Coffee & Your Gut
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Coffee, in moderation, is generally considered a healthful drink—speaking for the drink itself, at least! Because the same cannot be said for added sugar, various sorts of creamers, or iced caramelatte mocha frappucino dessert-style drinks:
The Bitter Truth About Coffee (or is it?)
Caffeine, too, broadly has more pros than cons (again, in moderation):
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
Some people will be concerned about coffee and the heart. Assuming you don’t have a caffeine sensitivity (or you do but you drink decaf), it is heart-neutral in moderation, though there are some ways of preparing it that are better than others:
Make Your Coffee Heart-Healthier!
So, what about coffee and the gut?
The bacteria who enjoy a good coffee
Amongst our trillions of tiny friends, allies, associates, and enemies-on-the-inside, which ones like coffee, and what kind of coffee do they prefer?
A big (n=35,214) international multicohort analysis examined the associations between coffee consumption and very many different gut microbial species, and found:
115 species were positively associated with coffee consumption, mostly of the kind considered “friendly”, including ones often included in probiotic supplements, such as various Bifidobacterium and Lactobacillus species.
The kind that was most strongly associated with coffee consumption, however, was Lawsonibacter asaccharolyticus, a helpful little beast who converts chlorogenic acid (one of the main polyphenols in coffee) into caffeic acid, quinic acid, and various other metabolites that we can use.
More specifically: moderate coffee-drinkers, defined as drinking 1–3 cups per day, enjoyed a 300–400% increase in L. asaccharolyticus, while high coffee-drinkers (no, not that kind of high), defined as drinking 4 or more cups of coffee per day, enjoyed a 400–800% increase, compared to “never/rarely” coffee-drinkers (defined as drinking 2 or fewer cups per month).
Click here to see more data from the study, in a helpful infographic
Things that did not affect the outcome:
- The coffee-making method—it seems the bacteria are not fussy in this regard, as espresso or brewed, and even instant, yielded the same gut microbiome benefits
- The caffeine content—as both caffeinated and decaffeinated yielded the same gut microbiome benefits
You can read the paper itself in full for here:
Want to enjoy coffee, but not keen on the effects of caffeine or the taste of decaffeinated?
Taking l-theanine alongside coffee flattens the curve of caffeine metabolism, and means one can get the benefits without unwanted jitteriness:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hormone Replacement
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I cant believe 10 Almonds addresses questions. Thanks. I see the word symptoms for menopause. I don’t know what word should replace it but maybe one should be used or is symptom accurate? And I recently read that there was a great disservice for women in my era as they were denied/scared of hormones replacement. Unnecessarily❞
You’d better believe it! In fact we love questions; they give us things to research and write about.
“Symptom” is indeed an entirely justified word to use, being:
- General: any phenomenon or circumstance accompanying something and serving as evidence of it.
- Medical: any phenomenon that arises from and accompanies a particular disease or disorder and serves as an indication of it.
If the question is more whether the menopause can be considered a disease/disorder, well, it’s a naturally occurring and ultimately inevitable change, yes, but then, so is cancer (it’s in the simple mathematics of DNA replication and mutation that, unless a cure for cancer is found, we will always eventually get cancer, if nothing else kills us first).
So, something being natural/inevitable isn’t a reason to not consider it a disease/disorder, nor a reason to not treat it as appropriate if it is causing us harm/discomfort that can be safely alleviated.
Moreover, and semantics aside, it is medical convention to consider menopause to be a medical condition, that has symptoms. Indeed, for example, the US’s NIH (and its constituent NIA, the National Institute of Aging) and the UK’s NHS, both list the menopause’s symptoms, using that word:
- NIA (NIH): What are the signs and symptoms of menopause?
- NHS: Common symptoms of menopause and perimenopause
With regard to fearmongering around HRT, certainly that has been rife, and there were some very flawed (and later soundly refuted) studies a while back that prompted this—and even those flawed studies were not about the same (bioidentical) hormones available today, in any case. So even if they had been correct (they weren’t), it still wouldn’t be a reason to not get treatment nowadays, if appropriate!
Share This Post
-
California Becomes Latest State To Try Capping Health Care Spending
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
California’s Office of Health Care Affordability faces a herculean task in its plan to slow runaway health care spending.
The goal of the agency, established in 2022, is to make care more affordable and accessible while improving health outcomes, especially for the most disadvantaged state residents. That will require a sustained wrestling match with a sprawling, often dysfunctional health system and powerful industry players who have lots of experience fighting one another and the state.
Can the new agency get insurers, hospitals, and medical groups to collaborate on containing costs even as they jockey for position in the state’s $405 billion health care economy? Can the system be transformed so that financial rewards are tied more to providing quality care than to charging, often exorbitantly, for a seemingly limitless number of services and procedures?
The jury is out, and it could be for many years.
California is the ninth state — after Connecticut, Delaware, Massachusetts, Nevada, New Jersey, Oregon, Rhode Island, and Washington — to set annual health spending targets.
Massachusetts, which started annual spending targets in 2013, was the first state to do so. It’s the only one old enough to have a substantial pre-pandemic track record, and its results are mixed: The annual health spending increases were below the target in three of the first five years and dropped beneath the national average. But more recently, health spending has greatly increased.
In 2022, growth in health care expenditures exceeded Massachusetts’ target by a wide margin. The Health Policy Commission, the state agency established to oversee the spending control efforts, warned that “there are many alarming trends which, if unaddressed, will result in a health care system that is unaffordable.”
Neighboring Rhode Island, despite a preexisting policy of limiting hospital price increases, exceeded its overall health care spending growth target in 2019, the year it took effect. In 2020 and 2021, spending was largely skewed by the pandemic. In 2022, the spending increase came in at half the state’s target rate. Connecticut and Delaware, by contrast, both overshot their 2022 targets.
It’s all a work in progress, and California’s agency will, to some extent, be playing it by ear in the face of state policies and demographic realities that require more spending on health care.
And it will inevitably face pushback from the industry as it confronts unreasonably high prices, unnecessary medical treatments, overuse of high-cost care, administrative waste, and the inflationary concentration of a growing number of hospitals in a small number of hands.
“If you’re telling an industry we need to slow down spending growth, you’re telling them we need to slow down your revenue growth,” says Michael Bailit, president of Bailit Health, a Massachusetts-based consulting group, who has consulted for various states, including California. “And maybe that’s going to be heard as ‘we have to restrain your margins.’ These are very difficult conversations.”
Some of California’s most significant health care sectors have voiced disagreement with the fledgling affordability agency, even as they avoid overtly opposing its goals.
In April, when the affordability office was considering an annual per capita spending growth target of 3%, the California Hospital Association sent it a letter saying hospitals “stand ready to work with” the agency. But the proposed number was far too low, the association argued, because it failed to account for California’s aging population, new investments in Medi-Cal, and other cost pressures.
The hospital group suggested a spending increase target averaging 5.3% over five years, 2025-29. That’s slightly higher than the 5.2% average annual increase in per capita health spending over the five years from 2015 to 2020.
Five days after the hospital association sent its letter, the affordability board approved a slightly less aggressive target that starts at 3.5% in 2025 and drops to 3% by 2029. Carmela Coyle, the association’s chief executive, said in a statement that the board’s decision still failed to account for an aging population, the growing need for mental health and addiction treatment, and a labor shortage.
The California Medical Association, which represents the state’s doctors, expressed similar concerns. The new phased-in target, it said, was “less unreasonable” than the original plan, but the group would “continue to advocate against an artificially low spending target that will have real-life negative impacts on patient access and quality of care.”
But let’s give the state some credit here. The mission on which it is embarking is very ambitious, and it’s hard to argue with the motivation behind it: to interject some financial reason and provide relief for millions of Californians who forgo needed medical care or nix other important household expenses to afford it.
Sushmita Morris, a 38-year-old Pasadena resident, was shocked by a bill she received for an outpatient procedure last July at the University of Southern California’s Keck Hospital, following a miscarriage. The procedure lasted all of 30 minutes, Morris says, and when she received a bill from the doctor for slightly over $700, she paid it. But then a bill from the hospital arrived, totaling nearly $9,000, and her share was over $4,600.
Morris called the Keck billing office multiple times asking for an itemization of the charges but got nowhere. “I got a robotic answer, ‘You have a high-deductible plan,’” she says. “But I should still receive a bill within reason for what was done.” She has refused to pay that bill and expects to hear soon from a collection agency.
The road to more affordable health care will be long and chock-full of big challenges and unforeseen events that could alter the landscape and require considerable flexibility.
Some flexibility is built in. For one thing, the state cap on spending increases may not apply to health care institutions, industry segments, or geographic regions that can show their circumstances justify higher spending — for example, older, sicker patients or sharp increases in the cost of labor.
For those that exceed the limit without such justification, the first step will be a performance improvement plan. If that doesn’t work, at some point — yet to be determined — the affordability office can levy financial penalties up to the full amount by which an organization exceeds the target. But that is unlikely to happen until at least 2030, given the time lag of data collection, followed by conversations with those who exceed the target, and potential improvement plans.
In California, officials, consumer advocates, and health care experts say engagement among all the players, informed by robust and institution-specific data on cost trends, will yield greater transparency and, ultimately, accountability.
Richard Kronick, a public health professor at the University of California-San Diego and a member of the affordability board, notes there is scant public data about cost trends at specific health care institutions. However, “we will know that in the future,” he says, “and I think that knowing it and having that information in the public will put some pressure on those organizations.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
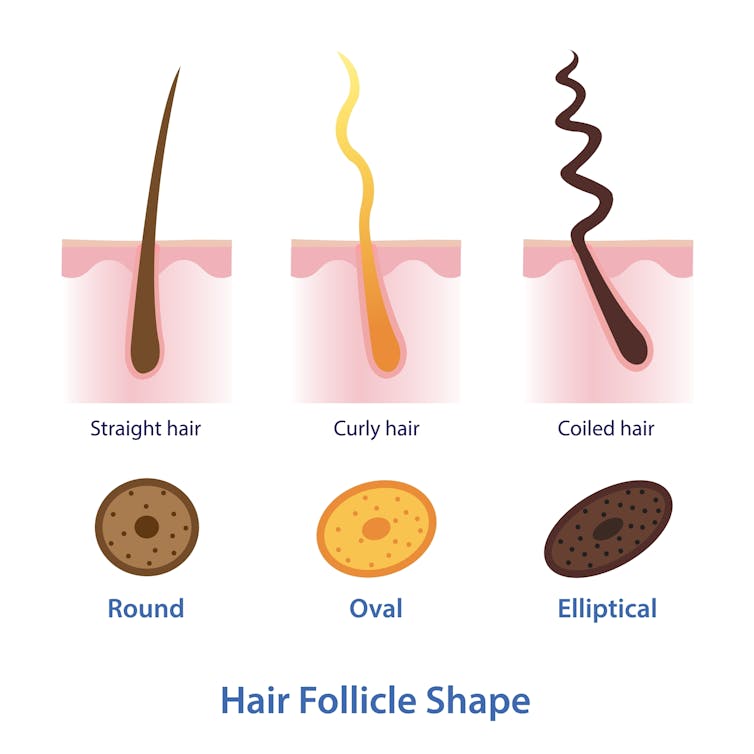
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.
Each hair strand grows from its own hair follicle.
Mosterpiece/ShutterstockLife changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.
Each hair on the scalp is replaced every three to five years.
Just Life/ShutterstockHormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.
Your hair can change at different stages of your life.
Igor Ivakhno/ShutterstockHormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
No, COVID-19 vaccines don’t cause ‘turbo cancer’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- COVID-19 vaccines do not cause “turbo cancer” or contain SV40, a virus that has been suspected of causing cancer.
- There is no link between rising cancer rates and COVID-19 vaccines.
- Staying up to date on COVID-19 vaccines is a safe, free way to support long-term health.
Myths that COVID-19 vaccines cause cancer have been circulating since the vaccines were first developed. These false claims resurfaced last month after Princess Kate Middleton announced that she is undergoing cancer treatment, with some vaccine opponents falsely claiming Middleton has a “turbo cancer” caused by COVID-19 vaccines.
Here’s what we know: “Turbo cancer” is a made-up term for a fake phenomenon, and there is strong evidence that COVID-19 vaccines do not cause cancer or increase cancer risk.
Read on to learn how to recognize false claims about COVID-19 vaccines and cancer.
Do COVID-19 vaccines contain cancer-causing ingredients?
No. Some vaccine opponents claim that COVID-19 vaccines contain SV40, a virus that has been suspected of causing cancer. This claim is false.
A piece of SV40’s DNA sequence—called a “promoter”—was used as starting material to develop COVID-19 vaccines, but the virus itself is not present in the vaccines. The promoter does not contain the part of the virus that enters the cell nucleus, so it poses no risk.
COVID-19 vaccines and their ingredients have been rigorously studied in millions of people worldwide and have been determined to be safe. The National Cancer Institute and the American Cancer Society agree that COVID-19 vaccines do not increase cancer risk or accelerate cancer growth.
Why are cancer rates rising in the U.S.?
Since the 1990s, cancer rates have been on the rise globally and in the U.S., most notably in people under 50. Increased cancer screening may partially explain the rising number of cancer diagnoses. Exposure to air pollution and lifestyle factors like tobacco use, alcohol use, and diet may also be contributing factors.
What are the benefits of staying up to date on COVID-19 vaccines?
Staying up to date on COVID-19 vaccines is a safe way to protect our long-term health. COVID-19 vaccines prevent severe illness, hospitalization, death, and long COVID.
The CDC says staying up to date on COVID-19 vaccines is a safer and more reliable way to build protection against COVID-19 than getting sick from COVID-19.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Regular Nail Polish vs Gel Nail Polish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing regular nail polish to gel nail polish, we picked the regular.
Why?
This one’s less about what’s in the bottle, and more about what gets done to your hands:
- Regular nail polish application involves carefully brushing it on.
- Regular nail polish removal involves wiping with acetone.
…whereas:
- Gel nail polish application involves deliberately damaging (roughing up) the nail to allow the color coat to adhere, then when the top coat is applied, holding the nails (and thus, the attached fingers) under a UV light to set it. That UV lamp exposure is very bad for the skin.
- Gel nail polish removal involves soaking in acetone, which is definitely worse than wiping with acetone. Failure to adequately soak it will result in further damage to the nail while trying to get the base coat off the nail that you already deliberately damaged when first applying it.
All in all, regular nail polish isn’t amazing for nail health (healthiest is for nails to be free and naked), but for those of us who like a little bit of color there, regular is a lot better than gel.
Gel nail polish damages the nail itself by necessity, and presents a cumulative skin cancer risk and accelerated aging of the skin, by way of the UV lamp use.
For your interest, here are the specific products that we compared, but the above goes for any of this kind:
Regular nail polish | Gel nail polish
If you’d like to read more about nail health, you might enjoy reading:
The Counterintuitive Dos and Don’ts of Nail Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Stress Affects Your Body
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sharon Bergquist gives us a tour:
Stress, from the inside out
Stress is a natural physical and emotional response to challenges or being overwhelmed. It can be beneficial in short-term situations (e.g. escape from a tiger) but is harmful when prolonged or frequent (e.g. escape the rat-race).
Immediate physiological response: cortisol, adrenaline (epinephrine), and norepinephrine are released by the adrenal glands.
The effects this has (non-exhaustive list; we’re just citing what’s in the video here):
- Cortisol impairs blood vessel function, promoting atherosclerosis.
- Adrenaline increases heart rate and blood pressure, leading to hypertension.
- Stress disrupts the brain-gut connection, causing:
- Digestive issues like irritable bowel syndrome and heartburn.
- Changes in gut bacteria composition, potentially affecting overall health.
- Cortisol increases appetite and cravings for energy-dense “comfort foods”.
- This in turn promotes visceral fat storage, which raises the risk of heart disease and insulin resistance.
- Immune-specific effects:
- Stress hormones initially aid in healing and immune defense.
- Chronic stress weakens immune function (by over-working it constantly), increasing susceptibility to infections and slowing recovery.
- Other systemic effects:
- Chronic stress shortens telomeres, which protect chromosomes. Shortened telomeres accelerate cellular aging.
- Chronic stress can also cause acne, hair loss, sexual dysfunction, headaches, muscle tension, fatigue, irritability, and difficulty concentrating.
So, how to manage this? The video says that viewing stressful situations as controllable challenges, rather than insurmountable threats, leads to better short-term performance and long-term health.
Which would be wonderful, except that usually things are stressful precisely because they are not entirely within the field of our control, and the usual advice is to tend to what we can control, and accept what we can’t.
However… That paradigm still leaves out the very big set of “this might be somewhat within our control or it might not; we really don’t know yet; we can probably impact it but what if we don’t do enough, or take the wrong approach and do the wrong thing? And also we have 17 competing stressors, which ones should we prioritize tending to first, and…” and so on.
To that end, we suggest checking out the “Want to learn more?” link we drop below the video today, as it is about managing stress realistically, in a world that, if we’re honest about it, can sometimes be frankly unmanageable.
Meanwhile, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Heart Health vs Systemic Stress ← this is good in and of itself, and also links to other stress-related resources of ours
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: