The Minimum Method – by Joey Thurman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Trying to squeeze out an extra 0.5% from every effort in life can be exhausting, especially with diminishing marginal returns when it comes to linear increases in effort.
Surely there must be a sweet spot of getting the best returns on the least effort and call it a day?
That’s what this book is about. Thurman examines and explains how to get “the most for least” in various important areas of health, including diet, exercise, sleep, breathwork, recovery, and a chapter specifically on brain health, though of course all the aforementioned things do affect brain health too.
An interesting feature of the book is that at the end of each chapter, he’ll give different advice for different levels of experience/commitment, so that essentially there’s an easy/medium/hard way to proceed each time.
The style is light and personal, without much hard science. The advice given is nonetheless consistent with prevailing scientific consensus, and there are still occasional scientific references throughout, with links to appropriate studies. Mostly though, the focus is on being practical.
Bottom line: if you’ve been looking for a “most for least” way of going about health, this is a fine option.
Click here to check out The Minimum Method, and enjoy benefits disproportionate to your effort!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Plant-Based Diet Revolution – by Dr. Alan Desomond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is this just another gut-healthy cooking guide? Not entirely…
For a start, it’s not just about giving you a healthy gut; it also covers a healthy heart and a healthy brain. There’s lots of science in here!
It’s also aimed as a transitional guide to eating more plants and fewer animal products, if you so choose. And if you don’t so choose, at least having the flexibility to cook both ways.
The recipes themselves (organized into basics, breakfasts, lunches, mains, desserts) are clear and easy while also being calculated to please readers (and their families) who are used to eating more meat. There are, for instance, plenty of healthy proteins, healthy fats, and comfort foods.
The “28 days” of the title refers to a meal plan using the recipes from the book; it’s not a big feature of the book though, so use it or don’t, but the cooking advice itself is more than worth the price of the book and the recipes are certainly great.
Bottom line: if you’re thinking of taking a “Meatless Mondays” approach to making your diet healthier, this book can help you do that in style!
Click here to check out The Plant-Based Diet Revolution, and upgrade your culinary repertoire!
Share This Post
-
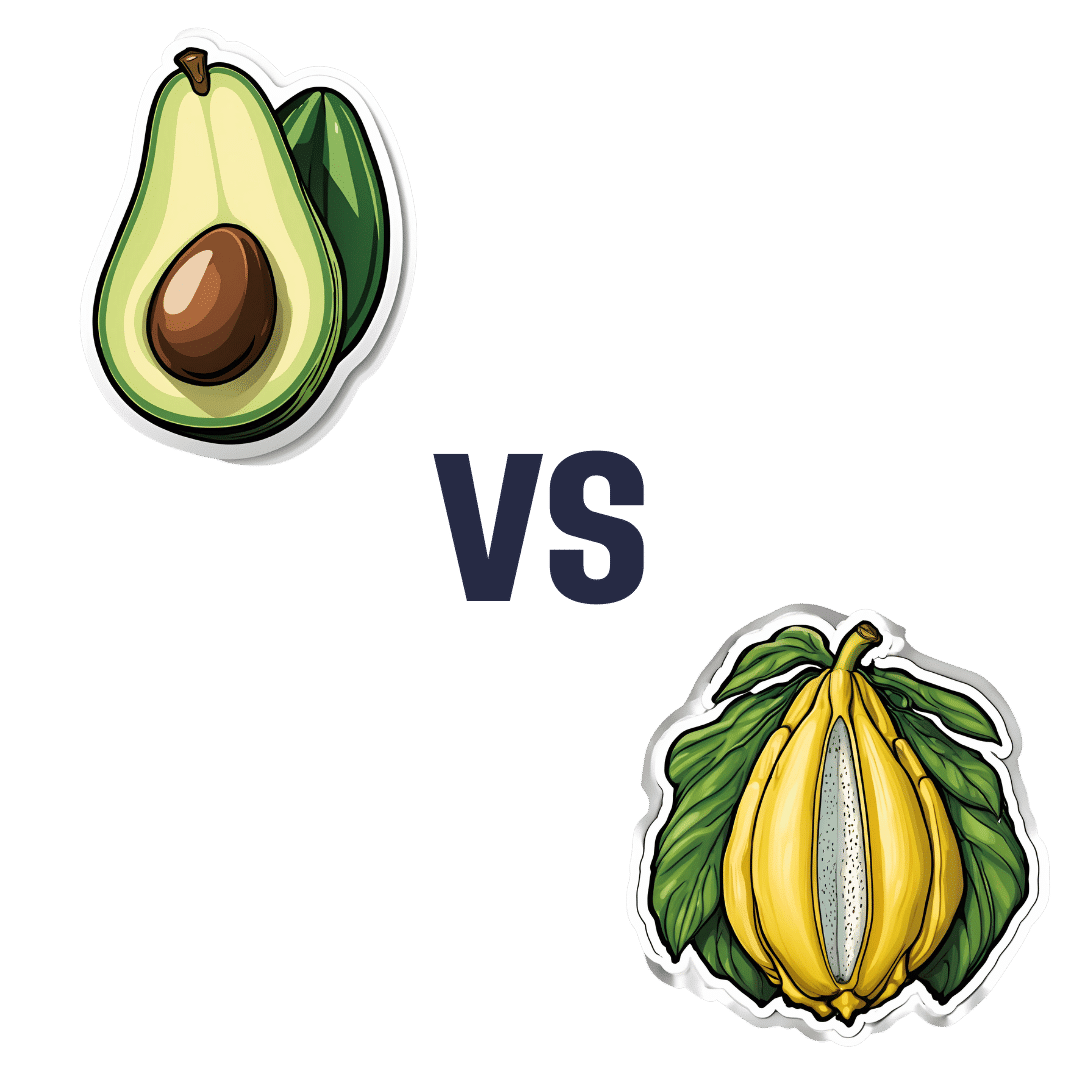
Avocado vs Jackfruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to jackfruit, we picked the avocado.
Why?
In terms of macros, avocado is higher in fats (famously healthy ones, including a good dose of omega-3), fiber (nearly 5x more), and protein (despite jackfruit being more often used as a meaty element in recipes, avocado has slightly more). Meanwhile, jackfruit is about 3x higher in carbs. All in all, a clear win for avocado.
Looking at vitamins, avocado has more of vitamins A, B2, B3, B5, B7, B9, E, K, and choline, while jackfruit has more of vitamins B1, B6, and C. Another win for avocado in this category.
In the category of minerals, avocado has more copper, iron, manganese, phosphorus, potassium, selenium, and zinc, while jackfruit has more calcium. One more win for avocado.
Adding up the sections makes for an easy overall win for avocado, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Jackfruit vs Durian – Which is Healthier? ← including some fun durian facts (such as how to pick a good one, and what happens if you eat durian and drink alcohol)
Enjoy!
Share This Post
-
52 Weeks to Better Mental Health – by Dr. Tina Tessina
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about the health benefits of journaling, but how to get started, and how to make it a habit, and what even to write about?
Dr. Tessina presents a year’s worth of journaling prompts with explanations and exercises, and no, they’re not your standard CBT flowchart things, either. Rather, they not only prompt genuine introspection, but also are crafted to be consistently uplifting—yes, even if you are usually the most disinclined to such positivity, and approach such exercises with cynicism.
There’s an element of guidance beyond that, too, and as such, this book is as much a therapist-in-a-book as you might find. Of course, no book can ever replace a competent and compatible therapist, but then, competent and compatible therapists are often harder to find and can’t usually be ordered for a few dollars with next-day shipping.
Bottom line: if undertaken with seriousness, this book will be an excellent investment in your mental health and general wellbeing.
Click here to check out 52 Weeks to Better Mental Health, and get on the best path for you!
Share This Post
Related Posts
-
The Power of Fun – by Catherine Price
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s said that nobody’s dying regret is to wish they’d spent more time at the office, yet many of don’t make enough time for fun.
This book has been published with two different subtitles:
- Why fun is the key to a happy and healthy life
- How to feel alive again
One offers a sensible reason to read this book; the other offers a deeply emotional reason. Both are entirely valid.
Catherine Price sets out in this work to identify what fun actually is (she puts it at the intersection of playfulness, connection and flow) and how to have more of it (she gives a five-step method to build and integrate it into life).
In the category of criticism, this 334-page book is (in this reviewer’s opinion) a little padded and could have been an article instead. But the advice contained within it is sound, and the impact it can have might be profound.
Bottom line: if you find you’ve settled into a routine that’s perhaps comfortable, but not actually that much fun, this book will help you to liven things up.
Click here to check out The Power Of Fun, and feel more alive!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pistachios vs Pine Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to pine nuts, we picked the pistachios.
Why?
First looking at the macros, pistachios have nearly 2x the protein while pine nuts have nearly 2x the fat. The fats are healthy in moderation (mostly polyunsaturated, a fair portion of monounsaturated, and a little saturated), but we’re going to value the protein content higher. Also, pistachios have approximately 2x the carbs, and/but nearly 3x the fiber. All in all, we’ll call this section a moderate win for pistachios.
When it comes to vitamins, pistachios have more of vitamins A, B1, B5, B6, B9, and C, while pine nuts have more of vitamins B2, B3, E, K, and choline. All in all, pistachios are scraping a 6:5 win here, or we could call it a tie if we want to value pine nuts’ vitamins more (due to the difference in how many foods each vitamin is found in, and thus the likelihood of having a deficiency or not).
In the category of minerals, pistachios have more calcium, copper, potassium, and selenium, while pine nuts have more iron, magnesium, manganese, and zinc. This would be a tie if we just call it 4:4, but what’s worth noting is that while both of these nuts are a good source of most of the minerals mentioned, pine nuts aren’t a very good source of calcium or selenium, so we’re going to declare this section a very marginal win for pistachios.
Adding up the moderate win, the scraped win, and the barely scraped win, all adds up to a win for pistachios. However, as you might have noticed, both are great so do enjoy both if you can!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: