone health, heart health, brain health, and more. Since we can’t see our bones or hearts or brains without scans (or a serious accident/incident), we’re going to focus on the outward signs of estrogen deficiency.
Estrogen helps maintain healthy collagen production, skin elasticity, wound healing, and moisture retention, making it essential for youthful and resilient skin. Declining estrogen levels with menopause lead to a thinner epidermis, decreased collagen production, and more pronounced wrinkles. Skin elasticity also diminishes, which slows the skin’s ability to recover from stretching or deformation. Wound healing also becomes slower, increasing the risk of infections and extended recovery periods after injuries or surgeries—bearing in mind that collagen is needed in everything from our skin to our internal connective tissue (fascia) and joints and bones. So all those things are going to struggle to recover from injury (and surgery is also an injury) without it.
Other visible changes associated with declining estrogen include significant dryness as a result of reduced hyaluronic acid and glycosaminoglycan production, which are essential for moisture retention. The skin becomes more prone to irritation and increased water loss. Additionally, estrogen deficiency results in less resistance to oxidative stress, making the skin more susceptible to damage from environmental factors such as UV radiation and pollution, as well as any from-the-inside pollution that some may have depending on diet and lifestyle.
Acne and enlarged pores are associated with increased testosterone, but testosterone and estrogen are antagonistic in most ways, and in this case a decrease in estrogen will do the same, due increased unopposed androgen signaling affecting the oil glands. The loss of supportive collagen also causes the skin around pores to lose structure, making them appear larger. The reduction in skin hydration further exacerbates the visibility of pores and can contribute to the development of blackheads due to abnormal cell turnover.
Blood vessel issues tend to arise as estrogen levels drop, leading to a reduction in angiogenesis, i.e. the formation and integrity of blood vessels. This results in more fragile and leaky blood vessels, making the skin more prone to bruising, especially on areas frequently exposed to the sun, such as the backs of the hands. This weakened vasculature also further contributes to the slower wound healing that we talked about, due to less efficient delivery of growth factors.
Hair and nail changes often accompany estrogen deficiency. Women may notice hair thinning, increased breakage, and a greater likelihood of androgenic alopecia. The texture of the hair can change, becoming more brittle. Similarly, nails can develop ridges, split more easily, and become more fragile due to reduced collagen and keratin production, which also affects the skin around the nails.
As for what to do about it? Management options for estrogen-deficient skin include:
- Bioidentical hormone replacement therapy (HRT), which can improve skin elasticity, boost collagen production, and reduce dryness and fragility, as well as addressing the many more serious internal things that are caused by the same deficiency as these outward signs.
- Low-dose topical estrogen cream, which can help alleviate skin dryness and increase skin strength, won’t give the systemic benefits (incl. to bones, heart, brain, etc) that only systemic HRT can yield.
- Plant-based phytoestrogens, which are not well-evidenced, but may be better than nothing if nothing is your only other option. However, if you are taking anything other form of estrogen, don’t use phytoestrogens as well, or they will compete for estrogen receptors, and do the job not nearly so well while impeding the bioidentical estrogen from doing its much better job.
And for all at any age, sunscreen continues to be one of the best things to put on one’s skin for general skin health, and this is even more true if running low on estrogen.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
These Signs Often Mean These Nutrient Deficiencies (Do You Have Any?)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
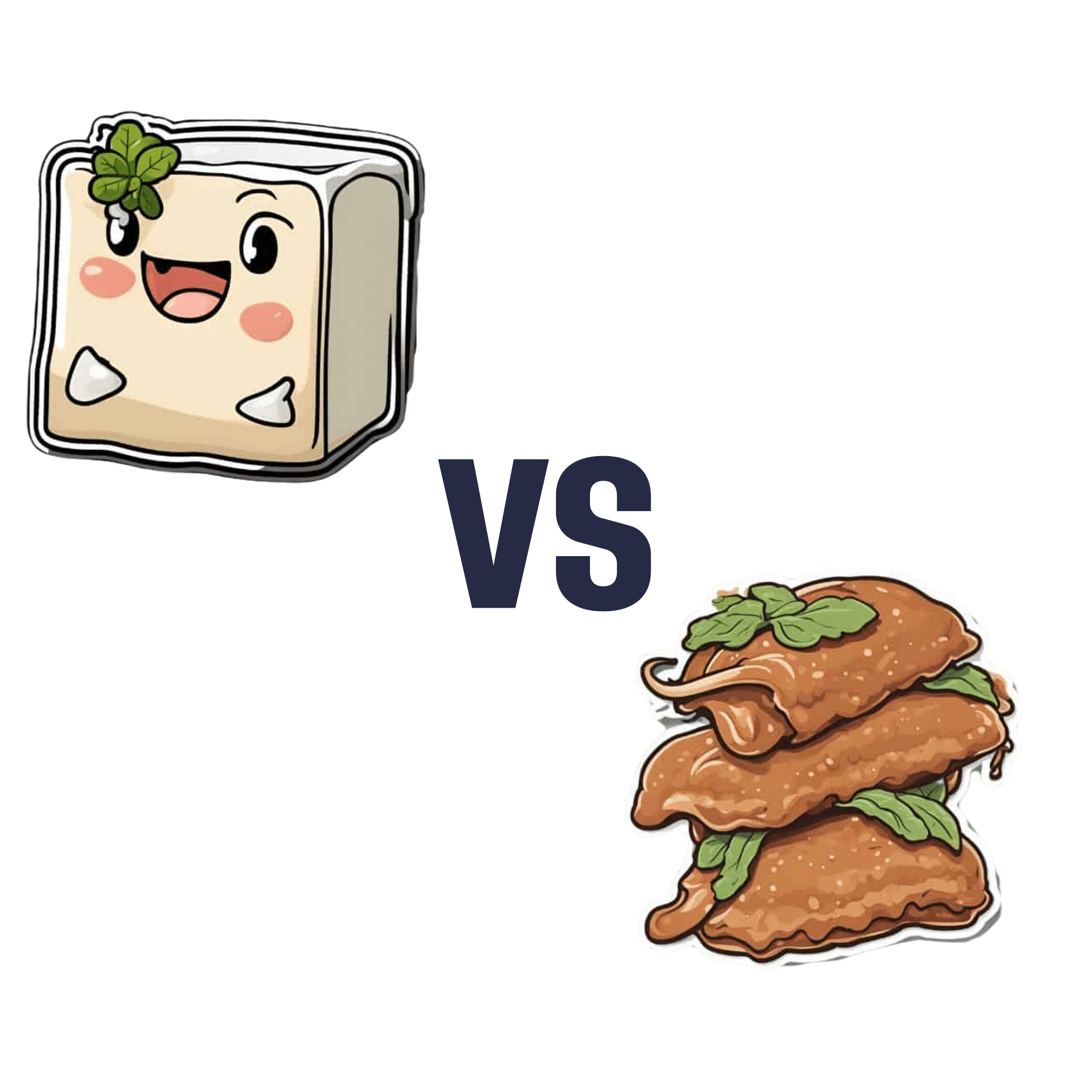
Tofu vs Seitan – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tofu to seitan, we picked the tofu.
Why?
This one is not close!
In terms of macros, seitan does have about 2x the protein, but it also has 6x the carbs and 6x the sodium of tofu, as well as less fiber than tofu.. So we’ll call it a tie on macros. But…
Seitan is also much more processed than tofu, as tofu has usually just been fermented and possibly pressed (depending on kind). Seitan, in contrast, is processed gluten that has been extracted from wheat and usually had lots of things happen to it on the way (depending on kind).
About that protein… Tofu is a complete protein, meaning it has all of the essential amino acids. Seitain, meanwhile, is lacking in lysine.
When it comes to vitamins and minerals, again tofu easily comes out on top; tofu has 5x the calcium, similar iron, more magnesium, 2x the phosphorous, 150% of the potassium, and contains several other nutrients that seitan doesn’t, such as folate and choline.
So, easy winning for tofu across the board on micronutrients.
Tofu is also rich in isoflavones, antioxidant phytonutrients, while seitan has no such benefits.
So, another win for tofu.
There are two reasons you might choose seitan:
- prioritizing bulk protein above all other health considerations
- you are allergic to soy and not allergic to gluten
If neither of those things are the case, then tofu is the healthier choice!
Want to learn more?
You might like to read:
- Tempeh vs Tofu – Which is Healthier? ← tempeh is, nutritionally speaking, tofu but better. Of course on a culinary level, there are many recipes where tofu will work and tempeh wouldn’t, though.
- Gluten: What’s The Truth?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tell Yourself a Better Lie – by Marissa Peer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As humans, we generally lie to ourselves constantly. Or perhaps we really believe some of the things we tell ourselves, even if they’re not objectively necessarily true:
- I’ll always be poor
- I’m destined to be alone
- I don’t deserve good things
- Etc.
Superficially, it’s easy to flip those, and choose to tell oneself the opposite. But it feels hollow and fake, doesn’t it? That’s where Marissa Peer comes in.
Our stories that we tell ourselves don’t start where we are—they’re generally informed by things we learned along the way. Sometimes good lessons, sometimes bad ones. Sometimes things that were absolutely wrong and/or counterproductive.
Peer invites the reader to ask “What if…”, unravel how the unhelpful lessons got wired into our brains in the first place, and then set about untangling them.
“Tell yourself a better lie” does not mean self-deceit. It means that we’re the authors of our own stories, so we might as well make them work for us. Many things in life are genuinely fixed; others are open to interpretation.
Sorting one from the other, and then treating them correctly in a way that’s helpful to us? That’s how we can stop hurting ourselves, and instead bring our own stories around to uplift and fortify us.
Get Your Copy of “Tell Yourself A Better Lie” on Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: