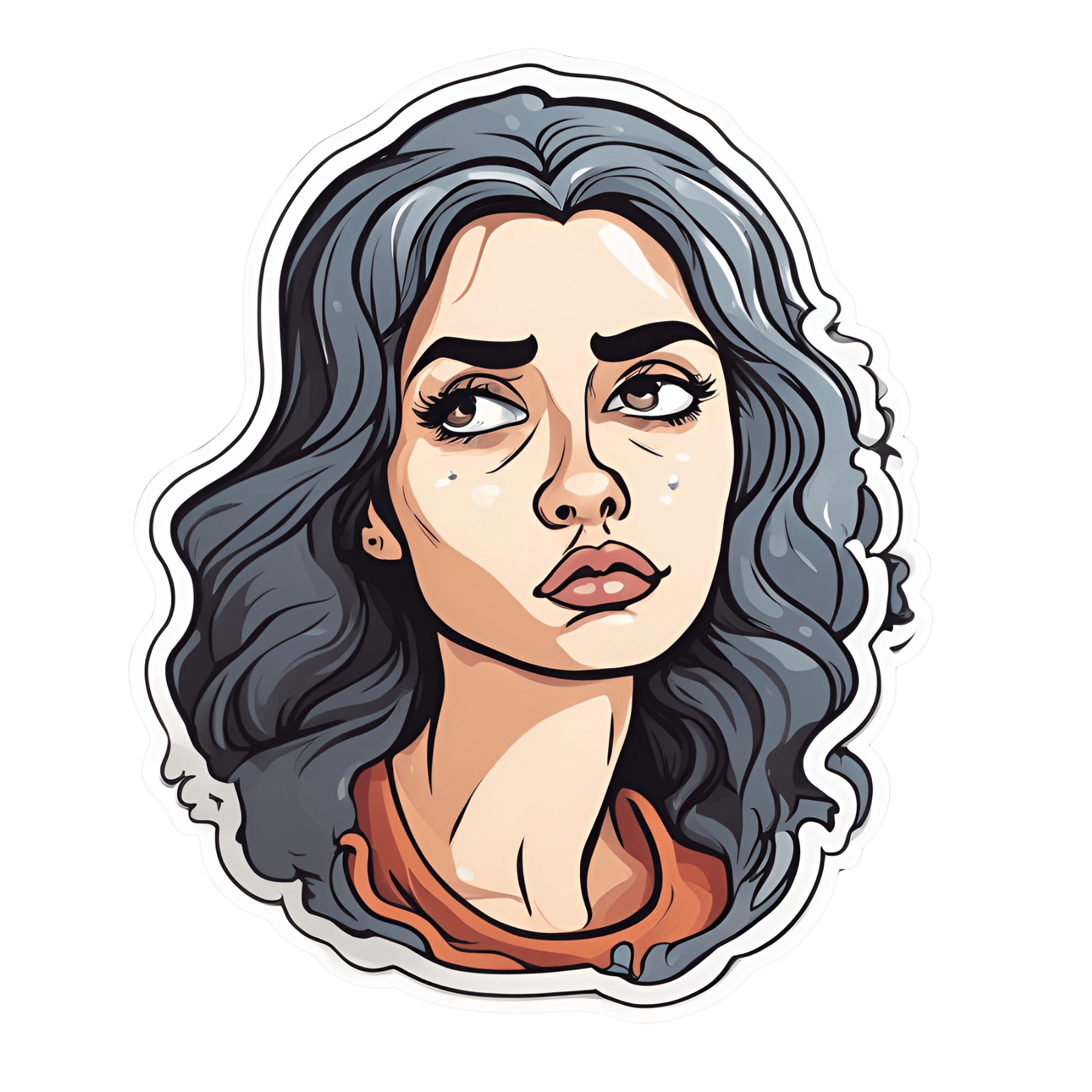
How To Survive A Heart Attack When You’re Alone
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Alan Mandel emphasizes the importance of staying calm and following these steps to improve survival chances:
Simple is best
Here’s how you will survive a heart attack alone: briefly.
So, you will need to get help as quickly as possible. 90% of people who make it to a hospital alive, go on to survive their heart attack, so that’s your top priority.
Call emergency services as soon as you suspect you are having a heart attack. Stay on the line, and stay calm.
While having a heart attack is not an experience that’s very conducive to relaxation, heightened emotions will exacerbate things, so focus on breathing calmly. One of the commonly reported symptoms of heart attack that doesn’t often make it to official lists is “a strong sense of impending doom”, and that is actually helpful as it helps separate it from “is this indigestion?” or such, but once you have acknowledged “yes, this is probably a heart attack”, you need to put those feelings aside for later.
If you have aspirin available, Dr. Mandel says that the time to take it is once you have called an ambulance. However, if aspirin is not readily available, do not exert yourself trying to find some; indeed, don’t move more than necessary.
Do not drive yourself to hospital; it will increase the risk of fainting, and you may crash.
While you are waiting, your main job is to remain calm; he recommends deep breathing, and lying with knees elevated or feet on a chair; this latter is to minimize the strain on your heart.
For more on all this, plus the key symptoms and risk factors, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Heart Attack: His & Hers (Be Prepared!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antioxidant Matcha Snack Bars
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The antioxidants in this come not just from the matcha, but also the cacao nibs and chocolate, as well as lots of nutrients from the hazelnuts and cashews. If you’re allergic to nuts, we’ll give you substitutions that will change the nutritional profile (and flavor), but still work perfectly well and be healthy too.
You will need
For the base:
- ⅔ cup roasted hazelnuts (if allergic, substitute dessicated coconut)
- ⅔ cup chopped dates
For the main part:
- 1 cup raw cashews (if allergic, substitute raw coconut, chopped)
- ½ cup almond milk (or your preferred milk of any kind)
- ½ cup cacao nibs
- 2 tbsp lime juice
- 1 tbsp matcha powder
- 1 tbsp maple syrup (omit if you don’t care for sweetness)
For the topping (optional):
- 2oz dark chocolate, melted (and if you like, tempered—but this isn’t necessary; it’ll just make it glossier if you do)
- Spare cacao nibs, chopped nuts, or anything else you might want on there
Method
(we suggest you read everything at least once before doing anything)
1) Blend the base ingredients in a food processor until it has a coarse sticky texture, but isn’t yet a paste or dough.
2) Line a cake pan with baking paper and spread the base mix on the base; press it down to compact it a little and ensure it is flat. If there’s room, put this in the freezer while you do the next bit. If not, the fridge will suffice.
3) Blend the main part ingredients apart from the cacao nibs, until smooth. Stir in the cacao nibs with a spoon.
4) Spread the main part evenly over the base, and allow everything you’ve built (in this recipe, not in life in general) to chill in the fridge for at least 4 hours.
5) Cut it into blocks of the size and shape you want to eat them, and (if adding the optional topping) separate the blocks slightly from each other, before drizzling with the chocolate topping. Put it back in the fridge to cool this too; an hour should be sufficient.
6) Serve!
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Which Tea Is Best, By Science?
- Which Plant Milk?
- Why You Should Diversify Your Nuts!
- Cashew Nuts vs Coconut – Which is Healthier?
- Cacao vs Carob – Which is Healthier?
Take care!
Share This Post
-
Getting antivirals for COVID too often depends on where you live and how wealthy you are
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medical experts recommend antivirals for people aged 70 and older who get COVID, and for other groups at risk of severe illness and hospitalisation from COVID.
But many older Australians have missed out on antivirals after getting sick with COVID. It is yet another way the health system is failing the most vulnerable.
CGN089/Shutterstock Who missed out?
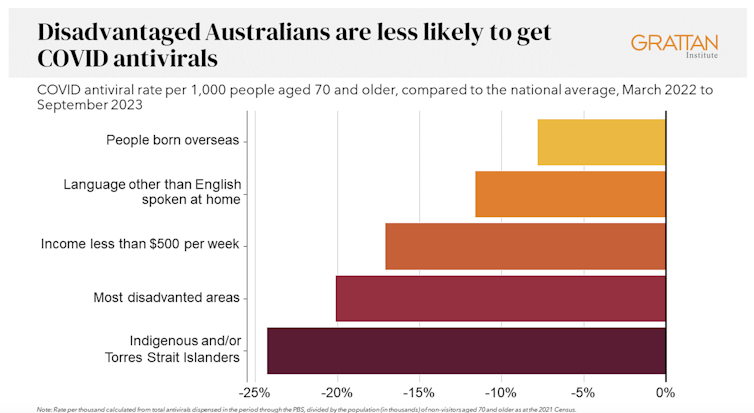
We analysed COVID antiviral uptake between March 2022 and September 2023. We found some groups were more likely to miss out on antivirals including Indigenous people, people from disadvantaged areas, and people from culturally and linguistically diverse backgrounds.
Some of the differences will be due to different rates of infection. But across this 18-month period, many older Australians were infected at least once, and rates of infection were higher in some disadvantaged communities.
How stark are the differences?
Compared to the national average, Indigenous Australians were nearly 25% less likely to get antivirals, older people living in disadvantaged areas were 20% less likely to get them, and people with a culturally or linguistically diverse background were 13% less likely to get a script.
People in remote areas were 37% less likely to get antivirals than people living in major cities. People in outer regional areas were 25% less likely.
Dispensing rates by group. Grattan Institute Even within the same city, the differences are stark. In Sydney, people older than 70 in the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were nearly twice as likely to have had an antiviral as those in Fairfield, in Sydney’s south-west.
Older people in leafy inner-eastern Melbourne (including Canterbury, Hawthorn and Kew) were 1.8 times more likely to have had an antiviral as those in Brimbank (which includes Sunshine) in the city’s west.
Why are people missing out?
COVID antivirals should be taken when symptoms first appear. While awareness of COVID antivirals is generally strong, people often don’t realise they would benefit from the medication. They wait until symptoms get worse and it is too late.
Frequent GP visits make a big difference. Our analysis found people 70 and older who see a GP more frequently were much more likely to be dispensed a COVID antiviral.
Regular visits give an opportunity for preventive care and patient education. For example, GPs can provide high-risk patients with “COVID treatment plans” as a reminder to get tested and seek treatment as soon as they are unwell.
Difficulty seeing a GP could help explain low antiviral use in rural areas. Compared to people in major cities, people in small rural towns have about 35% fewer GPs, see their GP about half as often, and are 30% more likely to report waiting too long for an appointment.
Just like for vaccination, a GP’s focus on antivirals probably matters, as does providing care that is accessible to people from different cultural backgrounds.
Care should go those who need it
Since the period we looked at, evidence has emerged that raises doubts about how effective antivirals are, particularly for people at lower risk of severe illness. That means getting vaccinated is more important than getting antivirals.
But all Australians who are eligible for antivirals should have the same chance of getting them.
These drugs have cost more than A$1.7 billion, with the vast majority of that money coming from the federal government. While dispensing rates have fallen, more than 30,000 packs of COVID antivirals were dispensed in August, costing about $35 million.
Such a huge investment shouldn’t be leaving so many people behind. Getting treatment shouldn’t depend on your income, cultural background or where you live. Instead, care should go to those who need it the most.
Getting antivirals shouldn’t depend on who your GP is. National Cancer Institute/Unsplash People born overseas have been 40% more likely to die from COVID than those born here. Indigenous Australians have been 60% more likely to die from COVID than non-Indigenous people. And the most disadvantaged people have been 2.8 times more likely to die from COVID than those in the wealthiest areas.
All those at-risk groups have been more likely to miss out on antivirals.
It’s not just a problem with antivirals. The same groups are also disproportionately missing out on COVID vaccination, compounding their risk of severe illness. The pattern is repeated for other important preventive health care, such as cancer screening.
A 3-step plan to meet patients’ needs
The federal government should do three things to close these gaps in preventive care.
First, the government should make Primary Health Networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with GPs and step in to boost uptake in communities that are missing out.
Second, the government should extend its MyMedicare reforms. MyMedicare gives general practices flexible funding to care for patients who live in residential aged care or who visit hospital frequently. That approach should be expanded to all patients, with more funding for poorer and sicker patients. That will give GP clinics time to advise patients about preventive health, including COVID vaccines and antivirals, before they get sick.
Third, team-based pharmacist prescribing should be introduced. Then pharmacists could quickly dispense antivirals for patients if they have a prior agreement with the patient’s GP. It’s an approach that would also work for medications for chronic diseases, such as cardiovascular disease.
COVID antivirals, unlike vaccines, have been keeping up with new variants without the need for updates. If a new and more harmful variant emerges, or when a new pandemic hits, governments should have these systems in place to make sure everyone who needs treatment can get it fast.
In the meantime, fairer access to care will help close the big and persistent gaps in health between different groups of Australians.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
154 million lives saved in 50 years: 5 charts on the global success of vaccines
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We know vaccines have been a miracle for public health. Now, new research led by the World Health Organization has found vaccines have saved an estimated 154 million lives in the past 50 years from 14 different diseases. Most of these have been children under five, and around two-thirds children under one year old.
In 1974 the World Health Assembly launched the Expanded Programme on Immunization with the goal to vaccinate all children against diphtheria, tetanus, pertussis (whooping cough), measles, polio, tuberculosis and smallpox by 1990. The program was subsequently expanded to include several other diseases.
The modelling, marking 50 years since this program was established, shows a child aged under ten has about a 40% greater chance of living until their next birthday, compared to if we didn’t have vaccines. And these positive effects can be seen well into adult life. A 50-year-old has a 16% greater chance of celebrating their next birthday thanks to vaccines.
What the study did
The researchers developed mathematical and statistical models which took in vaccine coverage data and population numbers from 194 countries for the years 1974–2024. Not all diseases were included (for example smallpox, which was eradicated in 1980, was left out).
The analysis includes vaccines for 14 diseases, with 11 of these included in the Expanded Programme on Immunization. For some countries, additional vaccines such as Japanese encephalitis, meningitis A and yellow fever were included, as these diseases contribute to major disease burden in certain settings.
The models were used to simulate how diseases would have spread from 1974 to now, as vaccines were introduced, for each country and age group, incorporating data on increasing vaccine coverage over time.
Children are the greatest beneficiaries of vaccines
Since 1974, the rates of deaths in children before their first birthday has more than halved. The researchers calculated almost 40% of this reduction is due to vaccines.
The effects have been greatest for children born in the 1980s because of the intensive efforts made globally to reduce the burden of diseases like measles, polio and whooping cough.
Some 60% of the 154 million lives saved would have been lives lost to measles. This is likely due to its ability to spread rapidly. One person with measles can spread the infection to 12–18 people.
The study also found some variation across different parts of the world. For example, vaccination programs have had a much greater impact on the probability of children living longer across low- and middle-income countries and settings with weaker health systems such as the eastern Mediterranean and African regions. These results highlight the important role vaccines play in promoting health equity.
Vaccine success is not assured
Low or declining vaccine coverage can lead to epidemics which can devastate communities and overwhelm health systems.
Notably, the COVID pandemic saw an overall decline in measles vaccine coverage, with 86% of children having received their first dose in 2019 to 83% in 2022. This is concerning because very high levels of vaccination coverage (more than 95%) are required to achieve herd immunity against measles.
In Australia, the coverage for childhood vaccines, including measles, mumps and rubella, has declined compared to before the pandemic.
This study is a reminder of why we need to continue to vaccinate – not just against measles, but against all diseases we have safe and effective vaccines for.
The results of this research don’t tell us the full story about the impact of vaccines. For example, the authors didn’t include data for some vaccines such as COVID and HPV (human papillomavirus). Also, like with all modelling studies, there are some uncertainties, as data was not available for all time periods and countries.
Nonetheless, the results show the success of global vaccination programs over time. If we want to continue to see lives saved, we need to keep investing in vaccination locally, regionally and globally.
Meru Sheel, Associate Professor and Epidemiologist, Infectious Diseases, Immunisation and Emergencies Group, Sydney School of Public Health, University of Sydney and Alexandra Hogan, Mathematical epidemiologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Frozen/Thawed/Refrozen Meat: How Much Is Safety, And How Much Is Taste?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What You Can (And Can’t) Safely Do With Frozen Meat
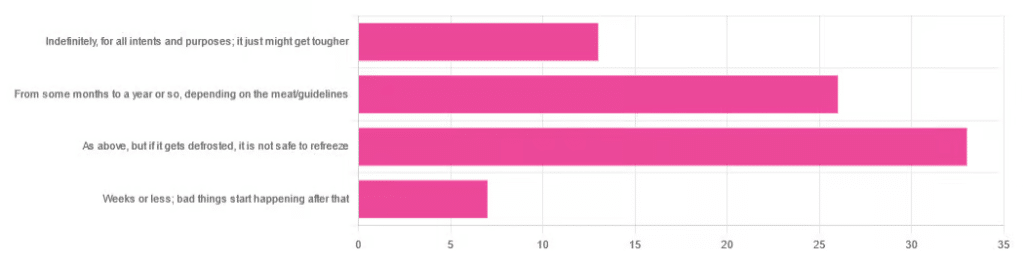
Yesterday, we asked you:
❝You have meat in the freezer. How long is it really safe to keep it?❞
…and got a range of answers, mostly indicating to a) follow the instructions (a very safe general policy) and b) do not refreeze if thawed because that would be unsafe. Fewer respondents indicated that meat could be kept for much longer than guidelines say, or conversely, that it should only be kept for weeks or less.
So, what does the science say?
Meat can be kept indefinitely (for all intents and purposes) in a freezer; it just might get tougher: True or False?
False, assuming we are talking about a normal household electrical freezer that bottoms out at about -18℃ / 0℉.
Fun fact: cryobiologists cryopreserve tissue samples (so basically, meat) at -196℃ / -320℉, and down at those temperatures, the tissues will last a lot longer than you will (and, for all practical purposes: indefinitely). There are other complications with doing so (such as getting the sample through the glass transition point without cracking it during the vitrification process) but those are beyond the scope of this article.
If you remember back to your physics or perhaps chemistry classes at school, you’ll know that molecules move more quickly at higher temperatures, and more slowly at lower ones, only approaching true stillness as they near absolute zero (-273℃ / -459℉ / 0K ← we’re not saying it’s ok, although it is; rather, that is zero kelvin; no degree sign is used with kelvins)
That means that when food is frozen, the internal processes aren’t truly paused; it’s just slowed to a point of near imperceptibility.
So, all the way up at the relatively warm temperatures of a household freezer, a lot of processes are still going on.
What this means in practical terms: those guidelines saying “keep in the freezer for up to 4 months”, “keep in the freezer for up to 9 months”, “keep in the freezer for up to 12 months” etc are being honest with you.
More or less, anyway! They’ll usually underestimate a little to be on the safe side—but so should you.
Bad things start happening within weeks at most: True or False?
False, for all practical purposes. Again, assuming a normal and properly-working household freezer as described above.
(True, technically but misleadingly: the bad things never stopped; they just slowed down to a near imperceptible pace—again, as described above)
By “bad” here we should clarify we mean “dangerous”. One subscriber wrote:
❝Meat starts losing color and flavor after being in the freezer for too long. I keep meat in the freezer for about 2 months at the most❞
…and as a matter of taste, that’s fair enough!
It is unsafe to refreeze meat that has been thawed: True or False?
False! Assuming it has otherwise been kept chilled, just the same as for fresh meat.
Food poisoning comes from bacteria, and there is nothing about the meat previously having been frozen that will make it now have more bacteria.
That means, for example…
- if it was thawed (but chilled) for a period of time, treat it like you would any other meat that has been chilled for that period of time (so probably: use it or freeze it, unless it’s been more than a few days)
- if it was thawed (and at room temperature) for a period of time, treat it like you would any other meat that has been at room temperature for that period of time (so probably: throw it out, unless the period of time is very small indeed)
The USDA gives for 2 hours max at room temperature before considering it unsalvageable, by the way.
However! Whenever you freeze meat (or almost anything with cells, really), ice crystals will form in and between cells. How much ice crystallization occurs depends on several variables, with how much water there is present in the food is usually the biggest factor (remember that animal cells are—just like us—mostly water).
Those ice crystals will damage the cell walls, causing the food to lose structural integrity. When you thaw it out, the ice crystals will disappear but the damage will be left behind (this is what “freezer burn” is).
So if your food seems a little “squishy” after having been frozen and thawed, that’s why. It’s not rotten; it’s just been stabbed countless times on a microscopic level.
The more times you freeze and thaw and refreeze food, the more this will happen. Your food will degrade in structural integrity each time, but the safety of it won’t have changed meaningfully.
Want to know more?
Further reading:
You can thaw and refreeze meat: five food safety myths busted
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Fibromyalgia Is Not An Acceptable Diagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Efrat Lamandre makes the case that fibromyalgia is less of a useful diagnosis and more of a rubber stamp, much like the role historically often fulfilled by “heart failure” as an official cause of death (because certainly, that heart sure did stop beating). It’s a way of answering the question without answering the question.
…and what to look for instead
Fibromyalgia is characterized by chronic pain, tenderness, sleep disturbances, fatigue, and other symptoms. It’s often considered an “invisible” illness, because it’s the kind that’s easy to dismiss if you’re not the one carrying it. A broken leg, one can point at and see it’s broken; a respiratory infection, one can see its effects and even test for presence of the pathogen and/or its antigens. But fibromyalgia? “It hurts and I’m tired” doesn’t quite cut it.
Much like “heart failure” as a cause of death when nothing else is implicated, fibromyalgia is a diagnosis that gets applied when known causes of chronic pain have been ruled out.
Dr. Lamandre advocates for functional medicine and seeking the underlying causes of the symptoms, rather than the industry standard approach, which is to just manage the symptoms themselves with medications (of course, managing the symptoms with medications has its place; there is no need to suffer needlessly if pain relief can be used; it’s just not a sufficient response).
She notes that potential triggers for fibromyalgia include microbiome imbalances, food sensitivities, thyroid issues, nutrient deficiencies, adrenal fatigue, mitochondrial dysfunction, mold toxicity, Lyme disease, and more. Is this really just one illness? Maybe, but quite possibly not.
In short… If you are given a diagnosis of fibromyalgia, she advises that you insist doctors keep on looking, because that’s not an answer.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Managing Chronic Pain (Realistically!)
- How To Eat To Beat Chronic Fatigue ← yes, including how to do so when you are chronically fatigued. In other words, this isn’t just dietary advice, but rather practical advice too
- When Painkillers Aren’t Helping, These Things Might
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can you ‘boost’ your immune system?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As flu season and a likely winter COVID-19 wave approach, you may encounter both proven and unproven methods claiming to “boost” your immune system. Before you reach for supplements, learn more about how the immune system works, how vaccines give us the best protection against many illnesses, and how some lifestyle factors can help your immune system function properly.
What is the immune system?
The immune system is the body’s first line of defense against invaders like viruses, bacteria, or fungi. You develop immunity—or protection from infection—when your immune system has learned how to recognize an invader and attack it before it makes you sick.
How can you boost your immune system?
You can teach your immune system how to fight back against dangerous invaders by staying up to date on vaccines. This season’s updated flu and COVID-19 vaccines target newer variants and are recommended for everyone 6 months and older.
Vaccines reduce your risk of getting sick and spreading illness to others. Even if you get infected with a disease after you’ve been vaccinated against it, the vaccine will still increase protection against severe illness, hospitalization, and death.
People who have compromised immune systems due to certain health conditions or because they need to take immunosuppressant medications may need additional vaccine doses.
Find out which vaccines you and your children need by using the CDC’s Adult Vaccine Assessment Tool and Child and Adolescent Vaccine Assessment Tool. Talk to your health care provider about the best vaccines for your family.
Find pharmacies offering updated flu and COVID-19 vaccines by visiting Vaccines.gov.
Can supplements boost your immune system?
Many vitamin, mineral, and herbal supplements that are marketed as “immune boosting” have little to no effect on your immune system. Research is split on whether some of these supplements—like vitamin C, vitamin D, and zinc—are capable of helping your body fight infections.
Plus, the Food and Drug Administration typically does not review supplements until after they have reached store shelves, and companies can sell supplements without notifying the FDA. This means that supplements may not be accurately labeled.
Eating a diverse diet rich in fruits and vegetables is the best way for most people to absorb nutrients that support optimal immune system function. People with certain health conditions and deficiencies may need specific supplements prescribed by a health care provider. For example, people with anemia may need iron supplements in order to maintain appropriate iron levels.
Before you begin taking a new supplement, talk to your health care provider, as some supplements may interact with medications you are taking or worsen certain health conditions.
Can lifestyle factors strengthen your immune system?
Based on current evidence, there is no direct link between lifestyle changes and enhanced immunity to infections. However, maintaining a healthy lifestyle through the following practices can help ensure that your immune system functions as it should:
- Eat a diet rich in fruits and vegetables.
- Exercise regularly.
- Don’t smoke.
- Limit or eliminate alcohol consumption.
- Get seven or more hours of sleep per night.
- Reduce stress.
Taking steps to avoid contact with germs also reduces your risk of getting sick. Safer sex barriers like condoms protect against HIV, while wearing a high-quality, well-fitting mask—especially in high-risk environments—protects against COVID-19. Both of these illnesses can reduce your production of white blood cells, which protect against infection.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: