Caffeine Blues – by Stephen Cherniske
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Caffeine use is an interesting and often-underexamined factor in health. Beyond the most superficial of sleep hygiene advice (à la “if you aren’t sleeping well, consider skipping your triple espresso martini at bedtime”), it’s often considered a “everybody has this” drug.
In this book, Cherniske explores a lot of the lesser-known effects of caffeine, and the book certainly is a litany against caffeine dependence, ultimately arguing strongly against caffeine use itself. The goal is certainly to persuade the reader to desist in caffeine use, and while the book’s selling point is “learn about caffeine” not “how to quit caffeine”, a program for quitting caffeine is nevertheless included.
You may notice the title and cover design are strongly reminiscent of “Sugar Blues”, which came decades before it, and that’s clearly not accidental. The style is similar—very sensationalist, and with a lot of strong claims. In this case, however, there is actually a more robust bibliography, albeit somewhat dated now as science has continued to progress since this book was published.
Bottom line: in this reviewer’s opinion, the book overstates its case a little, and is prone to undue sensationalism, but there is a lot of genuinely very good information in here too, making it definitely worth reading.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chili Chestnut, Sweet Apricot, & Whipped Feta Toasts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a delightful breakfast or light lunch option, full of gut-healthy ingredients and a fair list of healthy polyphenols too.
You will need
- ½ baguette, sliced into ½” slices; if making your own, feel free to use our Delicious Quinoa Avocado Bread recipe. If buying shop-bought, a sourdough baguette will likely be the healthiest option, and tasty too.
- 4 oz feta cheese; if you are vegan, a plant-based version will work in culinary terms, but will have a different (less gut-healthy) nutritional profile, as plant-based cheeses generally use a lot of coconut oil and potato starch, and are not actually fermented.
- 1 tbsp yogurt; your preference what kind; live-cultured with minimal additives is of course best—and this time, plant-based is also just as good, healthwise, since they are fermented and contain more or less the same beneficial bacteria, and have a good macro profile too.
- 4 oz precooked chestnuts, finely chopped
- 6 dried apricots, finely chopped
- ¼ bulb garlic, grated
- 2 tsp harissa paste
- 1 tsp black pepper, coarse ground
- ¼ tsp MSG or ½ tsp low-sodium salt
- Extra virgin olive oil, for frying
- Optional garnish: finely chopped chives
Method
(we suggest you read everything at least once before doing anything)
1) Combine the feta and yogurt in a small, high-speed blender and process into a smooth purée. If it isn’t working, add 1 tbsp kettle-hot water and try again.
2) Heat the oil in a skillet over a medium heat; add the garlic and when it starts to turn golden, add the chestnuts and harissa, as well as the black pepper and MSG/salt. Stir for about 2 minutes, and then stir in the apricots and take it off the heat.
3) Toast the baguette slices under the grill. If you’re feeling bold about the multitasking, you can start this while still doing the previous step, for optimal timing. If not, simply doing it in the order presented is fine.
4) Assemble: spread the whipped feta over the toast; add the apricot-chestnut mixture, followed by the finely chopped chives if using, and serve immediately:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Apricots vs Peaches – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Capsaicin For Weight Loss And Against Inflammation
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Sea Salt vs MSG – Which is Healthier?
Take care!
Share This Post
-
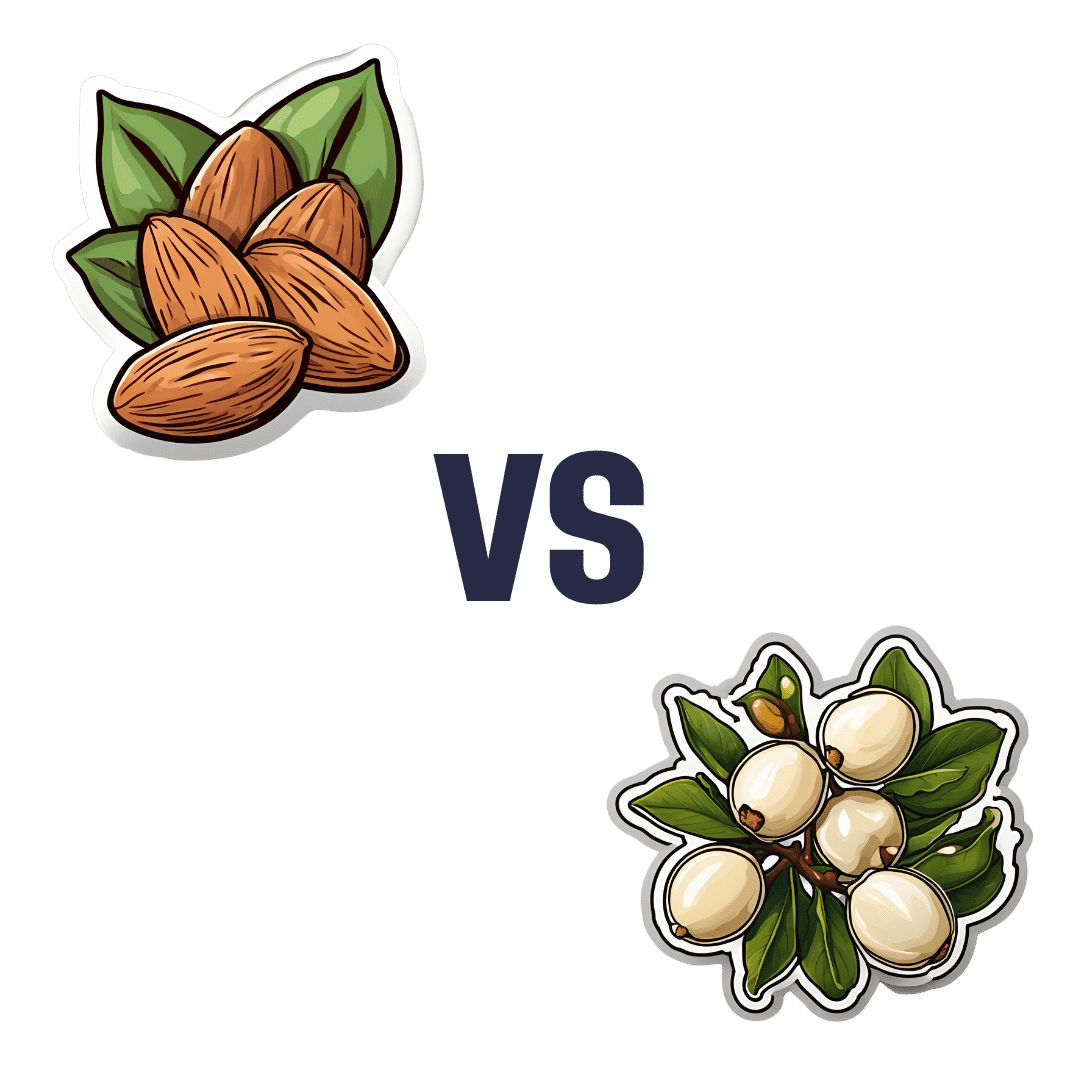
Almonds vs Macadamias – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to macadamias, we picked the almonds.
Why?
It’s not just our pro-almonds bias:
In terms of macros, almonds have 3x the protein and as well as more fiber and carbs, the ratio of which latter two give almonds the lower glycemic index, while macadamias have more total fat, and 4x the saturated fat percentage. All in all, we say this is a win for almonds in this category.
In the category of vitamins, almonds have more of vitamins B2, B3, B9, E, and choline, while macadamias have more of vitamins B1, B5, B6, and C. A modest 5:4 win for almonds, unless we consider that almonds have more than 47x as much vitamin E (almonds are an exceptionally good source of vitamin E), in which case, a stronger win for almonds.
When it comes to minerals, almonds have more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while macadamias have more manganese. A very clear win for almonds.
Adding up the sections makes for a convincing overall win for almonds, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Why You Should Diversify Your Nuts!
Enjoy!
Share This Post
-
Your Vitamins are Obsolete: The Vitamer Revolution – by Dr. Sheldon Zablow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not:a book to tell you “throw out your vitamins and just eat these foods”.
This book focuses mainly on two vitamins in which deficiencies are common especially as we get older: B9 and B12.
So, what does the title mean? It’s not so much that your vitamins are obsolete—that would imply that they were more useful previously, which is not the case. Rather, the most common forms of vitamins B9 and B12 provided in supplements are folic acid and cyanocobalamin, respectively, which as he demonstrates with extensive research to back up his claims, cannot be easily absorbed or used especially well.
About those vitamers: a vitamer is simply a form of a vitamin—most vitamins we need can arrive in a variety of forms. In the case of vitamins B9 and B12, he advocates for ditching vitamers folic acid and cyanocobalamin, cheap as they are, and springing for bioactive vitamers L-methylfolate, methylcobalamin, and adenosylcobalamin.
He also discusses (again, just as well-evidenced as the above things) why we might struggle to get enough from our diet after a certain age. For example, if trying to get these vitamins from meat, 50% of people over 50 cannot manufacture enough stomach acid to break down that protein to release the vitamins.
And as for methyl-B12 vitamers, you might expect you can get those from meat, and technically you can, but they don’t occur in all animals, just in one kind of animal. Specifically, the kind that has the largest brain-to-body ratio. However, eating the meat of this animal can result in protein folding errors in general and Creutzfeldt–Jakob disease in particular, so the author does not recommend eating humans, however nutritionally convenient that would be.
All this means that supplementation after a certain age really can be a sensible way to do it—but do it wisely, and pick the right vitamers.
The style of the book is informationally dense, but very readable even for a layperson provided one starts at the beginning and reads forwards, as otherwise one will find oneself in a mire of terms whose explanations one missed when they were first introduced.
Bottom line: if you are over 50 and/or have any known or suspected issues with vitamins B9 and/or B12, this book becomes very important reading.
Click here to check out Your Vitamins Are Obsolete, and get your body what it needs!
Share This Post
Related Posts
-
The Best Exercise to Stop Your Legs From Giving Out
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Doug Weiss, seniors-specialist physio, has an exercise that stops your knees from being tricked into collapsing (which is very common) by a misfiring (also common) reflex.
Step up…
Setup to step up thus:
- Use a sturdy support like a countertop or chair.
- Have an aerobic step or similar firm surface to step onto.
When you’re ready:
- Stand facing away from the step.
- Place one hand on the support for stability.
- Step backwards up onto the step with your right leg, then your left leg, so both feet are on the step.
- Step forward to come back down.
Once you’re confident of the series of movements, do it without the support, and do it for a few minutes each day. Don’t worry about how easy it becomes; this is not, first and foremost, a strength-training exercise; you don’t have to start adding weights or anything (although of course you can if you want).
How it works: there’s a part of you called the Golgi tendon organ, and it can trigger a Golgi tendon reflex, which is one of the body’s equivalents of a steam valve. However, instead of letting off steam to avoid a boiler explosion, it collapses a joint to save it from overload. However, if not exercised regularly, it can get overly sensitive, causing it to mistake your mere bodyweight for an overload. So, it collapses, thinking it is saving you from snapping a tendon, but it’s not. By exercising in the way described, the Golgi tendon reflex will go back to only being triggered by an actual overload, not the mere act of stepping.
Writer’s note: this one’s interesting to me as I have a) a strong lower body b) hypermobile joints that thus occasionally just fold like laundry regardless. Could it be that this will fix that? I guess I’ll find out 🙂
Meanwhile, for more on all of the above plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
What Nobody Teaches You About Strengthening Your Knees
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Longevity Code – by Dr. Kris Verburgh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the subtitle claim of “secrets from the leading edge of science”, we’ll note up front that this book was published in 2015, and what was new then, isn’t now. However, what was new then is still important now, so we think the book merits attention just the same.
The book examines why certain creatures (like humans) seem programmed to grow old and die, and why others (few others, but enough to make a list) either simply do not age, or else do age but can become younger when they hit a certain point. If this is the first you’re hearing of biologically immortal creatures, we’ll mention: they can and do die, just, their cause of death is usually by being eaten. But on a cellular and structural level, they don’t age. They grow to maturity and then just stay that way until one day they get eaten (or fall to some similar external circumstance).
Tackling the question of “why do we age?” (not as a philosophical question, but rather as an engineering question) is important to tackle the critical question of “…and could we not?”, and that’s what much of this book is about.
The real reason that compared to other mammals, humans live (for example) slightly longer than bats but not as long as naked mole rats, comes down mostly to genes, which makes it sound like things are set in stone, but rather, even without outright gene-editing technologies like CRISPR, gene expression is often quite modifiable, and often modifiable not just by drugs, but also by supplements, and indeed by nutraceuticals, which means also by diet, plus diet-adjacent things like fasting.
While this is mostly an explanatory book rather than a how-to, there’s enough to make practical use of, and even a recipes section.
The style is very gripping pop-science—or at least, if you’re anything like this reviewer, you’ll find it a page-turner. While being light on citations as we go (not like some authors who will mark several citations per page, or in the extreme, for every declarative sentence made), there is a reassuring bibliography at the back.
Bottom line: if you’re interested in the “under the hood” of aging, then you will love this book.
Click here to check out The Longevity Code, and slow down the aging process to live well for longer!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
This Naked Mind – by Annie Grace
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all read about the many, many, dangers of drinking. We’ve also probably all read about how to make the change to not drinking. Put things out of sight, tell your friends, have this rule, have this excuse (for not drinking) ready to give to people who challenge you, consider a support group, and so on.
What Annie Grace offers in this #1 bestseller is different:
A blend of mostly psychology and sociology, to examine the “liminal thinking” stages that funnel us to drink in the first place… and where that leads, and how to clamber back out of the pitcher plant we weren’t necessarily aware we were sliding into.
While she kicks off citing Jung, from a psychological perspective more of this book is CBTish, as it pertains a lot to examining the process of:
- belief—held and defended, based on the…
- conclusion—drawn, often irrationally, from the…
- experience—that we had upon acting on an…
- observation—often mistaking an illusion for the underlying…
- reality
…and how we can and often do go wrong at each step, and how little of the previous steps we can perceive at any given time.
What does this mean for managing/treating alcoholism or a tendency towards alchoholism?
It means interrupting those processes in a careful, surgically precise fashion, so that suddenly… The thing has no more power over us.
Whether you or a loved one struggle with a tendency to addiction (any addiction, actually, the advice goes the same), or are just curious about the wider factors at hand in the epidemiology of addiction, this book is for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: