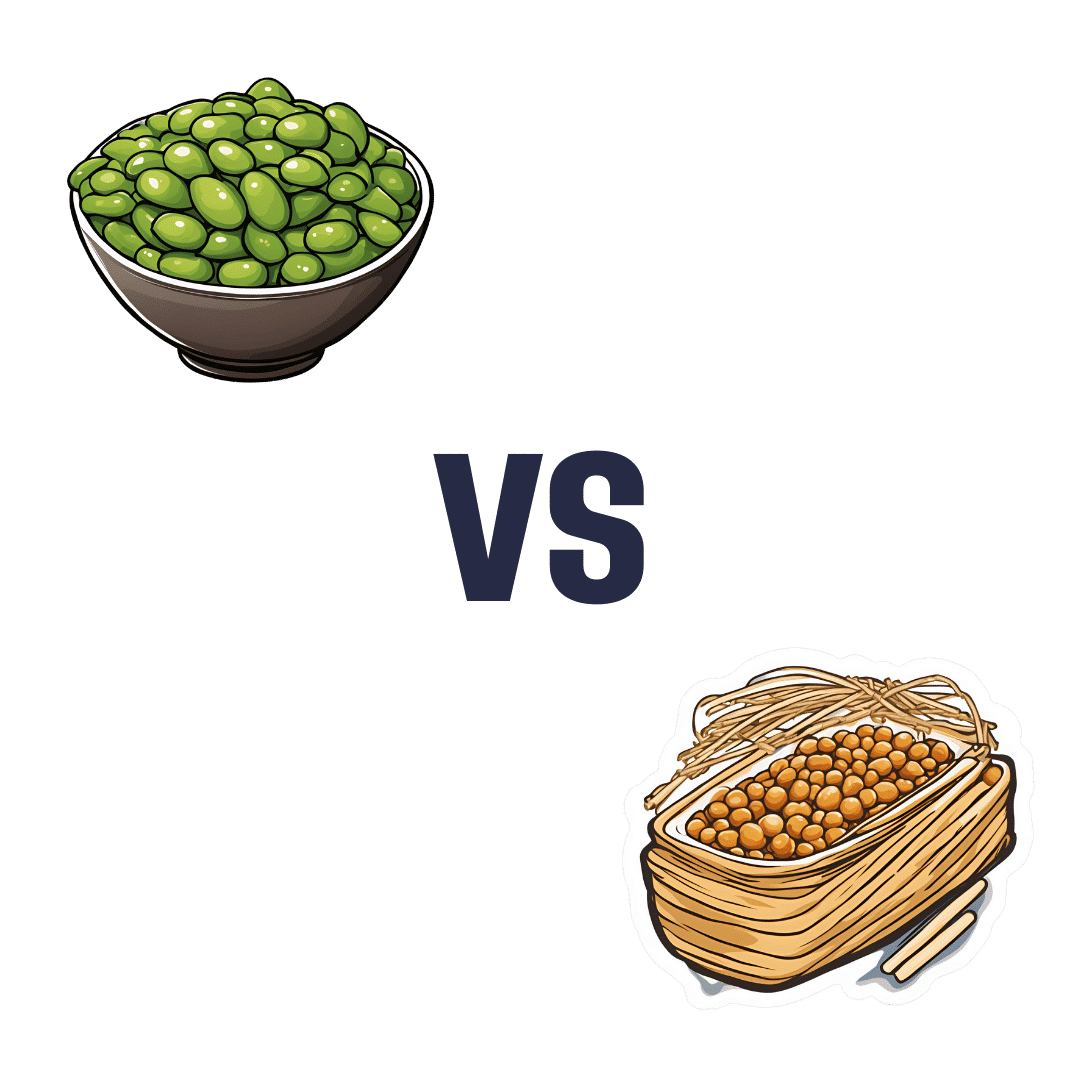
Edamame vs Natto – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edamame to nattō, we picked the nattō.
Why?
Yes, they are both soy beans, but in the battle of young and green vs old and fermented, there are some important differences:
In terms of macros, nattō has nearly 2x the protein for only slightly more carbs, and slightly more fiber, as well as more fat, but it’s not much and it’s a healthy profile, mostly polyunsaturated. All in all, a win for nattō in the macros category.
In the category of vitamins, edamame has more of vitamins B1, B5, B9, E, and K, while nattō has more of vitamins B2, B6, and C, this a 5:3 win for edamame in this round.
When it comes to minerals, edamame is not higher in any minerals, while nattō has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for nattō.
A word on phytoestrogens: soy in general contains these, including both of these iterations of soy, and/but the human body can’t use plant estrogens as such. What it can do, however, is break them down and use the bits to make human estradiol, if and only if you have ovaries that are present and operational (so, no menopause and/or bilateral ovariectomy). Either way, there’s nothing to set one ahead of the other in this matter in this head-to-head.
As an extra point in nattō’s favor, nattō is, like many fermented foods, extra-good for gut health by bringing a wealth of beneficial bacteria. Edamame is also good for gut health (just by virtue of being an edible plant and containing fiber), but not on the same level as nattō.
Adding up the sections makes a clear win for nattō, but by all means enjoy either or both—diversity is good!
Want to learn more?
You might like:
21% Stronger Bones in a Year at 62? Yes, It’s Possible (No Calcium Supplements Needed!) ← nattō features in the method!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
What Happens To Your Body When You Do 100 Glute Bridges Every Day
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not just for a sculpted butt:
Benefits
With consistent daily glute bridge practice, you may expect:
- Rounder, toned butt: targets the gluteus maximus, toning and lifting the butt for a rounder appearance.
- Improved posture: strengthens glutes to support the spine and pelvis, alleviating lower back and hip pain. Stretches tight hip flexors from prolonged sitting.
- Stronger lower back: glutes support the lower back and spine, reducing pain and making it easier to lift heavy objects. Activating the glutes transfers force from legs to core, preventing injuries.
- Stronger knees: stabilizes the knee joint and promotes alignment by engaging glutes, hamstrings, and quadriceps, reducing knee pain.
- Sculpted hamstrings: contracts hamstrings during lifts for strength, while stretching them on the way down increases flexibility.
- Increased hip flexibility: strengthens muscles around the hip joint, improving mobility and counteracting tight hips from sedentary habits.
- Reduced back pain: strengthens glutes to correct pelvic tilt and reduce strain on the lower back.
- Faster running speed: improves hip extension, strengthens hamstrings, and activates the gluteus medius for better running power and balance.
- Enhanced strength training performance: strengthens glutes, back, and knees, improving performance in exercises like squats and deadlifts.
As for how to get going, the video offers the following very sound advice: begin with 25–30 reps per session and gradually increase to sets of 100 daily. It should take about 5 minutes (that’s 3 seconds per repetition). Results can be seen in as little as 2 weeks, with significant changes after a month of consistent practice.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Strong Curves: A Woman’s Guide to Building a Better Butt and Body – by Bret Contreras & Kellie Davis
Take care!
Share This Post
-
Nutrivore – by Dr. Sarah Ballantyne
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The core idea of this book is that foods can be assigned a numerical value according to their total nutritional value, and that this number can be used to guide a person’s diet such that we will eat, in aggregate, a diet that is more nutritious. So far, so simple.
What Dr. Ballantyne also does, besides explaining and illustrating this system (there are chapters explaining the calculation system, and appendices with values), is also going over what to consider important and what we can let slide, and what things we might need more of to address a wide assortment of potential health concerns. And yes, this is definitely a “positive diet” approach, i.e. it focuses on what to add in, not what to cut out.
The premise of the “positive diet” approach is simple, by the way: if we get a full set of good nutrients, we will be satisfied and not crave unhealthy food.
She also offers a lot of helpful “rules of thumb”, and provides a variety of cheat-sheets and suchlike to make things as easy as possible.
There’s also a recipes section! Though, it’s not huge and it’s probably not necessary, but it’s just one more “she’s thinking of everything” element.
Bottom line: if you’d like a single-volume “Bible of” nutrition-made-easy, this is a very usable tome.
Click here to check out Nutrivore, and start filling up your diet!
Share This Post
Related Posts
-
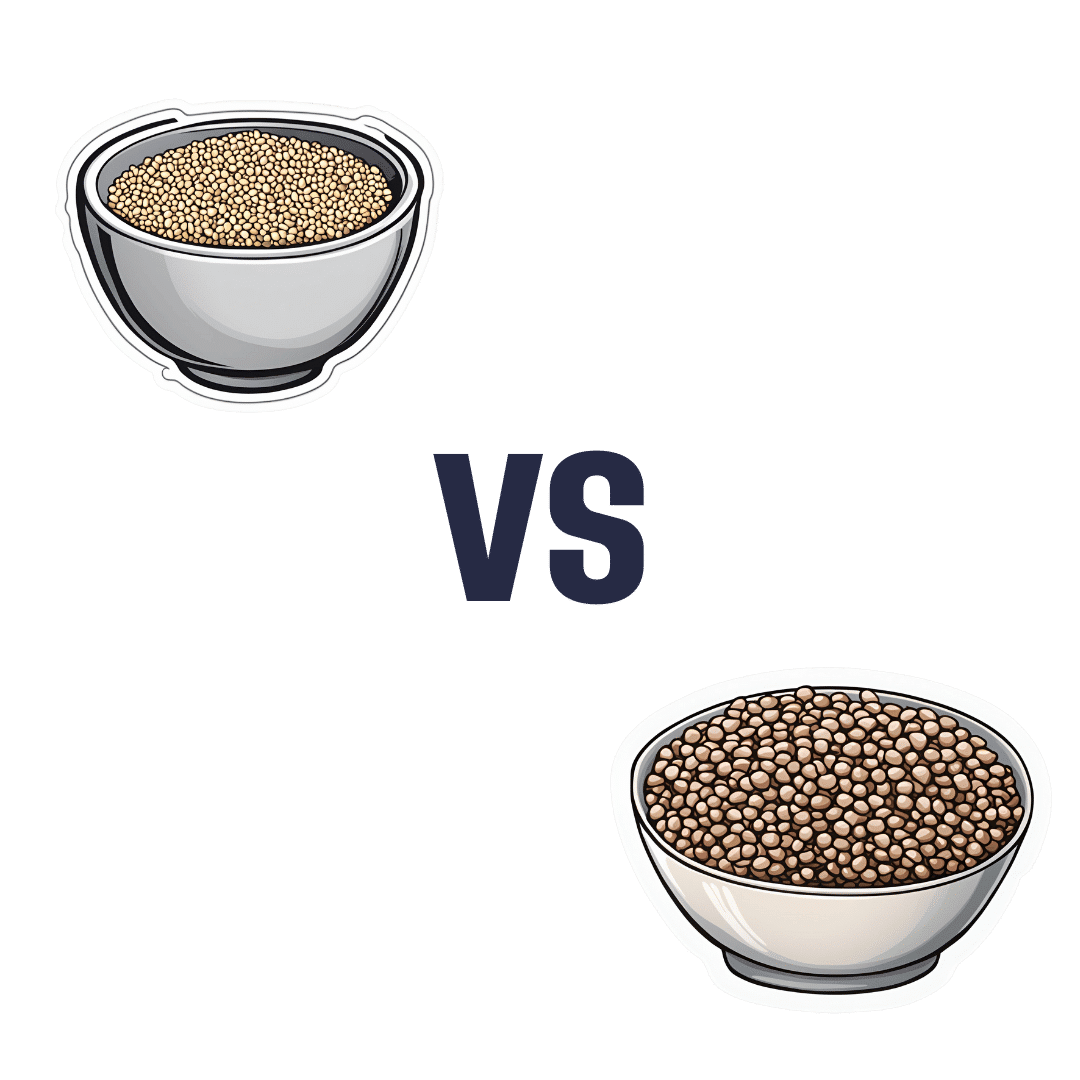
Millet vs Buckwheat – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing millet to buckwheat, we picked the buckwheat.
Why?
Both of these naturally gluten-free grains* have their merits, but we say buckwheat comes out on top for most people (we’ll discuss the exception later).
*actually buckwheat is a flowering pseudocereal, but in culinary terms, we’ll call it a grain, much like we call tomato a vegetable.
Considering the macros first of all, millet has slightly more carbs while buckwheat has more than 2x the fiber. An easy win for buckwheat (they’re about equal on protein, by the way).
In the category of vitamins, millet has more of vitamins B1, B2, B3, B6, and B9, while buckwheat has more of vitamins B5, E, K, and choline. Superficially that’s a 5:4 win for millet, though buckwheat’s margins of difference are notably greater, so the overall vitamin coverage could arguably be considered a tie.
When it comes to minerals, millet has more phosphorus and zinc, while buckwheat has more calcium, copper, iron, magnesium, manganese, potassium, and selenium. For most of them, buckwheat’s margins of difference are again greater. An easy win for buckwheat, in any case.
This all adds up to a clear win for buckwheat, but as promised, there is an exception: if you have issues with your kidneys that mean you are avoiding oxalates, then millet becomes the healthier choice, as buckwheat is rather high in oxalates while millet is low in same.
For everyone else: enjoy both! Diversity is good. But if you’re going to pick one, buckwheat’s the winner.
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Zuranolone: What to know about the pill for postpartum depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the year after giving birth, about one in eight people who give birth in the U.S. experience the debilitating symptoms of postpartum depression (PPD), including lack of energy and feeling sad, anxious, hopeless, and overwhelmed.
Postpartum depression is a serious, potentially life-threatening condition that can affect a person’s bond with their baby. Although it’s frequently confused with the so-called “baby blues,” it’s not the same.
The baby blues include similar, temporary symptoms that affect up to 80 percent of people who have recently given birth and usually go away within the first few weeks. PPD usually begins within the first month after giving birth and can last for months and interfere with a person’s daily life if left untreated. Thankfully, PPD is treatable and there is help available.
On August 4, the FDA approved zuranolone, branded as Zurzuvae, the first-ever oral medication to treat PPD. Until now, besides other common antidepressants, the only medication available to treat PPD specifically was the IV injection brexanolone, which is difficult to access and expensive and can only be administered in a hospital or health care setting.
Read on to find out more about zuranolone: what it is, how it works, how much it costs, and more.
What is zuranolone?
Zurzuvae is the brand name for zuranolone, an oral medication to treat postpartum depression. Developed by Sage Therapeutics in partnership with Biogen, it’s now available in the U.S. Zurzuvae is typically prescribed as two 25 mg capsules a day for 14 days. In clinical trials, the medication showed to be fast-acting, improving PPD symptoms in just three days.
How does zuranolone work?
Zuranolone is a neuroactive steroid, a type of medication that helps the neurotransmitter GABA’s receptors, which affect how the body reacts to anxiety, stress, and fear, function better.
“Zuranolone can be thought of as a synthetic version of [the neuroactive steroid] allopregnanolone,” says Dr. Katrina Furey, a reproductive psychiatrist, clinical instructor at Yale University, and co-host of the Analyze Scripts podcast. “Women with PPD have lower levels of allopregnenolone compared to women without PPD.”
How is it different from other antidepressants?
“What differentiates zuranolone from other previously available oral antidepressants is that it has a much more rapid response and a shorter course of treatment,” says Dr. Asima Ahmad, an OB-GYN, reproductive endocrinologist, and founder of Carrot Fertility.
“It can take effect as early as on day three of treatment, versus other oral antidepressants that can take up to six to 12 weeks to take full effect.”
What are Zurzuvae’s side effects?
According to the FDA, the most common side effects of Zurzuvae include dizziness, drowsiness, diarrhea, fatigue, the common cold, and urinary tract infection. Similar to other antidepressants, the medication may increase the risk of suicidal thoughts and actions in people 24 and younger. However, NPR noted that this type of labeling is required for all antidepressants, and researchers didn’t see any reports of suicidal thoughts in their trials.
“Drug trials also noted that the side effects for zuranolone were not as severe,” says Ahmad. “[There was] no sudden loss of consciousness as seen with brexanolone or weight gain and sexual dysfunction, which can be seen with other oral antidepressants.”
She adds: “Given the lower incidence of side effects and more rapid-acting onset, zuranolone could be a viable option for many,” including those looking for a treatment that offers faster symptom relief.
Can someone breastfeed while taking zuranolone?
It’s complicated. In clinical trials, participants were asked to stop breastfeeding (which, according to Furey, is common in early clinical trials).
A small study of people who were nursing while taking zuranolone found that 0.3 percent of the medication dose was passed on to breast milk, which, Furey says, is a pretty low amount of exposure for the baby. Ahmad says that “though some data suggests that the risk of harm to the baby may be low, there is still overall limited data.”
Overall, people should talk to their health care provider about the risks and benefits of breastfeeding while on the medication.
“A lot of factors will need to be weighed, such as overall health of the infant, age of the infant, etc., when making this decision,” Furey says.
How much does Zurzuvae cost?
Zurzuvae’s price before insurance coverage is $15,900 for the 14-day treatment. However, the Policy Center for Maternal Mental Health says insurance companies and Medicaid are expected to cover it because it’s the only drug of its kind.
Less than 1 percent of U.S. insurers have issued coverage guidelines so far, so it’s still unknown how much it will cost patients after insurance. Some insurers require patients to try another antidepressant first (like the more common SSRIs) before covering Zurzuvae. For uninsured and underinsured people, Sage Therapeutics said it will offer copay assistance.
The hefty price tag and potential issues with coverage may widen existing health disparities, says Ahmad. “We need to ensure that we are seeking out solutions to enable wide-scale access to all PPD treatments so that people have access to whatever treatment may work best for them.”
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
For many who are suffering with prolonged grief, the holidays can be a time to reflect and find meaning in loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The holiday season is meant to be filled with joy, connection and celebration of rituals. Many people, however, are starkly reminded of their grief this time of year and of whom – or what – they have lost.
The added stress of the holiday season doesn’t help. Studies show that the holidays negatively affect many people’s mental health.
While COVID-19-related stressors may have lessened, the grief from change and loss that so many endured during the pandemic persists. This can cause difficult emotions to resurface when they are least expected.
I am a licensed therapist and trauma-sensitive yoga instructor. For the last 12 years, I’ve helped clients and families manage grief, depression, anxiety and complex trauma. This includes many health care workers and first responders who have recounted endless stories to me about how the pandemic increased burnout and affected their mental health and quality of life.
I developed an online program that research shows has improved their well-being. And I’ve observed firsthand how much grief and sadness can intensify during the holidays.
Post-pandemic holidays and prolonged grief
During the pandemic, family dynamics, close relationships and social connections were strained, mental health problems increased or worsened, and most people’s holiday traditions and routines were upended.
Those who lost a loved one during the pandemic may not have been able to practice rituals such as holding a memorial service, further delaying the grieving process. As a result, holiday traditions may feel more painful now for some. Time off from school or work can also trigger more intense feelings of grief and contribute to feelings of loneliness, isolation or depression.
Sometimes feelings of grief are so persistent and severe that they interfere with daily life. For the past several decades, researchers and clinicians have been grappling with how to clearly define and treat complicated grief that does not abate over time.
In March 2022, a new entry to describe complicated grief was added to the Diagnostic and Statistical Manual of Mental Disorders, or DSM, which classifies a spectrum of mental health disorders and problems to better understand people’s symptoms and experiences in order to treat them.
This newly defined condition is called prolonged grief disorder. About 10% of bereaved adults are at risk, and those rates appear to have increased in the aftermath of the pandemic.
People with prolonged grief disorder experience intense emotions, longing for the deceased, or troublesome preoccupation with memories of their loved one. Some also find it difficult to reengage socially and may feel emotionally numb. They commonly avoid reminders of their loved one and may experience a loss of identity and feel bleak about their future. These symptoms persist nearly every day for at least a month. Prolonged grief disorder can be diagnosed at least one year after a significant loss for adults and at least six months after a loss for children.
I am no stranger to complicated grief: A close friend of mine died by suicide when I was in college, and I was one of the last people he spoke to before he ended his life. This upended my sense of predictability and control in my life and left me untangling the many existential themes that suicide loss survivors often face.
How grieving alters brain chemistry
Research suggests that grief not only has negative consequences for a person’s physical health, but for brain chemistry too.
The feeling of grief and intense yearning may disrupt the neural reward systems in the brain. When bereaved individuals seek connection to their lost loved one, they are craving the chemical reward they felt before their loss when they connected with that person. These reward-seeking behaviors tend to operate on a feedback loop, functioning similar to substance addiction, and could be why some people get stuck in the despair of their grief.
One study showed an increased activation of the amygdala when showing death-related images to people who are dealing with complicated grief, compared to adults who are not grieving a loss. The amygdala, which initiates our fight or flight response for survival, is also associated with managing distress when separated from a loved one. These changes in the brain might explain the great impact prolonged grief has on someone’s life and their ability to function.
Recognizing prolonged grief disorder
Experts have developed scales to help measure symptoms of prolonged grief disorder. If you identify with some of these signs for at least one year, it may be time to reach out to a mental health professional.
Grief is not linear and doesn’t follow a timeline. It is a dynamic, evolving process that is different for everyone. There is no wrong way to grieve, so be compassionate to yourself and don’t make judgments on what you should or shouldn’t be doing.
Increasing your social supports and engaging in meaningful activities are important first steps. It is critical to address any preexisting or co-occurring mental health concerns such as anxiety, depression or post-traumatic stress.
It can be easy to confuse grief with depression, as some symptoms do overlap, but there are critical differences.
If you are experiencing symptoms of depression for longer than a few weeks and it is affecting your everyday life, work and relationships, it may be time to talk with your primary care doctor or therapist.
A sixth stage of grief
I have found that naming the stage of grief that someone is experiencing helps diminish the power it might have over them, allowing them to mourn their loss.
For decades, most clinicians and researchers have recognized five stages of grief: denial/shock, anger, depression, bargaining and acceptance.
But “accepting” your grief doesn’t sit well for many. That is why a sixth stage of grief, called “finding meaning,” adds another perspective. Honoring a loss by reflecting on its meaning and the weight of its impact can help people discover ways to move forward. Recognizing how one’s life and identity are different while making space for your grief during the holidays might be one way to soften the despair.
When my friend died by suicide, I found a deeper appreciation for what he brought into my life, soaking up the moments he would have enjoyed, in honor of him. After many years, I was able to find meaning by spreading mental health awareness. I spoke as an expert presenter for suicide prevention organizations, wrote about suicide loss and became certified to teach my local community how to respond to someone experiencing signs of mental health distress or crisis through Mental Health First Aid courses. Finding meaning is different for everyone, though.
Sometimes, adding a routine or holiday tradition can ease the pain and allow a new version of life, while still remembering your loved one. Take out that old recipe or visit your favorite restaurant you enjoyed together. You can choose to stay open to what life has to offer, while grieving and honoring your loss. This may offer new meaning to what – and who – is around you.
If you need emotional support or are in a mental health crisis, dial 988 or chat online with a crisis counselor.
Mandy Doria, Assistant Professor of Psychiatry, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: