Brain Wash – by Dr. David Perlmutter, Dr. Austin Perlmutter, and Kristen Loberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be familiar with the lead author of this book, Dr. David Perlmutter, as a big name in the world of preventative healthcare. A lot of his work has focused specifically on carbohydrate metabolism, and he is as associated with grains and he is with brains. This book focuses on the latter.
Dr. Perlmutter et al. take a methodical look at all that is ailing our brains in this modern world, and systematically lay out a plan for improving each aspect.
The advice is far from just dietary, though the chapter on diet takes a clear stance:
❝The food you eat and the beverages you drink change your emotions, your thoughts, and the way you perceive the world❞
The style is explanatory, and the book can be read comfortably as a “sit down and read it cover to cover” book; it’s an enjoyable, informative, and useful read.
Bottom line: if you’d like to give your brain a gentle overhaul, this is the one-stop-shop book to give you the tools to do just that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
STI rates are increasing among midlife and older adults. We need to talk about it
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Globally, the rates of common sexually transmissible infections (STIs) are increasing among people aged over 50. In some cases, rates are rising faster than among younger people.
Recent data from the United States Centers for Disease Control and Prevention shows that, among people aged 55 and older, rates of gonorrhoea and chlamydia, two of the most common STIs, more than doubled between 2012 and 2022.
Australian STI surveillance data has reflected similar trends. Between 2013 and 2022, there was a steady increase in diagnoses of chlamydia, gonorrhoea and syphilis among people aged 40 and older. For example, there were 5,883 notifications of chlamydia in Australians 40 plus in 2013, compared with 10,263 in 2022.
A 2020 study of Australian women also showed that, between 2000 and 2018, there was a sharper increase in STI diagnoses among women aged 55–74 than among younger women.
While the overall rate of common STIs is highest among young adults, the significant increase in STI diagnoses among midlife and older adults suggests we need to pay more attention to sexual health across the life course.
Fit Ztudio/Shutterstock Why are STI rates rising among older adults?
STI rates are increasing globally for all age groups, and an increase among midlife and older people is in line with this trend.
However, increases of STIs among older people are likely due to a combination of changing sex and relationship practices and hidden sexual health needs among this group.
The “boomer” generation came of age in the 60s and 70s. They are the generation of free love and their attitude to sex, even as they age, is quite different to that of generations before them.
Given the median age of divorce in Australia is now over 43, and the internet has ushered in new opportunities for post-separation dating, it’s not surprising that midlife and older adults are exploring new sexual practices or finding multiple sexual partners.
People may start new relationships later in life. Tint Media/Shutterstock It’s also possible midlife and older people have not had exposure to sexual health education in school or do not relate to current safe sex messages, which tend to be directed toward young people. Condoms may therefore seem unnecessary for people who aren’t trying to avoid pregnancy. Older people may also lack confidence negotiating safe sex or accessing STI screening.
Hidden sexual health needs
In contemporary life, the sex lives of older adults are largely invisible. Ageing and older bodies are often associated with loss of power and desirability, reflected in the stereotype of older people as asexual and in derogatory jokes about older people having sex.
With some exceptions, we see few positive representations of older sexual bodies in film or television.
Older people’s sexuality is also largely invisible in public policy. In a review of Australian policy relating to sexual and reproductive health, researchers found midlife and older adults were rarely mentioned.
Sexual health policy generally targets groups with the highest STI rates, which excludes most older people. As midlife and older adults are beyond childbearing years, they also do not feature in reproductive health policy. This means there is a general absence of any policy related to sex or sexual health among midlife or older adults.
Added to this, sexual health policy tends to be focused on risk rather than sexual wellbeing. Sexual wellbeing, including freedom and capacity to pursue pleasurable sexual experiences, is strongly associated with overall health and quality of life for adults of all ages. Including sexual wellbeing as a policy priority would enable a focus on safe and respectful sex and relationships across the adult life course.
Without this priority, we have limited knowledge about what supports sexual wellbeing as people age and limited funding for initiatives to engage with midlife or older adults on these issues.
Midlife and older adults may have limited knowledge about STIs. Southworks/Shutterstock How can we support sexual health and wellbeing for older adults?
Most STIs are easily treatable. Serious complications can occur, however, when STIs are undiagnosed and untreated over a long period. Untreated STIs can also be passed on to others.
Late diagnosis is not uncommon as some STIs can have no symptoms and many people don’t routinely screen for STIs. Older, heterosexual adults are, in general, less likely than other groups to seek regular STI screening.
For midlife or older adults, STIs may also be diagnosed late because some doctors do not initiate testing due to concerns they will cause offence or because they assume STI risk among older people is negligible.
Many doctors are reluctant to discuss sexual health with their older patients unless the patient explicitly raises the topic. However, older people can be embarrassed or feel awkward raising matters of sex.
Resources for health-care providers and patients to facilitate conversations about sexual health and STI screening with older patients would be a good first step.
To address rising rates of STIs among midlife and older adults, we also need to ensure sexual health promotion is targeted toward these age groups and improve accessibility of clinical services.
More broadly, it’s important to consider ways to ensure sexual wellbeing is prioritised in policy and practice related to midlife and older adulthood.
A comprehensive approach to older people’s sexual health, that explicitly places value on the significance of sex and intimacy in people’s lives, will enhance our ability to more effectively respond to sexual health and STI prevention across the life course.
Jennifer Power, Associate Professor and Principal Research Fellow, Australian Research Centre in Sex, Health and Society, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
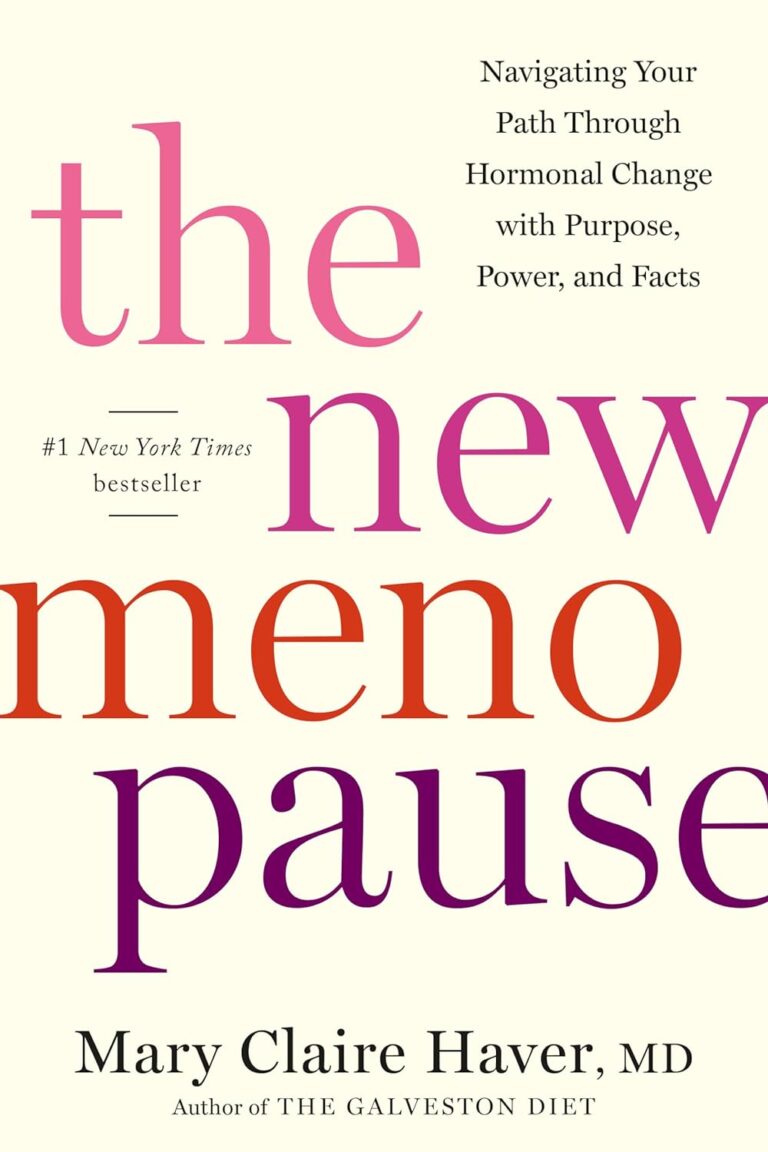
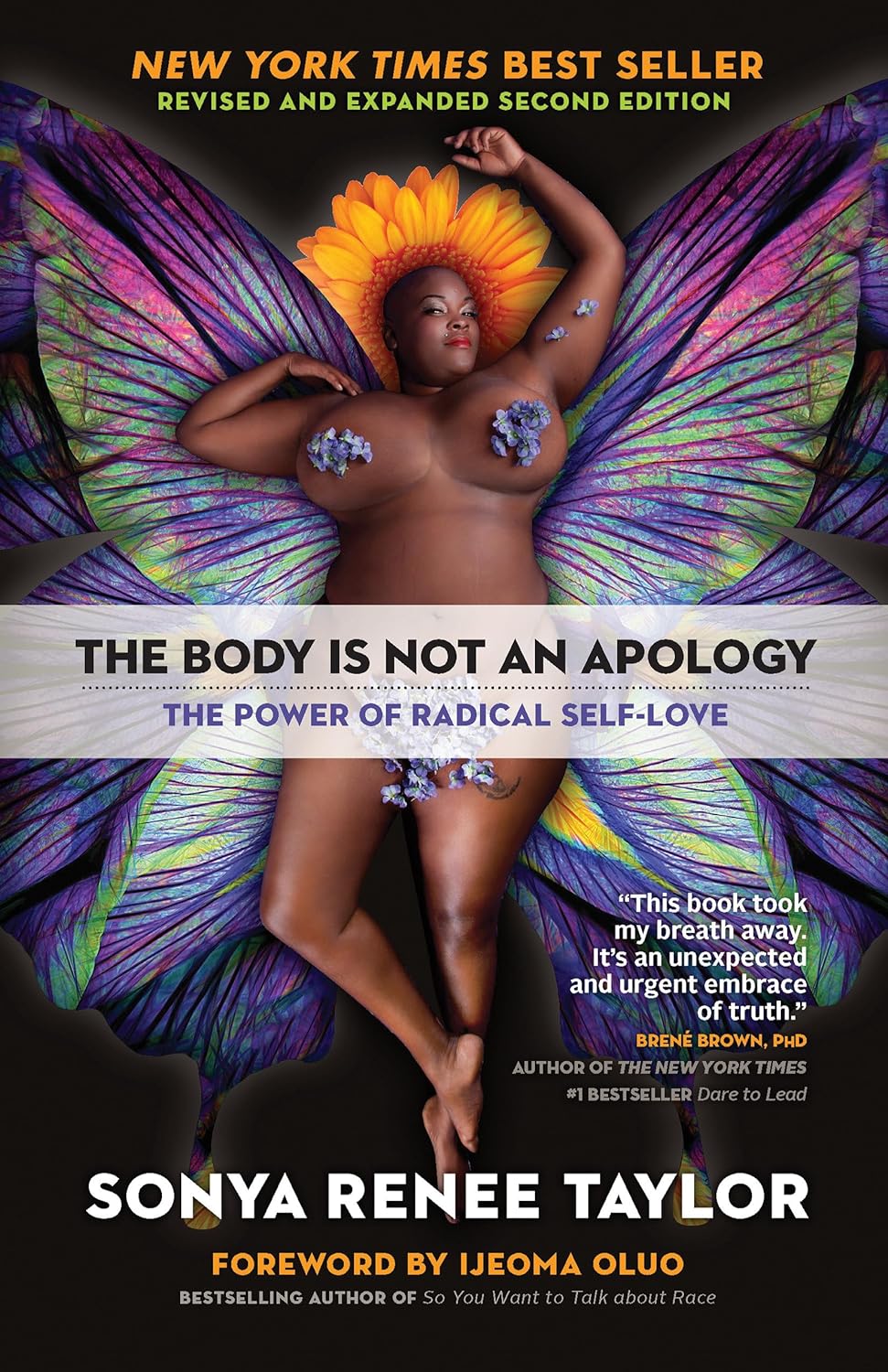
The Body Is Not an Apology – by Sonya Renee Taylor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a couple of things that this book is not about:
- Self-confidence (it’s about more than merely thinking highly of oneself)
- Self-acceptance (it’s about more than merely settling for “good enough”)
In contrast, it’s about loving and celebrating what is, while striving for better, for oneself and for others.
You may be wondering: whence this “radical” in the title?
The author argues that often, the problem with our bodies is not actually our bodies. If we have cancer, or diabetes, then sure, that’s a problem with the body. But most of the time, the “problem with our bodies” is simply society’s rejection of our “imperfect” bodies as somehow “less than”, and something we must invest time and money to correct. Hence, the need for a radical uprooting of ideas, to fix the real problem.
Bottom line: if, like most of us, you have a body that would not entirely pass for that of a Marvel Comics superhero, this is a book for you. And if you do have a MCU body? This is also a book for you, because we have bad news for you about what happens with age.
Click here to check out The Body Is Not An Apology, and appreciate more about yours!
Share This Post
-
Older adults need another COVID-19 vaccine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- The CDC recommends people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine.
- Updated COVID-19 vaccines are effective at protecting against severe illness, hospitalization, death, and long COVID.
- The CDC also shortened the isolation period for people who are sick with COVID-19.
Last week, the CDC said people 65 and older should receive an additional dose of the updated COVID-19 vaccine this spring. The recommendation also applies to immunocompromised people, who were already eligible for an additional dose.
Older adults made up two-thirds of COVID-19-related hospitalizations between October 2023 and January 2024, so enhancing protection for this group is critical.
The CDC also shortened the isolation period for people who are sick with COVID-19, although the contagiousness of COVID-19 has not changed.
Read on to learn more about the CDC’s updated vaccination and isolation recommendations.
Who is eligible for another COVID-19 vaccine this spring?
The CDC recommends that people ages 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring—if at least four months have passed since they received a COVID-19 vaccine. It’s safe to receive an updated COVID-19 vaccine from Pfizer, Moderna, or Novavax, regardless of which COVID-19 vaccines you received in the past.
Updated COVID-19 vaccines are available at pharmacies, local clinics, or doctor’s offices. Visit Vaccines.gov to find an appointment near you.
Under- and uninsured adults can get the updated COVID-19 vaccine for free through the CDC’s Bridge Access Program. If you’re over 60 and unable to leave your home, call the Aging Network at 1-800-677-1116 to learn about free at-home vaccination options.
What are the benefits of staying up to date on COVID-19 vaccines?
Staying up to date on COVID-19 vaccines prevents severe illness, hospitalization, death, and long COVID.
Additionally, the CDC says staying up to date on COVID-19 vaccines is a safer and more reliable way to build protection against COVID-19 than getting sick from COVID-19.
What are the new COVID-19 isolation guidelines?
According to the CDC’s general respiratory virus guidance, people who are sick with COVID-19 or another common respiratory illness, like the flu or RSV, should isolate until they’ve been fever-free for at least 24 hours without the use of fever-reducing medication and their symptoms improve.
After that, the CDC recommends taking additional precautions for the next five days: wearing a well-fitting mask, limiting close contact with others, and improving ventilation in your home if you live with others.
If you’re sick with COVID-19, you can infect others for five to 12 days, or longer. Moderately or severely immunocompromised patients may remain infectious beyond 20 days.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Kate Middleton is having ‘preventive chemotherapy’ for cancer. What does this mean?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Catherine, Princess of Wales, is undergoing treatment for cancer. In a video thanking followers for their messages of support after her major abdominal surgery, the Princess of Wales explained, “tests after the operation found cancer had been present.”
“My medical team therefore advised that I should undergo a course of preventative chemotherapy and I am now in the early stages of that treatment,” she said in the two-minute video.
No further details have been released about the Princess of Wales’ treatment.
But many have been asking what preventive chemotherapy is and how effective it can be. Here’s what we know about this type of treatment.
It’s not the same as preventing cancer
To prevent cancer developing, lifestyle changes such as diet, exercise and sun protection are recommended.
Tamoxifen, a hormone therapy drug can be used to reduce the risk of cancer for some patients at high risk of breast cancer.
Aspirin can also be used for those at high risk of bowel and other cancers.
How can chemotherapy be used as preventive therapy?
In terms of treating cancer, prevention refers to giving chemotherapy after the cancer has been removed, to prevent the cancer from returning.
If a cancer is localised (limited to a certain part of the body) with no evidence on scans of it spreading to distant sites, local treatments such as surgery or radiotherapy can remove all of the cancer.
If, however, cancer is first detected after it has spread to distant parts of the body at diagnosis, clinicians use treatments such as chemotherapy (anti-cancer drugs), hormones or immunotherapy, which circulate around the body .
The other use for chemotherapy is to add it before or after surgery or radiotherapy, to prevent the primary cancer coming back. The surgery may have cured the cancer. However, in some cases, undetectable microscopic cells may have spread into the bloodstream to distant sites. This will result in the cancer returning, months or years later.
With some cancers, treatment with chemotherapy, given before or after the local surgery or radiotherapy, can kill those cells and prevent the cancer coming back.
If we can’t see these cells, how do we know that giving additional chemotherapy to prevent recurrence is effective? We’ve learnt this from clinical trials. Researchers have compared patients who had surgery only with those whose surgery was followed by additional (or often called adjuvant) chemotherapy. The additional therapy resulted in patients not relapsing and surviving longer.
How effective is preventive therapy?
The effectiveness of preventive therapy depends on the type of cancer and the type of chemotherapy.
Let’s consider the common example of bowel cancer, which is at high risk of returning after surgery because of its size or spread to local lymph glands. The first chemotherapy tested improved survival by 15%. With more intense chemotherapy, the chance of surviving six years is approaching 80%.
Preventive chemotherapy is usually given for three to six months.
How does chemotherapy work?
Many of the chemotherapy drugs stop cancer cells dividing by disrupting the DNA (genetic material) in the centre of the cells. To improve efficacy, drugs which work at different sites in the cell are given in combinations.
Chemotherapy is not selective for cancer cells. It kills any dividing cells.
But cancers consist of a higher proportion of dividing cells than the normal body cells. A greater proportion of the cancer is killed with each course of chemotherapy.
Normal cells can recover between courses, which are usually given three to four weeks apart.
What are the side effects?
The side effects of chemotherapy are usually reversible and are seen in parts of the body where there is normally a high turnover of cells.
The production of blood cells, for example, is temporarily disrupted. When your white blood cell count is low, there is an increased risk of infection.
Cell death in the lining of the gut leads to mouth ulcers, nausea and vomiting and bowel disturbance.
Certain drugs sometimes given during chemotherapy can attack other organs, such as causing numbness in the hands and feet.
There are also generalised symptoms such as fatigue.
Given that preventive chemotherapy given after surgery starts when there is no evidence of any cancer remaining after local surgery, patients can usually resume normal activities within weeks of completing the courses of chemotherapy.
Ian Olver, Adjunct Professsor, School of Psychology, Faculty of Health and Medical Sciences, University of Adelaide
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dr. Suzanne Steinbaum’s Heart Book – by Dr. Suzanne Steinbaum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book is divided into three parts:
- What you should know
- What you should do
- All about you
This is a very useful format, since it lays out all the foundational knowledge, before offering practical advice and “how to” explanations, before finally wrapping up with personalizing things.
The latter is important, because while our basic risk factors can be assembled in a few lines of data (age, sex, race, genes, diet, exercise habits, etc) there’s a lot more to us than that, and oftentimes the data that doesn’t make the cut, makes the difference. Hormones on high on this list; we can say that a person is a 65-year-old woman and make a guess, but that’s all it is: a guess. Very few of us are the “average person” that statistical models represent accurately. And nor are social and psychological factors irrelevant; in fact often they are deciding factors!
So, it’s important to be able to look at ourselves as the whole persons we are, or else we’ll get a heart-healthy protocol that works on paper but actually falls flat in application, because the mathematical model didn’t take into account that lately we have been very stressed about such-and-such a thing, and deeply anxious about so-and-so, and a hopefully short-term respiratory infection has reduced blood oxygen levels, and all these kinds of things need to be taken into account too, for an overall plan to work.
The greatest strength of this book is that it attends to that.
The style of the book is a little like a long sales pitch (when all that’s being sold, by the way, is the ideas the book is offering; she wants you to take her advice with enthusiasm), but there’s plenty of very good information all the way through, making it quite worth the read.
Bottom line: if you’re a woman and/or love at least one woman, then you can benefit from this important book for understanding heart health that’s not the default.
Click here to check out Dr. Suzanne Steinbaum’s Heart Book, and enjoy a heart-healthy life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Fruits Every Senior Should Eat Today (And Why)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What will you prioritize in the new year?
Fruits to enjoy regularly
The 7 fruits recommended for seniors in this video are:
Apples
- Rich in soluble fiber (pectin) for lowering LDL cholesterol.
- Contains phytochemicals such as quercetin and other polyphenols that reduce inflammation and support heart health.
- High in vitamin C for immunity, skin elasticity, and joint health.
Bananas
- Natural energy boost from carbohydrates.
- High in potassium for regulating blood pressure, fluid balance, and preventing muscle cramps.
- Supports cardiovascular health and muscle function.
Avocados
- Rich in monounsaturated fats to improve cholesterol levels.
- High in potassium for blood pressure regulation.
- Contains vitamins E and K for brain health and bone density.
Grapes
- Hydrating and rich in antioxidants like resveratrol, which supports circulation and reduces inflammation.
- Contain vitamins C and K for immunity and bone health.
Plums
- Natural laxative with high fiber and sorbitol for digestive health.
- Rich in potassium and vitamin K for bone density and reducing osteoporosis risk.
- Contain polyphenols for reducing inflammation and supporting cognitive health.
Pomegranates
- Anti-inflammatory and antioxidant-rich (especially punicalagins and anthocyanins).
- Supports heart health, improves cholesterol levels, and promotes brain health.
- May help inhibit cancer cell growth in specific types.
Kiwi
- High in vitamin C to boost immunity.
- Rich in fiber and enzymes for digestive health.
- Low glycemic index, suitable for blood sugar management.
10almonds note: a lot of those statements can go for a lot of fruits, but those are definitely high on the list for the qualities mentioned!
For more on all the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Top 8 Fruits That Prevent & Kill Cancer ← there are two fruits that appear on both lists!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: