No, your aches and pains don’t get worse in the cold. So why do we think they do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s cold and wet outside. As you get out of bed, you can feel it in your bones. Your right knee is flaring up again. That’ll make it harder for you to walk the dog or go to the gym. You think it must be because of the weather.
It’s a common idea, but a myth.
When we looked at the evidence, we found no direct link between most common aches and pains and the weather. In the first study of its kind, we found no direct link between the temperature or humidity with most joint or muscle aches and pains.
So why are so many of us convinced the weather’s to blame? Here’s what we think is really going on.

Weather can be linked to your health
The weather is often associated with the risk of new and ongoing health conditions. For example, cold temperatures may worsen asthma symptoms. Hot temperatures increase the risk of heart problems, such as arrhythmia (irregular heartbeat), cardiac arrest and coronary heart disease.
Many people are also convinced the weather is linked to their aches and pains. For example, two in every three people with knee, hip or hand osteoarthritis say cold temperatures trigger their symptoms.
Musculoskeletal conditions affect more than seven million Australians. So we set out to find out whether weather is really the culprit behind winter flare-ups.
What we did
Very few studies have been specifically and appropriately designed to look for any direct link between weather changes and joint or muscle pain. And ours is the first to evaluate data from these particular studies.
We looked at data from more than 15,000 people from around the world. Together, these people reported more than 28,000 episodes of pain, mostly back pain, knee or hip osteoarthritis. People with rheumatoid arthritis and gout were also included.
We then compared the frequency of those pain reports between different types of weather: hot or cold, humid or dry, rainy, windy, as well as some combinations (for example, hot and humid versus cold and dry).

What we found
We found changes in air temperature, humidity, air pressure and rainfall do not increase the risk of knee, hip or lower back pain symptoms and are not associated with people seeking care for a new episode of arthritis.
The results of this study suggest we do not experience joint or muscle pain flare-ups as a result of changes in the weather, and a cold day will not increase our risk of having knee or back pain.
In order words, there is no direct link between the weather and back, knee or hip pain, nor will it give you arthritis.
It is important to note, though, that very cold air temperatures (under 10°C) were rarely studied so we cannot make conclusions about worsening symptoms in more extreme changes in the weather.
The only exception to our findings was for gout, an inflammatory type of arthritis that can come and go. Here, pain increased in warmer, dry conditions.
Gout has a very different underlying biological mechanism to back pain or knee and hip osteoarthritis, which may explain our results. The combination of warm and dry weather may lead to increased dehydration and consequently increased concentration of uric acid in the blood, and deposition of uric acid crystals in the joint in people with gout, resulting in a flare-up.
Why do people blame the weather?
The weather can influence other factors and behaviours that consequently shape how we perceive and manage pain.
For example, some people may change their physical activity routine during winter, choosing the couch over the gym. And we know prolonged sitting, for instance, is directly linked to worse back pain. Others may change their sleep routine or sleep less well when it is either too cold or too warm. Once again, a bad night’s sleep can trigger your back and knee pain.
Likewise, changes in mood, often experienced in cold weather, trigger increases in both back and knee pain.
So these changes in behaviour over winter may contribute to more aches and pains, and not the weather itself.
Believing our pain will feel worse in winter (even if this is not the case) may also make us feel worse in winter. This is known as the nocebo effect.

What to do about winter aches and pains?
It’s best to focus on risk factors for pain you can control and modify, rather than ones you can’t (such as the weather).
You can:
- become more physically active. This winter, and throughout the year, aim to walk more, or talk to your health-care provider about gentle exercises you can safely do at home, with a physiotherapist, personal trainer or at the pool
- lose weight if obese or overweight, as this is linked to lower levels of joint pain and better physical function
- keep your body warm in winter if you feel some muscle tension in uncomfortably cold conditions. Also ensure your bedroom is nice and warm as we tend to sleep less well in cold rooms
- maintain a healthy diet and avoid smoking or drinking high levels of alcohol. These are among key lifestyle recommendations to better manage many types of arthritis and musculoskeletal conditions. For people with back pain, for example, a healthy lifestyle is linked with higher levels of physical function.
Manuela Ferreira, Professor of Musculoskeletal Health, Head of Musculoskeletal Program, George Institute for Global Health and Leticia Deveza, Rheumatologist and Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Coconut vs Avocado – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing coconut to avocado, we picked the avocado.
Why?
In terms of macros, avocado is lower in carbs and also in net carbs—coconut’s a little higher in fiber, but not enough to make up for the difference in carbs nor, when it comes to glycemic index and insulin index, the impact of coconut’s much higher fat content on insulin responses too. On which note, while coconut’s fats are broadly considered healthy (its impressive saturated fat content is formed of medium-chain triglycerides which, in moderation, are heart-healthy), avocado’s fats are even healthier, being mostly monounsaturated fat with some polyunsaturated (and about 15x less saturated fat). All in all, a fair win for avocado on the macros front, but coconut isn’t bad in moderation.
When it comes to vitamins, avocados are higher in vitamins A, B1, B2, B3, B5, B6, B9, C, E, K, and choline. Most of those differences are by very large margins. Coconuts are not higher in any vitamins. A huge, easy, “perfect score” win for avocados.
In the category of minerals, however, it’s coconut’s turn to sweep with more calcium, copper, iron, magnesium, manganese, phosphorus, zinc, and selenium—though the margins are mostly not nearly as impressive as avocado’s vitamin margins. Speaking of avocados, they do have more potassium than coconuts do, but the margin isn’t very large. A compelling win for coconut’s mineral content.
Adding up the sections, we get to a very credible win for avocados, but coconuts are also very respectable. So, as ever, enjoy both (although we do recommend exercising moderation in the case of coconuts, mainly because of the saturated fat content), and if you’re choosing between them for some purpose, then avocado will generally be the best option.
Want to learn more?
You might like to read:
- Can Saturated Fats Be Healthy? ← defying Betteridge’s Law here!
- Avocado, Coconut & Lime Crumble Pots ← if you do want to enjoy both, here’s a fabulous way to do so in style
Take care!
Share This Post

Delicious Quinoa Avocado Bread
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
They’re gluten-free, full of protein and healthy fats, generous with the fiber, easy to make, and tasty too! What’s not to love? Keep this recipe (and its ingredients) handy for next time you want healthy burger buns or similar:
You will need
- 2½ cups quinoa flour
- 2 cups almond flour (if allergic, just substitute more quinoa flour)
- 1 avocado, peeled, pitted, and mashed
- zest and juice of 1 lime
- 2 tbsp ground flaxseed
- 1 tsp baking powder
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: seeds, oats, or similar for topping the buns
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉/175℃.
2) Mix the flaxseed with ⅓ cup warm water and set aside.
3) Mix, in a large bowl, the quinoa flour and almond flour with the baking powder and the MSG or salt.
4) Mix, in a separate smaller bowl, the avocado and lime.
5) Add the wet ingredients to the dry, slowly, adding an extra ½ cup water as you do, and knead into a dough.
6) Divide the dough into 4 equal portions, each shaped into a ball and then slightly flattened, to create a burger bun shape. If you’re going to add any seeds or similar as a topping, add those now.
7) Bake them in the oven (on a baking sheet lined with baking paper) for 20–25 minutes. You can check whether they’re done the same way you would a cake, by piercing them to the center with a toothpick and seeing whether it comes out clean.
8) Serve when sufficiently cooled.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Gluten: What’s The Truth?
- Why You Should Diversify Your Nuts!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post

How To Keep On Keeping On?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Keep On Keeping On… Long Term!
For many when it comes to health-related goals and practices, it’s easy to find ourselves in a bit of a motivational dip around this time of year. The enthusiasm of new year’s resolutions has been and gone, and there’s not yet much of a drive to “get a beach body” or “be summer-ready”.
A word to the wise on those before moving on, though:
- How to get a beach body: take your body to a beach. Voilà. Beach body.
- Remember: the beach is there for your pleasure and entertainment, not the other way around!
- How to be summer-ready: the real question is, will summer be ready for you?
But what is this, demotivational rhetoric to discourage you from getting fit and healthy?
Not at all, but rather, to be sure that you’re pursuing your own goals and not just what you feel might be expected of you.
All that in mind, let’s get to the tips…
Focus on adding health
It can be tempting (and even, good) to cut down on unhealthy things. But when it comes to motivation, it’s harder to stay motivated for deprivation, than it is for some healthy addition to life.
So for example, this philosophy would advocate for:
- Instead of counting calories, count steps! Or even…
- Instead of counting calories, count colors! Eat the rainbow and all that. No, skittles do not count, but eating a variety of naturally different-colored foods will tend to result in adding different nutrients to your diet.
- Instead of cutting out sugar, add fruit! How many per day will you go for? If you don’t eat much fruit as it is, consider making it a goal to have even just one piece of fruit a day, then build up from there. Find fruit you like! If you pick the fruit you want instead of the fruit you think you “should” have, it’s basically a dessert snack.
We’ve recommended it before, and we’ll recommend it again, but if you’re interested in “adding health”, you should definitely check out:
Dr. Greger’s Daily Dozen (checklist, plus app if you want it)
More details: it’s a checklist of 12 things you should try to include in your diet, with a free streak-tracking app, if you want it, all based on the same scientific research as the best-selling book “How Not To Die”.
“Minimum effort!”
Did you see the movie “Deadpool”? The protagonist has a catch-phrase as he goes into battle, saying to himself “Maximum effort!”.
And, that’s all very well and good if your superpower is immediate recovery from pretty much anything, but for the rest of us, sometimes it’s good to hold ourselves to “minimum effort!”.
Sometimes, something worth doing is worth doing just a little a bit. It’s always better than nothing! Even if feels like you gained nothing from it, it’s the foundation of a habit, and the habit will grow and add up. Sometimes it may even take you by surprise…
Don’t feel like doing 20 bodyweight squats? Do literally just one. Make a deal with yourself: do just one, then you can stop if you like. Then after you’ve done one, you might think to yourself “huh, that wasn’t so bad”, and you try out a few more. Maybe after 5 you can feel your blood pumping a bit and you think “you know what, that’s enough for now”, and great, you did 5x as much exercise as you planned! Wonder what you’ll do tomorrow!
(personal note from your writer here: I’ve managed to “just extend this exercise a little bit more than last time” my way into hour-long exercise sessions before now; I started with “just 10 squats” or “just one sun salutation” etc, to get myself out of a no-exercise period that I’d slipped into, and it’s amazing how quickly adding just a little bit to the previous day’s “minimum effort!” adds up to a very respectable daily exercise session)
Wondering what a good, easy, respectable short term goal could be?
Check Out, For Example: The Seven-Minute Workout
(You might have heard of this one before; it’s an incredibly efficient well-optimized short complete workout that requires no special equipment, just a bit of floorspace and a wall—the above app allows for customizations of it per your preferences, but the basic routine is an excellent starting point for most people)
Commit to yourself (and do any self-negotiation up-front)
Really commit, though. No “or I will look silly because I told people I’d do it”, no “or I will donate x amount to charity” etc, just “I will do it and that’s that”. If you find yourself second-guessing yourself or renegotiating with yourself, just shut that down immediately and refuse to consider it.
Note: you should have break-clauses in this contract with yourself, though. For example, “unless I am ill or injured” is a sensible rule to have in advance for most exercise regimes that weren’t undertaken with your illness or injury in mind.
Make a “To-Don’t” list
Much like how addicts are often advised to not try to quit more than one thing at once, we must also be mindful of not taking on too much at once. It can be very tempting to think:
“I will turn my life around, now! I’ll quit alcohol and animal products and sugar and refined grains, and I’ll go for a run each morning, and I’ll do this and that and there, I’ve got it, here is the blueprint for my healthy perfect life from this day forth!”
And, it’s great to have any and all of that as your end goal if you want, but please, pick one or two things at most to start with, focus on those, and when those have become second nature to you and just a normal part of your life, then choose the next thing to work on.
(You can plan out the whole thing in advance if you want! i.e., I’ll do this, then this, then this, but just… make sure that you’ve really got each one down to a matter of comfort and ease before you take up the next one)
In summary:
- Focus on adding health, whatever that looks like to you
- Figure out what “minimum effort!” is for you, and let that be your baseline
- Commit to yourself (and do any self-negotiation up-front, not later)
- Decide what you’re not going to do yet, and stick to that, too.
Share This Post
- How to get a beach body: take your body to a beach. Voilà. Beach body.
Related Posts

Languishing – by Prof. Corey Keyes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about depression and “flourishing” but what about when one isn’t exactly flourishing, but is not necessarily in the depths of depression either? That’s what this book is about.
Prof. Keyes offers, from his extensive research, hope for those who do not check enough of the boxes to be considered depressed, but who are also definitely more in the lane of “surviving” than “thriving”.
Specifically, he outlines five key ways to make the step from languishing to flourishing, based not on motivational rhetoric, but actual data-based science:
- Learn (creating your personal story of self-growth)
- Connect (building relationships, on the individual level and especially on the community level)
- Transcend (developing psychological resilience to the unexpected)
- Help (others! This is about finding your purpose, and then actively living it)
- Play (this is a necessary “recharge” element that many people miss, especially as we get older)
With regard to finding one’s purpose being given the one-word summary of “help”, this is a callback to our tribal origins, and how we thrive and flourish best and feel happiest when we have a role to fulfil and provide value to those around us)
Bottom line: if you’re not at the point of struggling to get out of bed each day, but you’re also not exactly leaping out of bed with a smile, this book can help get you from one place to the other.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Microplastics found in artery plaque linked with higher risk of heart attack, stroke and death
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Microplastics and nanoplastics are everywhere in our environment – including in our oceans and lakes, farmland, and even Arctic ice algae.
Microplastics have also been found inside of us – with studies detecting them in various tissues including in the lungs, blood, heart and placenta. Understandably, concern is rising about the potential risks of microplastics on our health.
However, while a growing body of research has focused on microplastics and nanoplastics, there’s still a lack of direct evidence that their presence in human tissues is harmful to our health – and it’s uncertain if they are related to particular diseases.
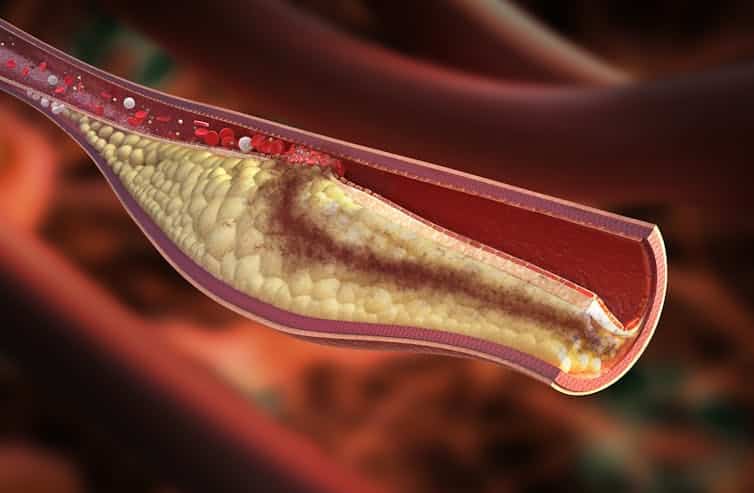
A new study has uncovered a correlation between microplastics and heart health, though. The researchers found that people who had detectable microplastics and nanoplastics in the plaque in their arteries had a higher risk of heart attack, stroke and death.
Heart health
The researchers looked at 257 people altogether. All of the patients were already undergoing preventative surgery to remove plaque from their carotid arteries (the main arteries that supply the brain with blood). This allowed the researchers to collect plaque samples and perform a chemical analysis. They then followed up with participants 34 months later.
Of the 257 participants, 150 were found to have the presence of microplastics and nanoplastics in their arterial plaque – mainly fragments of two of the most commonly used plastics in the world, polyethylene (used in grocery bags, bottles and food packaging) and polyvinyl chloride (used in flooring, cladding and pipes).
A statistical analysis of this data found that patients with microplastics and nanoplastics in their plaque had a higher risk of suffering a heart attack, stroke or death from any cause, compared with those who had no microplastics or nanoplastics in their plaque.
The researchers also analysed the macrophages (a type of immune cell that helps remove pathogens from the body) in the patients’ arteries. They found that participants who’d had microplastics and nanoplastics in their plaque also had evidence of plastic fragments in their macrophages.
They also looked at whether certain genes associated with inflammation (which can be a sign of disease) were switched on in the participants. They found that the participants who’d had microplastics and nanoplastics in their plaque also had signs of inflammation in their genes.

The microplastics were found in samples of plaque extracted from the carotid artery. Rocos/ Shutterstock These results may suggest an accumulation of nanoplastics and microplastics in carotid plaque could partly trigger inflammation. This inflammation may subsequently change the way plaque behaves in the body, making it less stable and triggering it to form a blood clot – which can eventually block blood flow, leading to heart attacks and strokes.
Interestingly, the researchers also found the presence of nanoplastics and microplastics was more common in participants who had diabetes and cardiovascular disease. This raises a lot of questions which have yet to be answered – such as why microplastics were more common in these participants, and if there may be a correlation between other diseases and the presence of microplastics in the body.
Other health risks
This study only focused on patients who had carotid artery disease and were already having surgery to remove the build-up of plaque. As such, it’s unclear whether the findings of this study can be applied to a larger population of people.
However, it isn’t the first study to show a link between microplastics and nanoplastics with poor health. Research suggests some of this harm may be due to the way microplastics and nanoplastics interact with proteins in the body.
For example, some human proteins adhere to the surface of polystyrene nanoplastics, forming a layer surrounding the nanoparticle. The formation of this layer may influence the activity and transfer of nanoplastics in human organs.
Another study suggested that nanoplastics can interact with a protein called alpha-synuclein, which in mouse studies has been shown to play a crucial role in facilitating communication between nerve cells. These clumps of nanoplastics and protein may increase the risk of Parkinson’s disease.
My published PhD research in chicken embryos found that nanoplastics may cause congenital malformations due to the way they interact with a protein called cadherin6B. Based on the interactions myself and fellow researchers saw, these malformations may affect the embryo’s eyes and neural tube, as well as the heart’s development and function.
Given the fact that nanoplastics and microplastics are found in carotid plaque, we now need to investigate how these plastics got into such tissues.
In mice, it has been demonstrated that gut macrophages (a type of white blood cell) can absorb microplastics and nanoplastics into their cell membrane. Perhaps a similar mechanism is taking place in the arteries, since nanoplastics have been identified in samples of carotid plaque macrophages.
The findings from this latest study add to a growing body of evidence showing a link between plastic products and our health. It is important now for researchers to investigate the specific mechanisms by which microplastics and nanoplastics cause harm in the body.
Meiru Wang, Postdoctoral Researcher, Molecular Biology and Nanotoxicology, Leiden University
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

From Painkillers To Hunger-Killers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Here’s this week’s selection of health news discoveries, the science behind them, what they mean for you, and where you can go from there:
Killing more than pain
It’s well-known that overuse of opioids can lead to many problems, and here’s another one: messing with the endocrine system. This time, mostly well-evidenced in men—however, the researchers are keen to point out that absence of evidence is very much not evidence of absence, hence “the hidden effects” in the headline below. It’s not that the effects are hard to see—it’s that a lot of the research has yet to be done. For now, though, we know at the very least that there’s an association between opioid use and hyperprolactinemia in men. The same research also begins to shine a light on the effects of opioid use on the hypothalamic-pituitary system and bone health, too:
Read in full: The hidden effects of opioid use on the endocrine system
Related: The 7 Approaches To Pain Management
Gut microbiome dysbiosis may lead to slipping disks
These things sound quite unconnected, but the association is strong. The likely mechanism of action is that the gut dysbiosis influences systemic inflammation, and thus spinal health—because the gut-spine axis cannot really be disconnected (while you’re alive, at least). It’s especially likely if you’re over 50 and female:
Read in full: Are back problems influenced by your gut?
Related: Is Your Gut Leading You Into Osteoporosis?
The Internet is really really great (for brains)
It’s common to see many articles on the Internet telling us, paradoxically, that we should spend less time on the Internet. However… Remember when in the 90s, it was all about “the information superhighway”? It turns out, the fact that it’s more like “the information spaghetti junction” these days doesn’t change the fact that stimulation is good for our brains, and daily Internet use improves memory, because of the different way that we index and store information that came from a virtual source. While there are parts of your brain for “things at home” and “things at the local supermarket”, there are also parts for “things at 10almonds” and “things at Facebook” and so forth. You are, in effect, building a vast mental library as you surf:
Read in full: Daily internet use supercharges your memory!
Related: Make Social Media Work For Your Mental Health
Fall back
Around this time of year in many places in the Northern Hemisphere, the clocks go back an hour (it’s next weekend in the US and Canada, by the way, and this weekend in most of Europe). Many enjoy this as the potential for an extra hour’s sleep, but for night owls, it can be more of a nuisance than a benefit—throwing out what’s often an already difficult relationship with the clock, and presenting challenges both practical and physiological (different processing of melatonin, for instance). Here be science:
Read in full: Why night owls struggle more when the clocks go back
Related: Early Bird Or Night Owl? Genes vs Environment
Can you outrun your hunger?
It seems so, though benefits are strongest in women. We say “outrun”, though this study did use stationary cycling. To put it in few words, intense exercise (but not moderate exercise) significantly reduced acylated ghrelin (hunger hormone) levels, and subjective reports of hunger, especially in women:
Read in full: Study finds intense exercise may suppress appetite in healthy humans
Related: 3 Appetite Suppressants Better Than Ozempic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: