Stop The World…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some news highlights from this week:
“US vs Them”?
With the US now set to lose its WHO membership, what does that mean for Americans? For most, the consequences will be indirect:
- the nation’s scientists and institutions will be somewhat “left out in the cold” when it comes to international scientific collaboration in the field of health
- the US will no longer enjoy a position of influence and power within the WHO, which organization’s reports and position statements have a lot of sway over the world’s health practices
Are there any benefits (of leaving the WHO) for Americans? Yes, there is one: the US will no longer be paying into the WHO’s budget, which means:
- the US will save the 0.006% of the Federal budget that it was paying into the WHO annually
- for the average American’s monthly budget, that means (if the saving is passed on) you’ll have an extra dime
However, since US scientific institutions will still need access to international data, likely that access will need to be paid separately, at a higher rate than US membership in WHO cost.
In short: it seems likely to go the way that Brexit did: “saving” on membership fees and then paying more for access to less.
Why is the US leaving again? The stated reasons were mainly twofold:
- the cost of US membership (the US’s contribution constituted 15% of the the overall WHO budget)
- holding the US’s disproportionately high COVID death rate (especially compared to countries such as China) to be a case of WHO mismanagement
Read in full: What losing WHO membership means for the U.S.
Related: What Would a Second Trump Presidency Look Like for Health Care? ← this was a speculative post by KFF Health News, last year
Halt, You’re Under A Breast
More seriously, this is about halting the metastasis of cancerous tumors in the breast. It is reasonable to expect the same principle and thus treatment may apply to other cancers too, but this is where the research is at for now (breast cancer research gets a lot of funding).
And, what principle and treatment is this, you ask? It’s about the foxglove-derived drug digoxin, and how it stops cancerous cells from forming clusters, and even actively dissolves clusters that have already formed. No clusters means no new tumors, which means no metastasis. No metastasis, in turn, means the cancer becomes much more treatable because it’s no longer a game of whack-a-mole; instead of spreading to other places, it’s a much more manageable case of “here’s the tumor, now let’s kill it with something”.
Note: yes, that does mean the tumor still needs killing by some other means—digoxin won’t do that, it “just” stops it from spreading while treatment is undertaken.
Read in full: Proof-of-concept study dissolves clusters of breast cancer cells to prevent metastases
Related: The Hormone Therapy That Reduces Breast Cancer Risk & More
Force Of Habit
“It takes 21 days to make a habit”, says popular lore. Popular is not, however, evidence-based:
❝This systematic review of 20 studies involving 2601 participants challenges the prevailing notion of rapid habit formation, revealing that health-related habits typically require 2–5 months to develop, with substantial individual variability ranging from 4 to 335 days. The meta-analysis demonstrated significant improvements in habit scores across various health behaviours, with key determinants including morning practices, personal choice, and behavioural characteristics❞
So, this is not a lottery, “maybe it will take until Tuesday, maybe it will take nearly a year”, so much as “there are important factors that seriously change how long a habit takes to become engrained, and here is what those factors are”.
Read in full: Study reveals healthy habits take longer than 21 days to set in
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
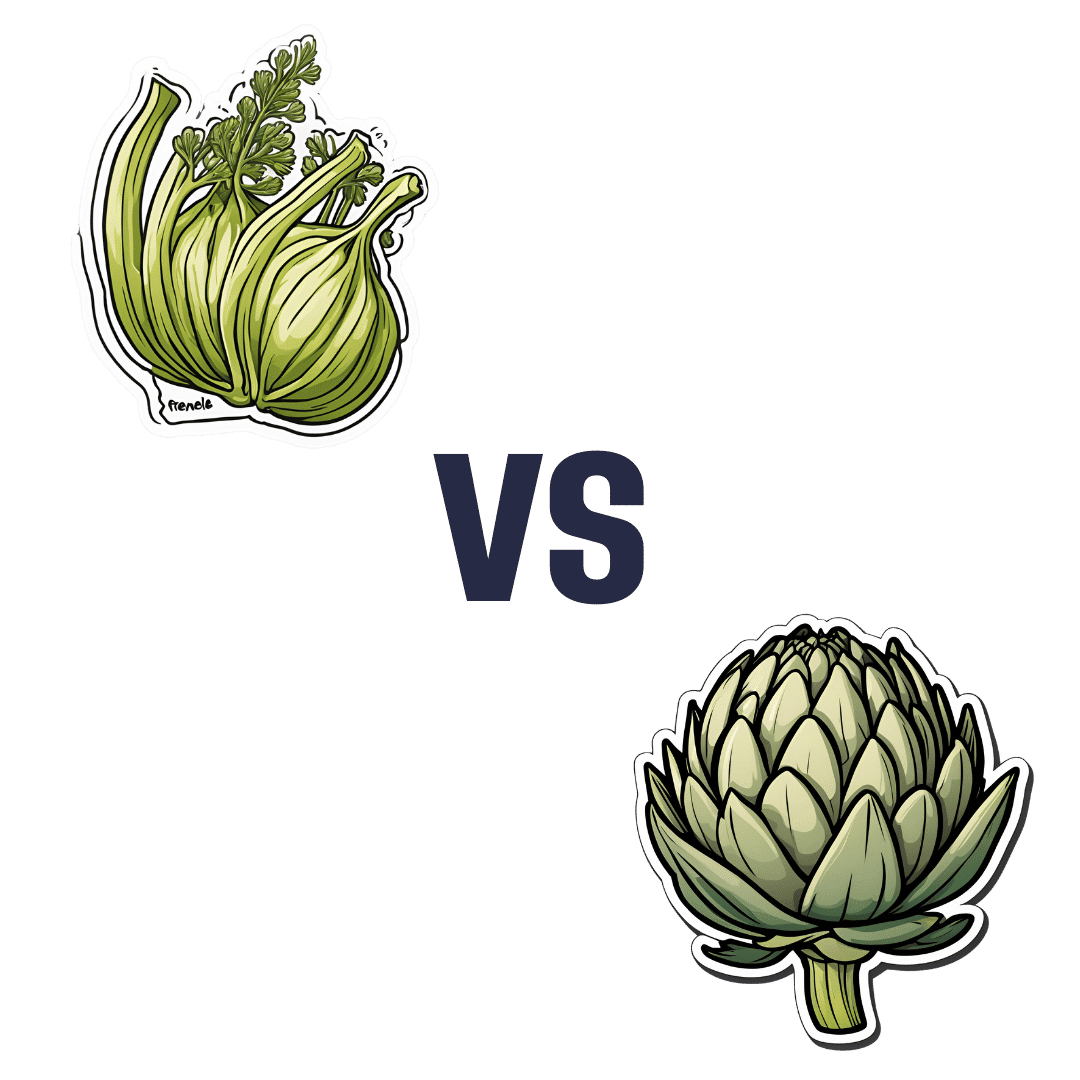
Fennel vs Artichoke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fennel to artichoke, we picked the artichoke.
Why?
Both are great! But artichoke wins on nutritional density.
In terms of macros, artichoke has more protein and more fiber, for only slightly more carbs.
Vitamins are another win for artichoke, boasting more of vitamins B1, B2, B3, B5, B6, B9, and choline. Meanwhile, fennel has more of vitamins A, E, and K, which is also very respectable but does allow artichoke a 6:3 lead.
In the category of minerals, artichoke has a lot more copper, iron, magnesium, manganese, and phosphorus, while fennel has a little more calcium, potassium, and selenium.
One other relevant factor is that fennel is a moderate appetite suppressant, which may be good or bad depending on your food-related goals.
All in all though, we say the artichoke wins by virtue of its greater abundance of nutrients!
Want to learn more?
You might like to read:
What Matters Most For Your Heart? ← appropriately enough, with fennel hearts and artichoke hearts!
Take care!
Share This Post
-
Hold Me Tight – by Dr. Sue Johnson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of relationship books are quite wishy-washy. This one isn’t.
This one is evidenced-based (and heavily referenced!), and yet at the same time as being deeply rooted in science, it doesn’t lose the human touch.
Dr. Johnson has spent her career as a clinical psychologist and researcher; she’s the primary developer of Emotionally Focused Therapy (EFT), which has demonstrated its effectiveness in over 35 years of peer-reviewed clinical research. In other words, it works.
EFT—and thus also this book—finds roots in Attachment Theory. As such, topics this book covers include:
- Recognizing and recovering from attachment injury
- How fights in a relationship come up, and how they can be avoided
- How lot of times relationships end, it’s not because of fights, but a loss of emotional connection
- Building a lifetime of love instead, falling in love again each day
This book lays the groundwork for ensuring a strong, secure, ongoing emotional bond, of the kind that makes/keeps a relationship joyful and fulfilling.
Dr. Johnson has been recognized in her field with a Lifetime Achievement Award, and the Order of Canada.
Share This Post
-
Walnut, Apricot, & Sage Nut Roast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to have at least one good nut roast recipe in your repertoire. It’s something that’s very good for making a good dish out of odds and ends that are in your house, and done well, it’s not only filling and nutritious, but a tasty treat too. Done badly, everyone knows the results can be unfortunate… Making this the perfect way to show off your skills!
You will need
- 1 cup walnuts
- ½ cup almonds
- ¼ cup whole mixed seeds (chia, pumpkin, & poppy are great)
- ¼ cup ground flax (also called flax meal)
- 1 medium onion, finely chopped
- 1 large carrot, grated
- 4 oz dried apricots, chopped
- 3 oz mushrooms, chopped
- 1 oz dried goji berries
- ½ bulb garlic, crushed
- 2 tbsp fresh sage, chopped
- 1 tbsp nutritional yeast
- 2 tsp dried rosemary
- 2 tsp dried thyme
- 2 tsp black pepper, coarse ground
- 1 tsp yeast extract (even if you don’t like it; trust us; it will work) dissolved in ¼ cup hot water
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃, and line a 2 lb loaf tin with baking paper.
2) Heat some oil in a skillet over a moderate heat, and fry the onion for a few minutes until translucent. Add the garlic, carrot, and mushrooms, cooking for another 5 minutes, stirring well. Set aside to cool a little once done.
3) Process the nuts in a food processor, pulsing until they are well-chopped but not so much that they turn into flour.
4) Combine the nuts, vegetables, and all the other ingredients in a big bowl, and mix thoroughly. If it doesn’t have enough structural integrity to be thick and sticky and somewhat standing up by itself if you shape it, add more ground flax. If it is too dry, add a little water but be sparing.
5) Spoon the mixture into the loaf tin, press down well (or else it will break upon removal), cover with foil and bake for 30 minutes. Remove the foil, and bake for a further 15 minutes, until firm and golden. When done, allow it to rest in the tin for a further 15 minutes, before turning it out.
6) Serve, as part of a roast dinner (roast potatoes, vegetables, gravy, etc).
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Chia Seeds vs Pumpkin Seeds – Which is Healthier?
- Apricots vs Peaches – Which is Healthier?
- Goji Berries: Which Benefits Do They Really Have?
- Ergothioneine: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Share This Post
Related Posts
-
The Fiber Fueled Cookbook – by Dr. Will Bulsiewicz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bulsiewicz’s book “Fiber Fuelled” (which is great), but this one is more than just a cookbook with the previous book in mind. Indeed, this is even a great stand-alone book by itself, since it explains the core principles well enough already, and then adds to it.
It’s also about a lot more than just “please eat more fiber”, though. It looks at FODMAPs, purine, histamine intolerance, celiac disease, altered gallbladder function, acid reflux, and more.
He offers a five-part strategy:
Genesis (what is the etiology of your problem)
- Restrict (cut things out to address that first)
- Observe (keep a food/symptom diary)
- Work things back in (re-add potential triggers one by one, see how it goes)
- Train your gut (your microbiome does not exist in a vacuum, and communication is two-way)
- Holistic healing (beyond the gut itself, looking at other relevant factors and aiming for synergistic support)
As for the recipes themselves, there are more than a hundred of them and they are good, so no more “how can I possibly cook [favorite dish] without [removed ingredient]?”
Bottom line: if you’d like better gut health, this book is a top-tier option for fixing existing complaints, and enjoying plain-sailing henceforth.
Click here to check out The Fiber Fueled Cookbook; your gut will thank you later!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Green Paneer Flatbreads
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These are versatile little snacks that can be eaten alone or served as part of a buffet; great for warm summer nights!
You will need
- 1 lb block of paneer (you can also use our plant-based high-protein paneer recipe)
- 7 oz unsweetened yogurt (your choice what kind; plant-based is fine; live cultured is best)
- 1 tomato, thinly sliced
- ½ red onion, thinly sliced
- 2 oz spinach leaves
- 1 tbsp lime juice
- 1 tsp red chili powder
- 4 wholewheat flatbreads
And then the marinade:
- 3 oz spinach
- ½ bulb garlic
- 1 tsp cumin seeds
- 1 tsp coriander seeds
- 1 tsp chili flakes
- ½ tsp MSG or 1 tsp low-sodium salt (MSG being the preferable and healthier option)
- 2 tbsp extra virgin olive oil
- Juice of ½ lime
Method
(we suggest you read everything at least once before doing anything)
1) Blend the marinade ingredients in a blender.
2) Cut the paneer into long cuboid chapes (similar to fish fingers) and put them in a bowl. Pour ⅔ of the marinade over them, and gently mix to coat evenly.
3) Heat a ridged griddle pan, and when hot, add the paneer and cook for 1–2 minutes each side without stirring, jiggling, or doing anything other than turning once per uncooked side.
4) Combine the onion, tomato, spinach leaves, lime choice, and chili powder to make the salad.
5) Add the remaining marinade to the yogurt to make a green dip.
6) Toast your flatbreads under the grill.
5) Assemble, putting the paneer and salad with a spoonful of the dip on the flatbread, and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- High-Protein Plant-Based Paneer
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Natural Facelift – by Sophie Perry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book isn’t: it’s mostly not about beauty, and it’s certainly not about ageist ideals of “hiding” aging.
The author herself discusses the privilege that is aging (not everyone gets to do it) and the importance of taking thankful pride in our lived-in bodies.
The title and blurb belie the contents of the book rather. Doubtlessly the publisher felt that extrinsic beauty would sell better than intrinsic wellbeing. As for what it’s actually more about…
Ever splashed your face in cold water to feel better? This book’s about revitalising the complex array of facial muscles (there are anatomical diagrams) and the often-tired and very diverse tissues that cover them, complete with the array of nerve endings very close to your CNS (not to mention the vagus nerve running just behind your jaw), and some of the most important blood vessels of your body, serving your brain.
With all that in mind, this book, full of useful therapeutic techniques, is a very, very far cry from “massage like this and you’ll look like you got photoshopped”.
The style varies, as some parts of explanation of principles, or anatomy, and others are hands-on (literally) guides to the exercises, but it is all very clear and easy to understand/follow.
Bottom line: aspects of conventional beauty may be a side-effect of applying the invigorating exercises described in this book. The real beauty is—literally—more than skin-deep.
Click here to check out The Natural Facelift, and order yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: