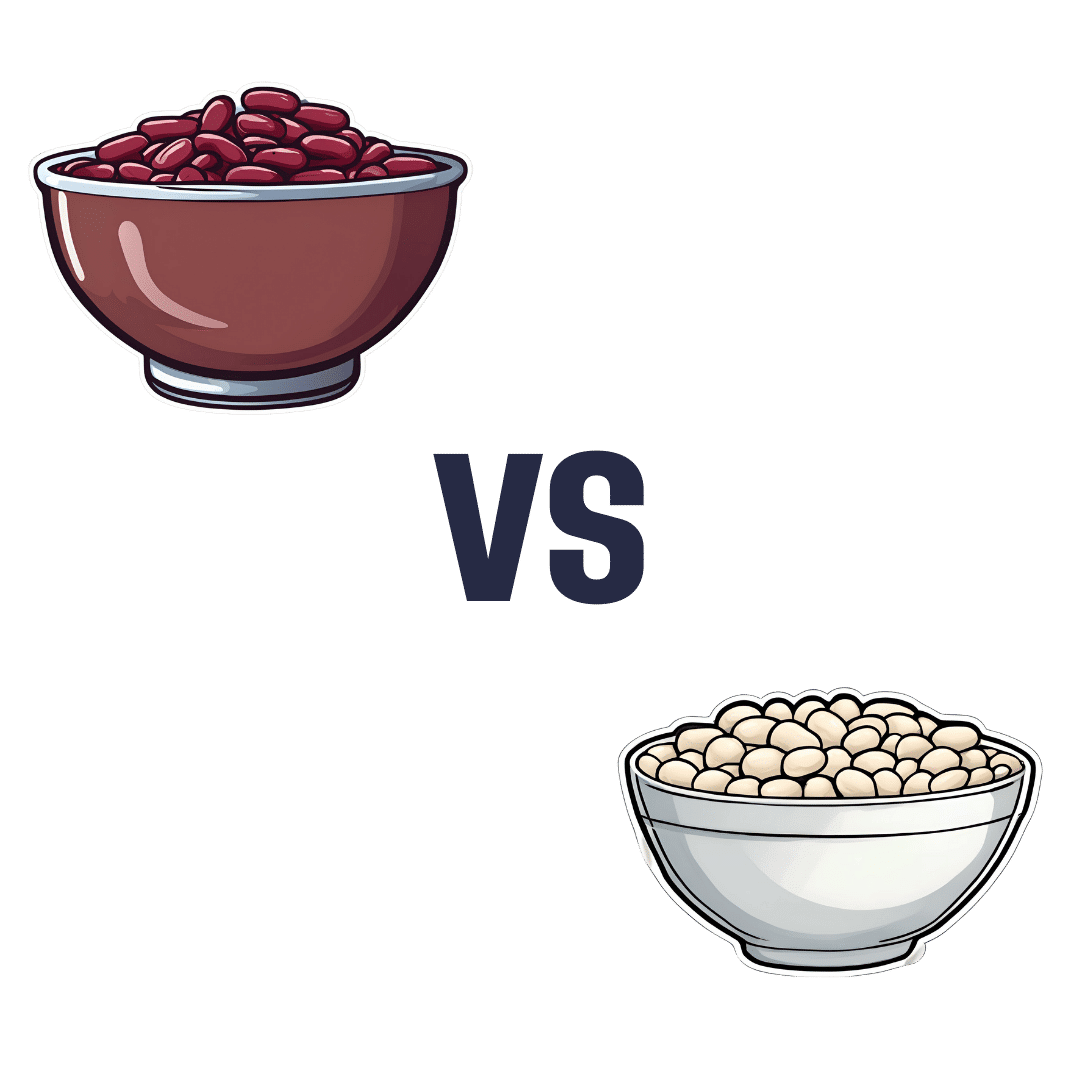
Kidney Beans vs White Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to white beans, we picked the white.
Why?
It was close, and each has its strengths! Bear in mind, these are very closely-related beans. But as we say, there are distinguishing factors…
In terms of macros, kidney beans have very slightly more fiber and white beans have very slightly more protein. But both are close enough in both of those things to call this a tie in this category.
When it comes to vitamins, there are two ways of looking at this:
- kidney beans have more of vitamins B1, B2, B3, B6, B9, C, and K, while white beans have more vitamin B5, E, and choline
- kidney beans have slightly more of some vitamins that don’t usually see a deficiency, while white beans have 31x more vitamin E
Nevertheless, we’re sticking by our usual method of noting that this is a 7:3 win for kidney beans in this category; we just wanted to note that in practical health terms, an argument can be made for white beans on the vitamin front too.
In the category of minerals, kidney beans have slightly more phosphorus, while white beans have more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. An easy win for white beans this time.
(In case you’re wondering about the margin on phosphorus, it was 0.2x more, so we’re not seeing a situation like white beans’ 31x more vitamin E)
In short: both are great and both have their strengths. Enjoy both, together if you like! But if we have to pick one, we’re going with white beans.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can I Eat That? – by Jenefer Roberts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The answer to the question in the title is: you can eat pretty much anything, if you’re prepared for the consequences!
This book looks to give you the information to make your own decisions in that regard. There’s a large section on the science of glucose metabolism in the context of food (other aspects of glucose metabolism aren’t covered), so you will not simply be told “raw carrots are good; mashed potatoes are bad”, you’ll understand many factors that affect it, e.g:
- Macronutrient profiles of food and resultant base glycemic indices
- How the glycemic index changes if you cut something, crush it, mash it, juice it, etc
- How the glycemic index changes if you chill something, heat it, fry it, boil it, etc
- The many “this food works differently in the presence of this other food” factors
- How your relative level of insulin resistance affects things itself
…and much more.
The style is simple and explanatory, without deep science, but with good science and comprehensive advice.
There are also the promised recipes; they’re in an appendix at the back and aren’t the main meat of the book, though.
Bottom line: if you’ve ever found it confusing working out what works how in the mysterious world of diabetes nutrition, this book is a top tier demystifier.
Click here to check out Can I Eat That?, and gain confidence in your food choices!
Share This Post
-
The Uses of Delusion – by Dr. Stuart Vyse
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us try to live rational lives. We try to make the best decisions we can based on the information we have… And if we’re thoughtful, we even try to be aware of common logical fallacies, and overcome our personal biases too. But is self-delusion ever useful?
Dr. Stuart Vyse, psychologist and Fellow for the Committee for Skeptical Inquiry, argues that it can be.
From self-fulfilling prophecies of optimism and pessimism, to the role of delusion in love and loss, Dr. Vyse explores what separates useful delusion from dangerous irrationality.
We also read about such questions as (and proposed answers to):
- Why is placebo effect stronger if we attach a ritual to it?
- Why are negative superstitions harder to shake than positive ones?
- Why do we tend to hold to the notion of free will, despite so much evidence for determinism?
The style of the book is conversational, and captivating from the start; a highly compelling read.
Bottom line: if you’ve ever felt yourself wondering if you are deluding yourself and if so, whether that’s useful or counterproductive, this is the book for you!
Click here to check out The Uses of Delusion, and optimize yours!
Share This Post
-
Astrology, Mental health and the Economics of Well Being
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ultimately can the mental health system single-handedly address the concerns of inequality and economic access in society?
Around 75 per cent of the Indian population lives in rural areas, but their access to quality mental health care is limited and traditional approaches continue to be in use. The shortage is to such a large extent that there are only 0.7 physicians per 1000 population and only one psychiatrist for every 343,000 Indians. While over the years the mental health sector has seen major developments, like the 2017 mental health care act. This act establishes equal access for all citizens, to avail government-run or funded mental health services in the country. However, it does not bridge the gap in society as the majority of the population remains deeply unaware or unable to access these services.
While the uncertainties of the pandemic brought mental wellbeing to the forefront, the national budget for the sector dropped, making this an issue of human rights. This accessibility to services is further corroborated by the recurring financial expenses of medications and frequent visits to government clinics. The cost of sessions is steep and a single session is not ideal. Spending exorbitant amounts on healthcare is a burden most families can’t afford leading to debt. In the absence of insurance and healthcare schemes and provisions, therapy remains a luxury to many Indians.
Economic struggles are only one of the causes of this discerning gap in the mental health sector. Barriers caused by sexuality, gender, caste and religion also play a major role in mediating people’s perception and access to therapeutic services. The persistent stigma surrounding mental health, especially in India continues to be a hindrance to seeking help. The supernatural inhibitions and disparity in knowledge across communities only create more confusion. The notion that mental well being is an optional expense is popular, even though the country’s population is in a dire state. Data collected in a WHO report found that nearly 15 per cent of Indian adults need active intervention for one or more mental health issues.
The population disregards the very prevalence of such mental disorders and more than often finds it fruitless to receive treatment. Some who are open-minded fail to afford the hiked fees that therapists in urban settings charge, leaving them with no option. While for years Indians attributed the systemic weakness of the mental health system to the people’s attitudes, a 2016 survey showed more than 42% of people have positive attitudes toward mental wellbeing and treatment. While the skeptics remain, these underprivileged sections of society too struggle to gain the accessibility they deserve.
This is where astrology, tarot card reading and other spiritual practices, have created a market for themselves in the well-being industry. The sceptics, and those from poor socio-economic backgrounds resort to these local and easily accessible ways of coping, to instil the faith they so desperately need. Astrology is a layman’s substitute for therapy, or for some even a supplement when they cannot afford extended periods of treatment. Visiting a local astrologer in many ways breeds the self-awareness one would expect from a session in therapy. These practices even hold certain similarities to actual psychotherapy settings, in the way they define, and alleviate aspects of one’s personality and behaviour.
Very often one simply needs an explanation, or an answer to the ‘why’ no matter how scientifically rooted that response truly is. Astrologers impart a level of faith, that things will get better. For those in rural areas, struggling to provide the bare necessities to their family affording therapy is impossible, so their local psychic, astrologer or pandit becomes their anchor during emotional duress. Tarot cards and other practices primarily focus on the future and act as a guide point for how to deal with the things ahead. For a farmer coping with anxiety, access to anti-anxiety medication is strained, and so is therapy. His best bet remains to consult his next-door jyotish about his burdens.
A famous clinician Caroline Hexdall in an interview said that “ Part of the popularity of astrology and tarot today has to do with their universal nature”. With growing technology and the pervasiveness of social media, people can gain easy access to self-care and astrology resources. Apps and web pages provide daily tarot cards, zodiac signs readings and astrological predictions for people, and almost serve the purpose of a therapist. Is reading the lines on our palm, and checking the alignment of the stars enough to cure the mental illness they undergo? Is it a solution or a quick fix as a consequence of an ignorant healthcare system?
Several studies have also shown the deteriorating effects of depending on astrology. Cases of worsening and onset of depression, anxiety and personality disorders are common for those who use astrology as more than just a temporary coping mechanism. It also becomes a source of losing control, as every feeling is attributed to fate and destiny, instilling a sense of helplessness. Ultimately can the mental health system single-handedly address the concerns of inequality and economic access in society?
Maahira Jain is a third-year student at Ashoka University studying Psychology and Media studies. She is a movie buff and is extremely passionate about writing and traveling.
This article is republished from OpenAxis under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
The New Menopause – by Dr. Mary Claire Haver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is most famous for “The Galveston Diet”, which book is astonishingly similar in its content, chapters, format, etc to Nikki Williams’ “It’s Not You, It’s Your Hormones” which came out a few years previously but didn’t get the same marketing.
Nonetheless, this time Dr. Haver has something new to add, and we think it’s worth a read.
The general theme of this book is a comprehensive overview of the menopause, experientially (subjective to the person going through it) and empirically (by science), from start to finish and beyond. This book’s more about human physiology, and less about diet than the previous.
Dr. Haver also discusses in-depth how estrogen is thought of as a sex hormone (and it is), to the point that people consider it perhaps expendable, and forget (or are simply unaware) that we have estrogen receptors throughout our bodies and estrogen is vital for maintaining many other bodily functions, including your heart, cognitive function, bone integrity, blood sugar balance, and more.
(in case you’re wondering “why don’t men fall to bits, then?”, don’t worry, their testosterone does these things for them. Testosterone is orders of magnitude less potent than estrogen, mg for mg, so they need a lot more of it, but under good conditions they produce plenty so it’s fine)
But, the amount of testosterone available to peri/postmenopausal women is simply not enough to do that job (and it’d also result in a transition of secondary sex characteristics, which for most people would be very unwanted), so, something else needs to be done.
Dr. Haver also discusses in detail the benefits and risks of HRT and how to get/manage them, respectively, with the latest up-to-date research (at time of going to print; the book was published in April 2024).
Bottom line: if you want to know what’s going on with your peri- or post-menopausal body and how it could be better (or if you want to know what’s going on with someone else approaching/experiencing menopause), then this is a top-tier book.
Click here to check out The New Menopause, and know what’s going on and what to do about it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eating on the Wild Side: – by Jo Robinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is an investigative journalist, and it shows here, as she leaves no stone unturned in her quest for the truth in the face of many food myths.
She covers a lot of “popular wisdom” things that are varyingly true or false, or sometimes even both—in the case of food lore that’s a good rule of thumb, but has notable exceptions (e.g. “more colorful and/or darker-colored fruits/vegetables contain more nutrients”, which is a very good rule of thumb until one meets a cauliflower, for example).
She also covers food preparation myths, and how, to give one example, in spite of the popularity of “less cooked is better”, in some cases certain cooking methods will indeed destroy nutrients; in others, certain cooking methods will improve nutritional availability. Either by destroying an adjacent antinutrient (e.g. phytates), or by breaking something down into a more manageable form that our body can absorb. Knowing which is which, is important.
The book is organized by kinds of food, and does exclusively cover plants, but there’s more than enough material for any omnivore to enjoy.
The style is… Journalistic, it would be fair to say. Which is not surprising, given the author. But it means that it is written in a fairly narrative way, to draw the reader in and make it an enjoyable read while still being informative in all parts (there is no padding). In terms of science, the in-the-prose science is as minimal as possible to still convey what needs to be conveyed, while 25 pages of bibliography stack up at the end to show that indeed, this journalist cites sources.
Bottom line: this is a really enjoyable book, packed with a wealth of knowledge, and is perfect to uplift your cooking by knowing your ingredients a little more intimately!
Click here to check out Eating On The Wild Side, and, enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Fiber Fueled Cookbook – by Dr. Will Bulsiewicz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bulsiewicz’s book “Fiber Fuelled” (which is great), but this one is more than just a cookbook with the previous book in mind. Indeed, this is even a great stand-alone book by itself, since it explains the core principles well enough already, and then adds to it.
It’s also about a lot more than just “please eat more fiber”, though. It looks at FODMAPs, purine, histamine intolerance, celiac disease, altered gallbladder function, acid reflux, and more.
He offers a five-part strategy:
Genesis (what is the etiology of your problem)
- Restrict (cut things out to address that first)
- Observe (keep a food/symptom diary)
- Work things back in (re-add potential triggers one by one, see how it goes)
- Train your gut (your microbiome does not exist in a vacuum, and communication is two-way)
- Holistic healing (beyond the gut itself, looking at other relevant factors and aiming for synergistic support)
As for the recipes themselves, there are more than a hundred of them and they are good, so no more “how can I possibly cook [favorite dish] without [removed ingredient]?”
Bottom line: if you’d like better gut health, this book is a top-tier option for fixing existing complaints, and enjoying plain-sailing henceforth.
Click here to check out The Fiber Fueled Cookbook; your gut will thank you later!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: