What pathogen might spark the next pandemic? How scientists are preparing for ‘disease X’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Before the COVID pandemic, the World Health Organization (WHO) had made a list of priority infectious diseases. These were felt to pose a threat to international public health, but where research was still needed to improve their surveillance and diagnosis. In 2018, “disease X” was included, which signified that a pathogen previously not on our radar could cause a pandemic.
While it’s one thing to acknowledge the limits to our knowledge of the microbial soup we live in, more recent attention has focused on how we might systematically approach future pandemic risks.
Former US Secretary of Defense Donald Rumsfeld famously talked about “known knowns” (things we know we know), “known unknowns” (things we know we don’t know), and “unknown unknowns” (the things we don’t know we don’t know).
Although this may have been controversial in its original context of weapons of mass destruction, it provides a way to think about how we might approach future pandemic threats.

Influenza: a ‘known known’
Influenza is largely a known entity; we essentially have a minor pandemic every winter with small changes in the virus each year. But more major changes can also occur, resulting in spread through populations with little pre-existing immunity. We saw this most recently in 2009 with the swine flu pandemic.
However, there’s a lot we don’t understand about what drives influenza mutations, how these interact with population-level immunity, and how best to make predictions about transmission, severity and impact each year.
The current H5N1 subtype of avian influenza (“bird flu”) has spread widely around the world. It has led to the deaths of many millions of birds and spread to several mammalian species including cows in the United States and marine mammals in South America.
Human cases have been reported in people who have had close contact with infected animals, but fortunately there’s currently no sustained spread between people.
While detecting influenza in animals is a huge task in a large country such as Australia, there are systems in place to detect and respond to bird flu in wildlife and production animals.

It’s inevitable there will be more influenza pandemics in the future. But it isn’t always the one we are worried about.
Attention had been focused on avian influenza since 1997, when an outbreak in birds in Hong Kong caused severe disease in humans. But the subsequent pandemic in 2009 originated in pigs in central Mexico.
Coronaviruses: an ‘unknown known’
Although Rumsfeld didn’t talk about “unknown knowns”, coronaviruses would be appropriate for this category. We knew more about coronaviruses than most people might have thought before the COVID pandemic.
We’d had experience with severe acute respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS) causing large outbreaks. Both are caused by viruses closely related to SARS-CoV-2, the coronavirus that causes COVID. While these might have faded from public consciousness before COVID, coronaviruses were listed in the 2015 WHO list of diseases with pandemic potential.
Previous research into the earlier coronaviruses proved vital in allowing COVID vaccines to be developed rapidly. For example, the Oxford group’s initial work on a MERS vaccine was key to the development of AstraZeneca’s COVID vaccine.
Similarly, previous research into the structure of the spike protein – a protein on the surface of coronaviruses that allows it to attach to our cells – was helpful in developing mRNA vaccines for COVID.
It would seem likely there will be further coronavirus pandemics in the future. And even if they don’t occur at the scale of COVID, the impacts can be significant. For example, when MERS spread to South Korea in 2015, it only caused 186 cases over two months, but the cost of controlling it was estimated at US$8 billion (A$11.6 billion).

The 25 viral families: an approach to ‘known unknowns’
Attention has now turned to the known unknowns. There are about 120 viruses from 25 families that are known to cause human disease. Members of each viral family share common properties and our immune systems respond to them in similar ways.
An example is the flavivirus family, of which the best-known members are yellow fever virus and dengue fever virus. This family also includes several other important viruses, such as Zika virus (which can cause birth defects when pregnant women are infected) and West Nile virus (which causes encephalitis, or inflammation of the brain).
The WHO’s blueprint for epidemics aims to consider threats from different classes of viruses and bacteria. It looks at individual pathogens as examples from each category to expand our understanding systematically.
The US National Institute of Allergy and Infectious Diseases has taken this a step further, preparing vaccines and therapies for a list of prototype pathogens from key virus families. The goal is to be able to adapt this knowledge to new vaccines and treatments if a pandemic were to arise from a closely related virus.
Pathogen X, the ‘unknown unknown’
There are also the unknown unknowns, or “disease X” – an unknown pathogen with the potential to trigger a severe global epidemic. To prepare for this, we need to adopt new forms of surveillance specifically looking at where new pathogens could emerge.
In recent years, there’s been an increasing recognition that we need to take a broader view of health beyond only thinking about human health, but also animals and the environment. This concept is known as “One Health” and considers issues such as climate change, intensive agricultural practices, trade in exotic animals, increased human encroachment into wildlife habitats, changing international travel, and urbanisation.
This has implications not only for where to look for new infectious diseases, but also how we can reduce the risk of “spillover” from animals to humans. This might include targeted testing of animals and people who work closely with animals. Currently, testing is mainly directed towards known viruses, but new technologies can look for as yet unknown viruses in patients with symptoms consistent with new infections.
We live in a vast world of potential microbiological threats. While influenza and coronaviruses have a track record of causing past pandemics, a longer list of new pathogens could still cause outbreaks with significant consequences.
Continued surveillance for new pathogens, improving our understanding of important virus families, and developing policies to reduce the risk of spillover will all be important for reducing the risk of future pandemics.
This article is part of a series on the next pandemic.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women and Minorities Bear the Brunt of Medical Misdiagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Charity Watkins sensed something was deeply wrong when she experienced exhaustion after her daughter was born.
At times, Watkins, then 30, had to stop on the stairway to catch her breath. Her obstetrician said postpartum depression likely caused the weakness and fatigue. When Watkins, who is Black, complained of a cough, her doctor blamed the flu.
About eight weeks after delivery, Watkins thought she was having a heart attack, and her husband took her to the emergency room. After a 5½-hour wait in a North Carolina hospital, she returned home to nurse her baby without seeing a doctor.
When a physician finally examined Watkins three days later, he immediately noticed her legs and stomach were swollen, a sign that her body was retaining fluid. After a chest X-ray, the doctor diagnosed her with heart failure, a serious condition in which the heart becomes too weak to adequately pump oxygen-rich blood to organs throughout the body. Watkins spent two weeks in intensive care.
She said a cardiologist later told her, “We almost lost you.”
Watkins is among 12 million adults misdiagnosed every year in the U.S.
In a study published Jan. 8 in JAMA Internal Medicine, researchers found that nearly 1 in 4 hospital patients who died or were transferred to intensive care had experienced a diagnostic error. Nearly 18% of misdiagnosed patients were harmed or died.
In all, an estimated 795,000 patients a year die or are permanently disabled because of misdiagnosis, according to a study published in July in the BMJ Quality & Safety periodical.
Some patients are at higher risk than others.
Women and racial and ethnic minorities are 20% to 30% more likely than white men to experience a misdiagnosis, said David Newman-Toker, a professor of neurology at Johns Hopkins School of Medicine and the lead author of the BMJ study. “That’s significant and inexcusable,” he said.
Researchers call misdiagnosis an urgent public health problem. The study found that rates of misdiagnosis range from 1.5% of heart attacks to 17.5% of strokes and 22.5% of lung cancers.
Weakening of the heart muscle — which led to Watkins’ heart failure — is the most common cause of maternal death one week to one year after delivery, and is more common among Black women.
Heart failure “should have been No. 1 on the list of possible causes” for Watkins’ symptoms, said Ronald Wyatt, chief science and chief medical officer at the Society to Improve Diagnosis in Medicine, a nonprofit research and advocacy group.
Maternal mortality for Black mothers has increased dramatically in recent years. The United States has the highest maternal mortality rate among developed countries. According to the Centers for Disease Control and Prevention, non-Hispanic Black mothers are 2.6 times as likely to die as non-Hispanic white moms. More than half of these deaths take place within a year after delivery.
Research shows that Black women with childbirth-related heart failure are typically diagnosed later than white women, said Jennifer Lewey, co-director of the pregnancy and heart disease program at Penn Medicine. That can allow patients to further deteriorate, making Black women less likely to fully recover and more likely to suffer from weakened hearts for the rest of their lives.
Watkins said the diagnosis changed her life. Doctors advised her “not to have another baby, or I might need a heart transplant,” she said. Being deprived of the chance to have another child, she said, “was devastating.”
Racial and gender disparities are widespread.
Women and minority patients suffering from heart attacks are more likely than others to be discharged without diagnosis or treatment.
Black people with depression are more likely than others to be misdiagnosed with schizophrenia.
Minorities are less likely than whites to be diagnosed early with dementia, depriving them of the opportunities to receive treatments that work best in the early stages of the disease.
Misdiagnosis isn’t new. Doctors have used autopsy studies to estimate the percentage of patients who died with undiagnosed diseases for more than a century. Although those studies show some improvement over time, life-threatening mistakes remain all too common, despite an array of sophisticated diagnostic tools, said Hardeep Singh, a professor at Baylor College of Medicine who studies ways to improve diagnosis.
“The vast majority of diagnoses can be made by getting to know the patient’s story really well, asking follow-up questions, examining the patient, and ordering basic tests,” said Singh, who is also a researcher at Houston’s Michael E. DeBakey VA Medical Center. When talking to people who’ve been misdiagnosed, “one of the things we hear over and over is, ‘The doctor didn’t listen to me.’”
Racial disparities in misdiagnosis are sometimes explained by noting that minority patients are less likely to be insured than white patients and often lack access to high-quality hospitals. But the picture is more complicated, said Monika Goyal, an emergency physician at Children’s National Hospital in Washington, D.C., who has documented racial bias in children’s health care.
In a 2020 study, Goyal and her colleagues found that Black kids with appendicitis were less likely than their white peers to be correctly diagnosed, even when both groups of patients visited the same hospital.
Although few doctors deliberately discriminate against women or minorities, Goyal said, many are biased without realizing it.
“Racial bias is baked into our culture,” Goyal said. “It’s important for all of us to start recognizing that.”
Demanding schedules, which prevent doctors from spending as much time with patients as they’d like, can contribute to diagnostic errors, said Karen Lutfey Spencer, a professor of health and behavioral sciences at the University of Colorado-Denver. “Doctors are more likely to make biased decisions when they are busy and overworked,” Spencer said. “There are some really smart, well-intentioned providers who are getting chewed up in a system that’s very unforgiving.”
Doctors make better treatment decisions when they’re more confident of a diagnosis, Spencer said.
In an experiment, researchers asked doctors to view videos of actors pretending to be patients with heart disease or depression, make a diagnosis, and recommend follow-up actions. Doctors felt far more certain diagnosing white men than Black patients or younger women.
“If they were less certain, they were less likely to take action, such as ordering tests,” Spencer said. “If they were less certain, they might just wait to prescribe treatment.”
It’s easy to see why doctors are more confident when diagnosing white men, Spencer said. For more than a century, medical textbooks have illustrated diseases with stereotypical images of white men. Only 4.5% of images in general medical textbooks feature patients with dark skin.
That may help explain why patients with darker complexions are less likely to receive a timely diagnosis with conditions that affect the skin, from cancer to Lyme disease, which causes a red or pink rash in the earliest stage of infection. Black patients with Lyme disease are more likely to be diagnosed with more advanced disease, which can cause arthritis and damage the heart. Black people with melanoma are about three times as likely as whites to die within five years.
The covid-19 pandemic helped raise awareness that pulse oximeters — the fingertip devices used to measure a patient’s pulse and oxygen levels — are less accurate for people with dark skin. The devices work by shining light through the skin; their failures have delayed critical care for many Black patients.
Seven years after her misdiagnosis, Watkins is an assistant professor of social work at North Carolina Central University in Durham, where she studies the psychosocial effects experienced by Black mothers who survive severe childbirth complications.
“Sharing my story is part of my healing,” said Watkins, who speaks to medical groups to help doctors improve their care. “It has helped me reclaim power in my life, just to be able to help others.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
What are ‘collarium’ sunbeds? Here’s why you should stay away
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reports have recently emerged that solariums, or sunbeds – largely banned in Australia because they increase the risk of skin cancer – are being rebranded as “collarium” sunbeds (“coll” being short for collagen).
Commercial tanning and beauty salons in Queensland, New South Wales and Victoria are marketing collariums, with manufacturers and operators claiming they provide a longer lasting tan and stimulate collagen production, among other purported benefits.
A collarium sunbed emits both UV radiation and a mix of visible wavelength colours to produce a pink or red light. Like an old-school sunbed, the user lies in it for ten to 20 minute sessions to quickly develop a tan.
But as several experts have argued, the providers’ claims about safety and effectiveness don’t stack up.
Why were sunbeds banned?
Commercial sunbeds have been illegal across Australia since 2016 (except for in the Northern Territory) under state-based radiation safety laws. It’s still legal to sell and own a sunbed for private use.
Their dangers were highlighted by young Australians including Clare Oliver who developed melanoma after using sunbeds. Oliver featured in the No Tan Is Worth Dying For campaign and died from her melanoma at age 26 in 2007.
Sunbeds lead to tanning by emitting UV radiation – as much as six times the amount of UV we’re exposed to from the summer sun. When the skin detects enough DNA damage, it boosts the production of melanin, the brown pigment that gives you the tanned look, to try to filter some UV out before it hits the DNA. This is only partially successful, providing the equivalent of two to four SPF.
Essentially, if your body is producing a tan, it has detected a significant amount of DNA damage in your skin.
Research shows people who have used sunbeds at least once have a 41% increased risk of developing melanoma, while ten or more sunbed sessions led to a 100% increased risk.
In 2008, Australian researchers estimated that each year, sunbeds caused 281 cases of melanoma, 2,572 cases of squamous cell carcinoma (another common type of skin cancer), and $3 million in heath-care costs, mostly to Medicare.
How are collarium sunbeds supposed to be different?
Australian sellers of collarium sunbeds imply they are safe, but their machine descriptions note the use of UV radiation, particularly UVA.
UVA is one part of the spectrum of UV radiation. It penetrates deeper into the skin than UVB. While UVB promotes cancer-causing mutations by discharging energy straight into the DNA strand, UVA sets off damage by creating reactive oxygen species, which are unstable compounds that react easily with many types of cell structures and molecules. These damage cell membranes, protein structures and DNA.
Evidence shows all types of sunbeds increase the risk of melanoma, including those that use only UVA.
Some manufacturers and clinics suggest the machine’s light spectrum increases UV compatibility, but it’s not clear what this means. Adding red or pink light to the mix won’t negate the harm from the UV. If you’re getting a tan, you have a significant amount of DNA damage.
Collagen claims
One particularly odd claim about collarium sunbeds is that they stimulate collagen.
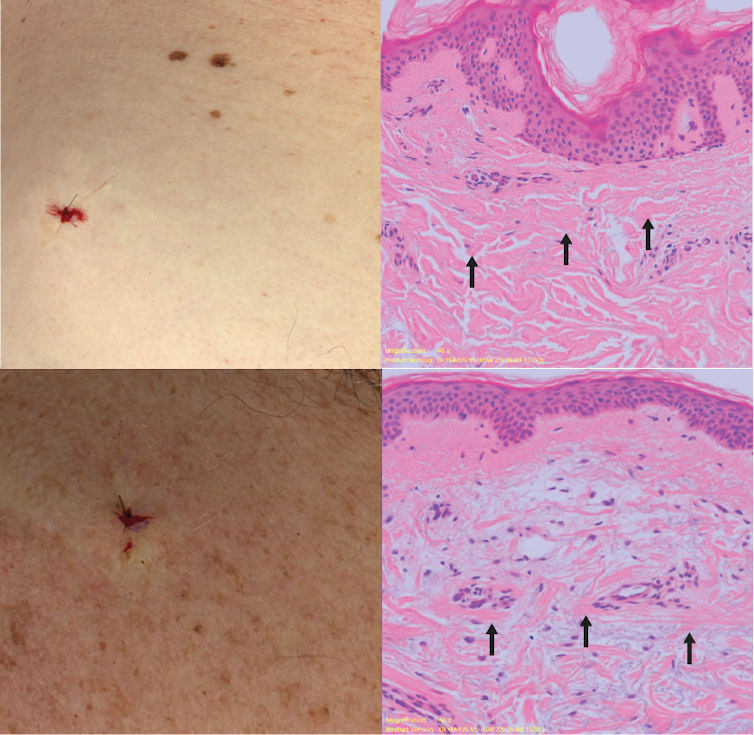
Collagen is the main supportive tissue in our skin. It provides elasticity and strength, and a youthful appearance. Collagen is constantly synthesised and broken down, and when the balance between production and recycling is lost, the skin loses strength and develops wrinkles. The collagen bundles become thin and fragmented. This is a natural part of ageing, but is accelerated by UV exposure.
Sun-protected skin (top) has thick bands of pink collagen (arrows) in the dermis, as seen on microscopic examination. Chronically sun-damaged skin (bottom) has much thinner collagen bands.
Katie Lee/UQThe reactive oxygen species generated by UVA light damage existing collagen structures and kick off a molecular chain of events that downgrades collagen-producing enzymes and increases collagen-destroying enzymes. Over time, a build-up of degraded collagen fragments in the skin promotes even more destruction.
While there is growing evidence red light therapy alone could be useful in wound healing and skin rejuvenation, the UV radiation in collarium sunbeds is likely to undo any benefit from the red light.
What about phototherapy?
There are medical treatments that use controlled UV radiation doses to treat chronic inflammatory skin diseases like psoriasis.
The anti-collagen effects of UVA can also be used to treat thickened scars and keloids. Side-effects of UV phototherapy include tanning, itchiness, dryness, cold sore virus reactivation and, notably, premature skin ageing.
These treatments use the minimum exposure necessary to treat the condition, and are usually restricted to the affected body part to minimise risks of future cancer. They are administered under medical supervision and are not recommended for people already at high risk of skin cancer, such as people with atypical moles.
So what happens now?
It looks like many collariums are just sunbeds rebranded with red light. Queensland Health is currently investigating whether these salons are breaching the state’s Radiation Safety Act, and operators could face large fines.
As the 2024 Australians of the Year – melanoma treatment pioneers Georgina Long and Richard Scolyer – highlighted in their acceptance speech, “there is nothing healthy about a tan”, and we need to stop glamorising tanning.
However, if you’re desperate for the tanned look, there is a safer and easy way to get one – out of a bottle or by visiting a salon for a spray tan.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Anne Cust, Professor of Cancer Epidemiology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Next-Level Headache Hacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Muscle With A Lot Of Therapeutic Value
First, a quick anatomy primer, so that the rest makes sense. We’re going to be talking about your sternocleidomastoid (SCM) muscle today.
To find it, there are two easy ways:
- look in a mirror, turn your head to one side and it’ll stick out on the opposite side of your neck
- look at this diagram
(we’re going to talk about it in the singular, but you have one on each side)
This muscle is interesting for very many reasons, but what we’re going to focus on today is that massaging/stretching it (correctly!) can benefit several things that are right next to it and/or behind it, namely:
- The tenth cranial nerve
- The eleventh cranial nerve
- The carotid artery
Why do we care about these?
Well, we would die quickly without the first and last of those. However, more practically, massaging each has benefits:
The tenth cranial nerve
This one is also known by its superhero alter-ego name:
The Vagus Nerve (And How You Can Make Use Of It)
The eleventh cranial nerve
This one’s not nearly so critical to life, but it does facilitate most of the motor functions in that general part of the body—including some mechanics of speech production, and maintaining posture of the shoulders/neck/head (which in turn strongly affects presence/absence of certain kinds of headaches).
The carotid artery
We suspect you know what this one does already; it supplies the brain (and the rest of your head, for that matter) with oxygenated blood.
What is useful to know today, is that it can be massaged, via the SCM, in a way that brings about a gentler version of this “one weird trick” to cure a lot of kinds of headaches:
Curing Headaches At Home With Actual Science
How (And Why) To Massage Your SCM
…to relieve many kinds of headache, migraine, eye-ache, and tension or pain the jaw. It’s not a magical cure all so this comes with no promises, but it can and will help with a lot of things.
In few words: turn your ahead away from the side where it hurts (if both, just pick one and then repeat for the other side), and slightly downwards. When your SCM sticks out a bit on the other side, gently pinch and rub it, working from the bottom to the top.
If you prefer videos, here is a demonstration:
How (And Why) To Stretch Your SCM
The above already includes a little stretch, but you can stretch it in a way that specifically stimulates your vagus nerve (this is good for many things).
In few words: stand (or sit) up straight, and interlace your fingers together. Put your hands on the back of your neck, thumbs-downwards, and (keeping your face forward) look to one side with your eyes only, and hold that until you feel the urge to yawn (it’ll probably take between about 3 seconds and 30 seconds). Then repeat on the other side.
If you prefer videos, this one is a very slight variation of what we just described but works the same way:
Take care!
Share This Post
Related Posts
-
Flossing Without Flossing?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Flossing Without Flossing?
You almost certainly brush your teeth. You might use mouthwash. A lot of people floss for three weeks at a time, often in January.
There are a lot of options for oral hygiene; variations of the above, and many alternatives too. This is a big topic, so rather than try to squeeze it all in one, this will be a several-part series.
The first part was: Toothpastes & Mouthwashes: Which Help And Which Harm?
How important is flossing?
Interdental cleaning is indeed pretty important, even though it may not have the heart health benefits that have been widely advertised:
However! The health of our gums is very important in and of itself, especially as we get older:
Flossing Is Associated with Improved Oral Health in Older Adults
But! It helps to avoid periodontal (e.g. gum) disease, not dental caries:
Flossing for the management of periodontal diseases and dental caries in adults
And! Most certainly it can help avoid a stack of other diseases:
Interdental Cleaning Is Associated with Decreased Oral Disease Prevalence
…so in short, if you’d like to have happy healthy teeth and gums, flossing is an important adjunct, and/but not a one-stop panacea.
Is it better to floss before or after brushing?
As you prefer. A team of scientists led by Dr. Claudia Silva studied this, and found that there was “no statistical difference between brush-floss and floss-brush”:
Flossing is tedious. How do we floss without flossing?
This is (mostly) about water-flossing! Which does for old-style floss what sonic toothbrushes to for old-style manual toothbrushes.
If you’re unfamiliar, it means using a device that basically power-washes your teeth, but with a very narrow high-pressure jet of water.
Do they work? Yes:
As for how it stacks up against traditional flossing, Liang et al. found:
❝In our previous single-outcome analysis, we concluded that interdental brushes and water jet devices rank highest for reducing gingival inflammation while toothpick and flossing rank last.
In this multioutcome Bayesian network meta-analysis with equal weight on gingival inflammation and bleeding-on-probing, the surface under the cumulative ranking curve was 0.87 for water jet devices and 0.85 for interdental brushes.
Water jet devices and interdental brushes remained the two best devices across different sets of weightings for the gingival inflammation and bleeding-on-probing. ❞
~ Journal of Evidence-Based Dental Practice
You may be wondering how safe it is if you have had dental work done, and, it appears to be quite safe, for example:
BDJ | Water-jet flossing: effect on composites
Want to try water-flossing?
Here are some examples on Amazon:
- Waterpik Complete Care 9.0 ← example of a top-end water-flossing device
- Philips Sonicare Power Flosser 3000 ← top-tier not-Waterpik-brand device
- INSMART Cordless Water Dental Flosser ← very low price and still average 4.5 star reviews, so in our opinion, a fine first choice
Bonus: if you haven’t tried interdental brushes, here’s an example for that
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The FIRST Program: Fighting Insulin Resistance with Strength Training – by Dr. William Shang
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of advice about fighting insulin resistance focuses on diet. And, that’s worthwhile! How we eat does make a huge difference to our insulin responses (as does fasting). But, we expect our regular 10almonds readers either know these things now, or can read one of several very good books we’ve already reviewed about such.
This one’s different: it focuses, as the title promises, on fighting insulin resistance with strength training. And why?
It’s because of the difference that our body composition makes to our metabolism. Now, our body fat percentage is often talked about (or, less usefully but more prevalently, even if woefully misleadingly, our BMI), but Dr. Shang makes the case for it being our musculature that has the biggest impact; because of how it hastens our metabolism, and because of how it is much healthier for the body to store glycogen in muscle tissue, than just cramming whatever it can into the liver and visceral fat. It becomes relevant, then, that there’s a limit to how much glycogen can be stored in muscle tissue, and that limit is how much muscle you have.
This is not, however, 243 pages to say “lift some weights, lazybones”. Rather, he explains the relevant pathophysiology (we will be more likely to adhere to things we understand, than things we do not), and gives practical advice on exercising the different kinds of muscle fibers, arguing that the whole is greater than the sum of its parts, as well as outlining an exercise program for the gym, plus a chapter on no-gym exercises too.
The style is quite dense, which may be offputting for some, but it suffices to take one’s time and read thoughtfully; the end result is worth it.
Bottom line: if you’d like to keep insulin resistance at bay, this book is an excellent extra tool for that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
“I Stretched Every Day For 30 Days: Game Changer!”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How much can an unflexible person really improve in just 20 minutes per day for a month? Makari Espe finds out:
Consistency really is key
We’re supposed to stretch at least 3 times per week; for many people, the reality is often more like 2 times per year (often the 1st and 2nd of January).
So, how quickly can such neglect be turned around?
Upon initial testing, she found she was even less flexible than thought, and set about her work:
The stretches she used were from random 20-minute full body stretch videos on YouTube, of which there are many, but she used a different one each day. As she went along, she found some favorite kinds of stretching and some favorite instructors, and settled on mostly Peloton stretching videos—she also switched to evening stretching sessions instead of morning.
Along the way, she already noticed gradual improvement in mobility and reduced body tension, and after 3 weeks, it had become a habit that she started craving.
The final test? There’s a marked improvement; see the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Yoga Teacher: “If I wanted to get flexible in 2025, here’s what I’d do”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: