Can you die from long COVID? The answer is not so simple
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nearly five years into the pandemic, COVID is feeling less central to our daily lives.
But the virus, SARS-CoV-2, is still around, and for many people the effects of an infection can be long-lasting. When symptoms persist for more than three months after the initial COVID infection, this is generally referred to as long COVID.
In September, Grammy-winning Brazilian musician Sérgio Mendes died aged 83 after reportedly having long COVID.
Australian data show 196 deaths were due to the long-term effects of COVID from the beginning of the pandemic up to the end of July 2023.
In the United States, the Centers for Disease Control and Prevention reported 3,544 long-COVID-related deaths from the start of the pandemic up to the end of June 2022.
The symptoms of long COVID – such as fatigue, shortness of breath and “brain fog” – can be debilitating. But can you die from long COVID? The answer is not so simple.

How could long COVID lead to death?
There’s still a lot we don’t understand about what causes long COVID. A popular theory is that “zombie” virus fragments may linger in the body and cause inflammation even after the virus has gone, resulting in long-term health problems. Recent research suggests a reservoir of SARS-CoV-2 proteins in the blood might explain why some people experience ongoing symptoms.
We know a serious COVID infection can damage multiple organs. For example, severe COVID can lead to permanent lung dysfunction, persistent heart inflammation, neurological damage and long-term kidney disease.
These issues can in some cases lead to death, either immediately or months or years down the track. But is death beyond the acute phase of infection from one of these causes the direct result of COVID, long COVID, or something else? Whether long COVID can directly cause death continues to be a topic of debate.
Of the 3,544 deaths related to long COVID in the US up to June 2022, the most commonly recorded underlying cause was COVID itself (67.5%). This could mean they died as a result of one of the long-term effects of a COVID infection, such as those mentioned above.
COVID infection was followed by heart disease (8.6%), cancer (2.9%), Alzheimer’s disease (2.7%), lung disease (2.5%), diabetes (2%) and stroke (1.8%). Adults aged 75–84 had the highest rate of death related to long COVID (28.8%).
These findings suggest many of these people died “with” long COVID, rather than from the condition. In other words, long COVID may not be a direct driver of death, but rather a contributor, likely exacerbating existing conditions.

‘Cause of death’ is difficult to define
Long COVID is a relatively recent phenomenon, so mortality data for people with this condition are limited.
However, we can draw some insights from the experiences of people with post-viral conditions that have been studied for longer, such as myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS).
Like long COVID, ME/CFS is a complex condition which can have significant and varied effects on a person’s physical fitness, nutritional status, social engagement, mental health and quality of life.
Some research indicates people with ME/CFS are at increased risk of dying from causes including heart conditions, infections and suicide, that may be triggered or compounded by the debilitating nature of the syndrome.
So what is the emerging data on long COVID telling us about the potential increased risk of death?
Research from 2023 has suggested adults in the US with long COVID were at greater risk of developing heart disease, stroke, lung disease and asthma.
Research has also found long COVID is associated with a higher risk of suicidal ideation (thinking about or planning suicide). This may reflect common symptoms and consequences of long COVID such as sleep problems, fatigue, chronic pain and emotional distress.
But long COVID is more likely to occur in people who have existing health conditions. This makes it challenging to accurately determine how much long COVID contributes to a person’s death.
Research has long revealed reliability issues in cause-of-death reporting, particularly for people with chronic illness.

So what can we conclude?
Ultimately, long COVID is a chronic condition that can significantly affect quality of life, mental wellbeing and overall health.
While long COVID is not usually immediately or directly life-threatening, it’s possible it could exacerbate existing conditions, and play a role in a person’s death in this way.
Importantly, many people with long COVID around the world lack access to appropriate support. We need to develop models of care for the optimal management of people with long COVID with a focus on multidisciplinary care.
Dr Natalie Jovanovski, Vice Chancellor’s Senior Research Fellow in the School of Health and Biomedical Sciences at RMIT University, contributed to this article.
Rose (Shiqi) Luo, Postdoctoral Research Fellow, School of Health and Biomedical Sciences, RMIT University; Catherine Itsiopoulos, Professor and Dean, School of Health and Biomedical Sciences, RMIT University; Kate Anderson, Vice Chancellor’s Senior Research Fellow, RMIT University; Magdalena Plebanski, Professor of Immunology, RMIT University, and Zhen Zheng, Associate Professor, STEM | Health and Biomedical Sciences, RMIT University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Brain Health Action Plan – by Dr. Teryn Clarke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is a physician and neurologist, and she brings a lot of science with her when she sets out to Alzheimer’s-proof our brains:
- She talks about brain nourishment, and what things in contrast sabotage our brains, and how.
- She talks intermittent fasting, and optimal scheduling when it comes to food, sleep, exercise, and more.
- She talks about how the rest of our health affects our brain health, and vice versa.
The “action plan” promised by the title includes all of those elements, plus such matters as ongoing education, cognitive stimulation, stress management, dealing with depression, and other mostly-brain-based factors.
As such, it’s not just a “for your information” book, and Dr. Clarke does outline suggested goals, tasks, and habits, advises the use of a streak tracker, provides suggested recipes, and in all ways does what she can to make it easy for the reader to implement the information within.
Bottom line: if you’d like to dodge dementia, this book is quite a comprehensive guide.
Click here to check out Brain Health Action Plan, and enact yours!
Share This Post
-
Are Squats the Ultimate Game-Changer?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Jess Grochowsky, PT, DPT, MTC, CLT, CMPTP, says the answer is yes, and here’s why:
The most complete exercise
Squats are a powerful full-body exercise that targets legs, core, and (when weights are used) upper body. All in all, they enhance strength, mobility, metabolism, and joint health, making them essential for longevity and maintaining quality of movement throughout life.
In particular, they allow a much greater range of movement through more dimensions than most exercises do, meaning that (unlike a lot of more linear exercises) they build functional strength that sees us well in everyday life—mobility, joint control, and muscle stability.
Proper Squat Technique:
- The squat involves lowering the center of mass (which is slightly behind your navel and slightly down; exact position depends on your body composition and proportions) toward the floor.
- Use the “head to hips” principle to maintain a straight spine: as the head moves forward, the hips go back.
- Different foot positions (sumo, narrow, etc) target various muscles.
4 key variables to adjust squats:
- Base of support: the surface you stand on (firm vs unstable like a Bosu ball) affects stability and muscle engagement.
- Foot position: wide stances increase stability and target inner thighs and glutes; narrow stances focus more on quads.
- Weights: can use free weights, kettlebells, or bars. Adding weights increases intensity and can incorporate upper body exercises (e.g. bicep curls, overhead presses, etc).
- Squat depth: ranges from partial to deep squats, depending on functional goals.
Types of squats and variations given in the video:
- Firm surface squats: provide stability and allow even weight distribution.
- Unstable surface squats: engage smaller stabilizing muscles.
- Yoga ball squats: shift the center of mass backward, increasing quad and glute activation.
- Weighted squats: add resistance to increase muscle load and core stability (e.g. one-sided weights for oblique engagement).
- Dynamic weighted squats: incorporate quick movements, like kettlebell swings, for power and coordination.
- Single-leg squats: enhance balance and increase workload on one side of the body.
For more on all of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
The Sucralose News: Scaremongering Or Serious?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the news on sucralose?
These past days the press has been abuzz with frightening tales:
- This Common Artificial Sweetener Can Break Down DNA, Scientists Warn
- Sucralose Damages DNA, Linked to Leaky Gut
- Chemical found in common sweetener damages DNA
- Chemical found in widely used sweetener breaks up DNA
- Chemical from Splenda breaks up DNA
How true and/or serious is this?
Firstly, let’s manage expectations. Pineapple juice also breaks down DNA, but is not generally considered a health risk. So let’s keep that in mind, while we look into the science.
Is sucralose as scary as pineapple juice, or is it something actually dangerous?
The new study (that sparked off these headlines)
The much-referenced study is publicly available to read in full—here it is:
You may notice that this doesn’t have quite the snappy punchiness of some of the headlines, but let’s break this down, if you’ll pardon the turn of phrase:
- Toxicological: pertaining to whether or not it has toxic qualities
- Pharmacokinetic: the science of asking, of chemicals in bodies, “where did it come from; where did it go; what could it do there; what can we know?”
- Sucralose-6-acetate: an impurity that can be found in sucralose. For perspective, the study found that the sucralose in Splenda contained “up to” 0.67% sucralose-6-acetate.
- Sucralose: a modified form of sucrose, that makes it hundreds of times sweeter, and non-caloric because the body cannot break it down so it’s treated as a dietary fiber and just passes through
- In vitro: things are happening in petri dishes, not in animals (human or otherwise), which would be called “in vivo”
- Screening assays: “we set up a very closed-parameters chemical test, to see what happens when we add this to this” ⇽ oversimplification, but this is the basic format of a screening assay
Great, now we understand the title, but what about the study?
Researchers looked primarily at the effects of sucralose-6-acetate and sucralose (together and separately) on epithelial cells (these are very simple cells that are easy to study; conveniently, they are also most of what makes up our intestinal walls). For this, they used a fancy way of replicating human intestinal walls, that’s actually quite fascinating but beyond the scope of today’s newsletter. Suffice it to say: it’s quite good, and/but has its limitations too. They also looked at some in vivo rat studies.
What they found was…
Based on samples from the rat feces (somehow this didn’t make it into the headlines), it appears that sucralose may be acetylated in the intestines. What that means is that we, if we are like the rats (definitely not a given, but a reasonable hypothesis), might convert up to 10% of sucralose into sucralose-6-acetate inside us. Iff we do, the next part of the findings become more serious.
Based on the in vitro simulations, both sucralose and sucralose-6-acetate reduced intestinal barrier integrity at least a little, but sucralose-6-acetate was the kicker when it came to most of the effects—at least, so we (reasonably!) suppose.
Basically, there’s a lot of supposition going on here but the suppositions are reasonable. That’s how science works; there’s usually little we can know for sure from a single study; it’s when more studies roll in that we start to get a more complete picture.
What was sucralose-6-acetate found to do? It increased the expression of genes associated with inflammation, oxidative stress, and cancer (granted those three things generally go together). So that’s a “this probably has this end result” supposition.
More concretely, and which most of the headlines latched onto, it was found (in vitro) to induce cytogenic damage, specifically, of the clastogenic variety (produces DNA strand breaks—so this is different than pineapple’s bromelain and DNA-helicase’s relatively harmless unzipping of genes).
The dose makes the poison
So, how much is too much and is that 0.67% something to worry about?
- Remembering the rat study, it may be more like 10% once our intestines have done their thing. Iff we’re like rats.
- But, even if it’s only 0.67%, this will still be above the “threshold of toxicological concern for genotoxicity”, of 0.15µg/person/day.
- On the other hand, the fact that these were in vitro studies is a serious limitation.
- Sometimes something is very dangerous in vitro, because it’s being put directly onto cells, whereas in vivo we may have mechanisms for dealing with that.
We won’t know for sure until we get in vivo studies in human subjects, and that may not happen any time soon, if ever, depending on the technical limitations and ethical considerations that sometimes preclude doing certain studies in humans.
Bottom line:
- The headlines are written to be scary, but aren’t wrong; their claims are fundamentally true
- What that means for us as actual humans may not be the same, however; we don’t know yet
- For now, it is probably reasonable to avoid sucralose just in case
Share This Post
Related Posts
-
Cherries vs Elderberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to elderberries, we picked the elderberries.
Why?
Both are great! But putting them head-to-head…
In terms of macros, cherries have slightly more protein (but we are talking miniscule numbers here, 0.34mg/100g), while elderberries have moderately more carbs and more than 4x the fiber. This carbs:fiber ratio difference means that elderberries have the lower glycemic index by far, as well as simply more grams/100g fiber, making this an easy win for elderberries.
In the category of vitamins, cherries have more of vitamins A, B9, E, K, and choline, while elderberries have more of vitamins B1, B2, B3, B6, and C. The margins of difference mean that elderberries have the very slightly better overall vitamin coverage, but it’s so slight that we’ll call this a 5:5 tie.
When it comes to minerals, cherries have more copper, magnesium, and manganese, while elderberries have more calcium, iron, phosphorus, potassium, selenium, and zinc. A nice easy win to top it off for elderberries.
On the polyphenols (and other phytochemicals) front, both are great in different ways, nothing that’d we’d consider truly sets one ahead of the other.
All in all, adding up the sections, an overall win for elderberries, but by all means enjoy either or both!
Want to learn more?
You might like to read:
- Cherries’ Very Healthy Wealth Of Benefits!
- Herbs for Evidence-Based Health & Healing ← one of them is elderberry, which hastens recovery from upper respiratory viral infections 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 10 Causes Of High Blood Pressure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As Dr. Frita Fisher explains, these are actually the top 10 known causes of high blood pressure. Number zero on the list would be “primary hypertension”, which means high blood pressure with no clear underlying cause.
Superficially, this feels a little like the sometime practice of writing the catch-all “heart failure” as the cause of death on a death certificate, because yes, that heart sure did stop beating. But in reality, primary hypertension is most likely often caused by such things as unmanaged chronic stress—something that doesn’t show up on most health screenings.
Dr. Fisher’s Top 10
- Thyroid disease: both hyperthyroidism and hypothyroidism can cause high blood pressure.
- Obstructive sleep apnea: characterized by snoring, daytime sleepiness, and headaches, this condition can lead to hypertension.
- Chronic kidney disease: diseases ranging from diabetic nephropathy to renal vascular disease can cause high blood pressure.
- Elevated cortisol levels: conditions like Cushing’s syndrome or disease, which involve high cortisol levels, can lead to hypertension—as can a lifestyle with a lot of chronic stress, but that’s less readily diagnosed as such than something one can tell from a blood test.
- Elevated aldosterone levels: excess aldosterone from the adrenal glands causes the body to retain salt and water, increasing blood pressure, because more stuff = more pressure.
- Brain tumor: tumors that increase intracranial pressure can cause a rise in blood pressure to ensure adequate brain perfusion. In these cases, the hypertension is keeping you alive—unless it kills you first. If this seems like a strange bodily response, remember that our bodily response to an infection is often fever, to kill off the infection which can’t survive at such high temperatures (but neither can we, so it becomes a game of chicken with our life on the line), so sometimes our body does kill us with one thing while trying to save us from another.
- Coarctation of the aorta: this congenital heart defect results in narrowing of the aorta, leading to hypertension, especially in the upper body.
- Pregnancy: pregnancy can either induce or worsen existing hypertension.
- Obesity: excess weight increases blood flow and pressure on arteries, raising the risk of hypertension and associated conditions, e.g. diabetes etc.
- Drugs: certain medications and recreational drugs (including, counterintuitively, alcohol!) can elevate blood pressure.
For more information on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Hypertension: Factors Far More Relevant Than Salt
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
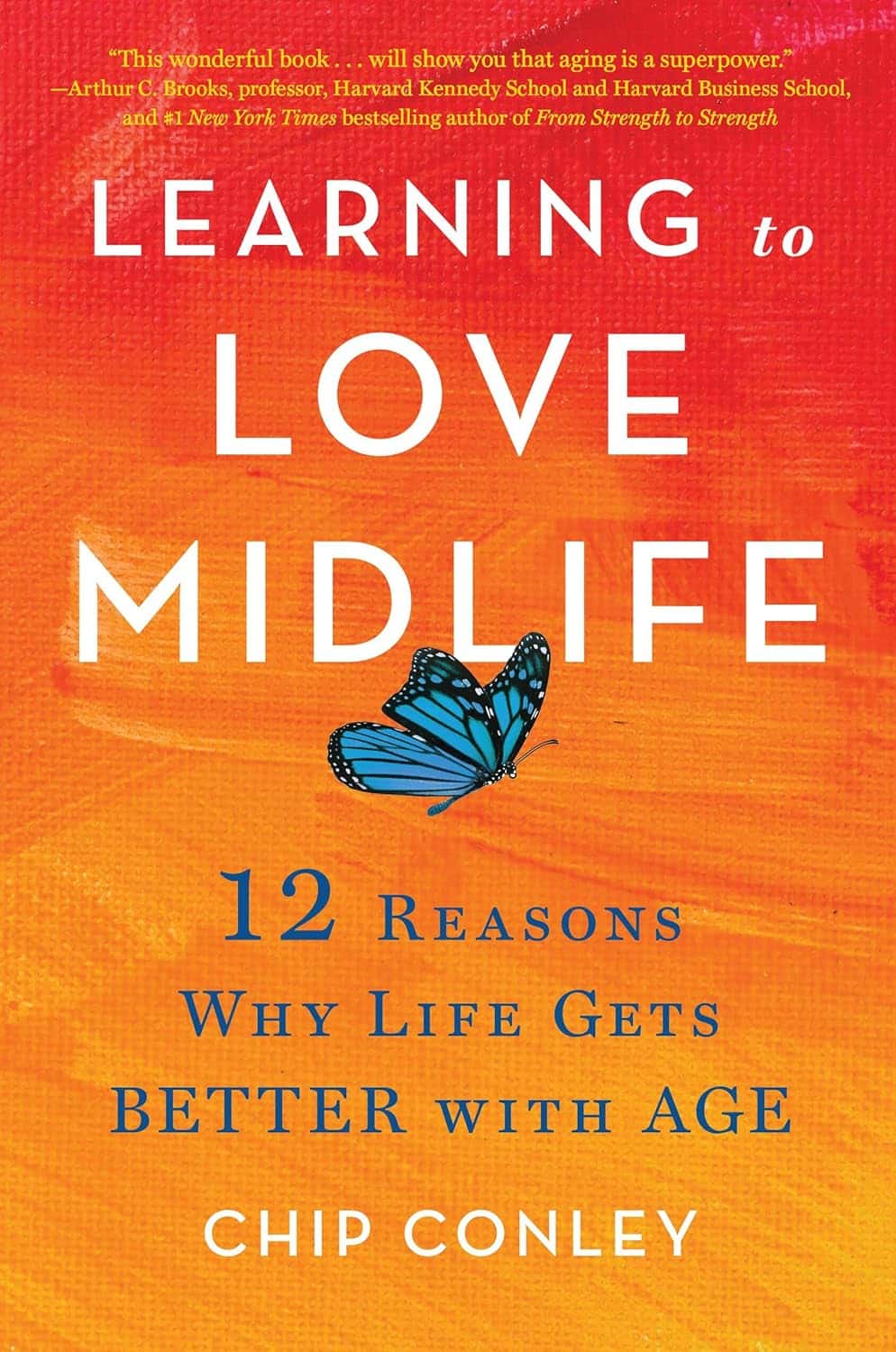
Learning to Love Midlife – by Chip Conley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While the book is titled about midlife, it could have said: midlife and beyond.
Some of the benefits discussed in this book really only kick in during one’s 50s, 60s, or 70s, usually. Which, for all but the most optimistic, is generally considered to be stretching beyond what is usually called “midlife”.
However! Chip Conley makes the argument for midlife being anywhere from one’s early 30s to mid-70s, depending on what (and how) we’re doing in life.
He talks about (as the subtitle promises) 12 reasons life gets better with age, and those reasons are grouped into 5 categories, thus:
- Physical life
- Emotional life
- Mental life
- Vocational life
- Spiritual life
It may surprise some readers that there are physical benefits that come with aging, but we do get two chapters in that category.
The writing style is very casual, yet with references to science throughout, and a bibliography for such.
Bottom line: if you’d like to make sure you’re making the most of your midlife and beyond, this a book that offers a lot of guidance on doing so!
Click here to check out Learning to Love Midlife, and age in style!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: