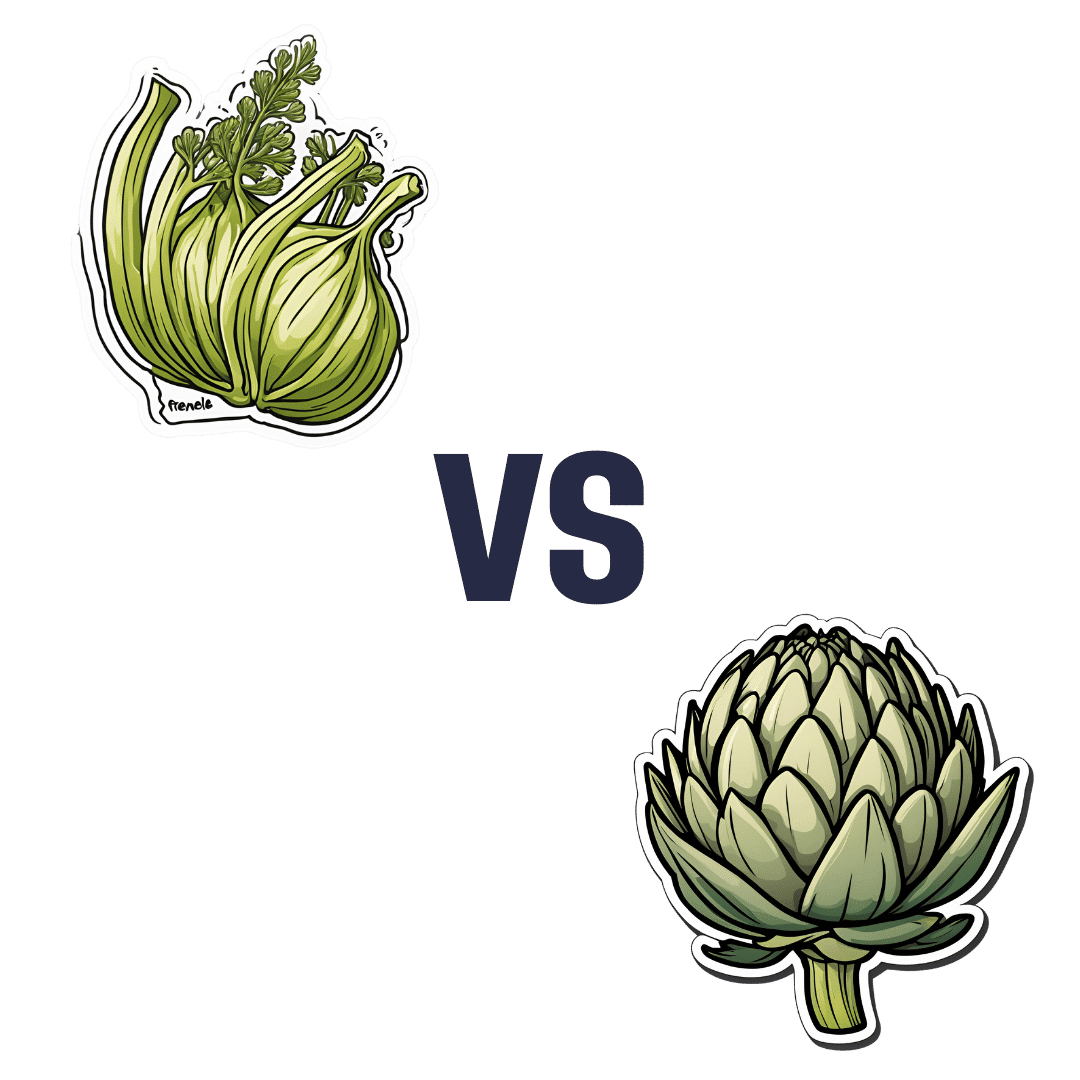
Fennel vs Artichoke – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fennel to artichoke, we picked the artichoke.
Why?
Both are great! But artichoke wins on nutritional density.
In terms of macros, artichoke has more protein and more fiber, for only slightly more carbs.
Vitamins are another win for artichoke, boasting more of vitamins B1, B2, B3, B5, B6, B9, and choline. Meanwhile, fennel has more of vitamins A, E, and K, which is also very respectable but does allow artichoke a 6:3 lead.
In the category of minerals, artichoke has a lot more copper, iron, magnesium, manganese, and phosphorus, while fennel has a little more calcium, potassium, and selenium.
One other relevant factor is that fennel is a moderate appetite suppressant, which may be good or bad depending on your food-related goals.
All in all though, we say the artichoke wins by virtue of its greater abundance of nutrients!
Want to learn more?
You might like to read:
What Matters Most For Your Heart? ← appropriately enough, with fennel hearts and artichoke hearts!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Simple Wall Pilates for Seniors – by Grace Clark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While the cover illustration makes this look a little too simple, in fact there’s a lot of value in this book, with exercises ranging from things like that on the cover, to the “wall downward dog”. But the actual exercises (of which there are 29) themselves are only a part of the book (taking about 70 pages of it with clear illustrations).
There’s also a lot about important Pilates principles to apply, such as breathing, correct body alignment (if you don’t already do Pilates, you will not have this, as Pilates alignment is quite specific), flexibility, balance, stability, coordination, range of motion, isometric exercise considerations, endurance, and more.
Unlike a lot of “…for seniors” books, this is not a watered down barely-does-anything version of the “real” exercises, but rather, would present most the same challenges to a 20-year-old reader; it’s just that the focus here is more on matters that tend to concern an older rather than younger demographic. That 20-something may be busy building their butt, for instance, while the 80-year-old is building their bones. No reason both shouldn’t do both, of course, but the focus is age-specific.
The author guides us through working up from easy things to hard, breaking stuff down so that we can progress at our own pace, such that even the most cautious or enthusiastic reader can start at an appropriate point and proceed accordingly.
She also talks us through a 28-day program (as promised by the subtitle), and advice on how to keep it going without plateauing, how to set realistic goals, how to tailor it to our abilities as we go, track our progress, and so forth.
The style is clear and instructional, and one thing that sets this apart from a lot of Pilates books is that the education comes from an angle not of “trust me”, but rather from well-sourced claims with bibliography whose list spans 5 pages at the end.
Bottom line: if you’d like to progressively increase your strength, stability, and more—with no gym equipment, just a wall—then this book will have you see improvements in the 28 days it promises, and thereafter.
Click here to check out Simple Wall Pilates For Seniors, and experience the difference!
Share This Post
-
Calm For Surgery – by Dr Chris Bonney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As a general rule of thumb, nobody likes having surgery. We may like the results of the surgery, we may like having the surgery done and behind us, but surgery itself is not most people’s idea of fun, and honestly, the recovery period afterwards can be a pain in every sense of the word.
Dr. Chris Bonney, an anesthesiologist, gives us the industry-secrets low-down, and is the voice of experience when it comes to the things to know about and/or prepare in advance—the little things that make a world of difference to your in-hospital experience and afterwards.
Think of it like “frequent flyer traveller tips” but for surgeries, whereupon knowing a given tip can mean the difference between deeply traumatic suffering and merely not being at your usual best. We think that’s worth it.
Share This Post
-
Tasty Hot-Or-Cold Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Full of fiber as well as vitamins and minerals, this versatile “serve it hot or cold” soup is great whatever the weather—give it a try!
You will need
- 1 quart low-sodium vegetable stock—ideally you made this yourself from vegetable offcuts you kept in the freezer until you had enough to boil in a big pan, but failing that, a large supermarket will generally be able to sell you low-sodium stock cubes.
- 2 medium potatoes, peeled and diced
- 2 leeks, chopped
- 2 stalks celery, chopped
- 1 large onion, diced
- 1 large carrot, diced, or equivalent small carrots, sliced
- 1 zucchini, diced
- 1 red bell pepper, diced
- 1 tsp rosemary
- 1 tsp thyme
- ¼ bulb garlic, minced
- 1 small piece (equivalent of a teaspoon) ginger, minced
- 1 tsp red chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp turmeric
- Extra virgin olive oil, for frying
- Optional: ½ tsp MSG or 1 tsp low-sodium salt
About the MSG/salt: there should be enough sodium already from the stock and potatoes, but in case there’s not (since not all stock and potatoes are made equal), you might want to keep this on standby.
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, and add the diced onion, frying until it begins to soften.
2) Add the ginger, potato, carrot, and leek, and stir for about 5 minutes. The hard vegetables won’t be fully cooked yet; that’s fine.
3) Add the zucchini, red pepper, celery, and garlic, and stir for another 2–3 minutes.
4) Add the remaining ingredients; seasonings first, then vegetable stock, and let it simmer for about 15 minutes.
5) Check the potatoes are fully softened, and if they are, it’s ready to serve if you want it hot. Alternatively, let it cool, chill it in the fridge, and enjoy it cold:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits? ← 5/5 in our recipe today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
Related Posts
-
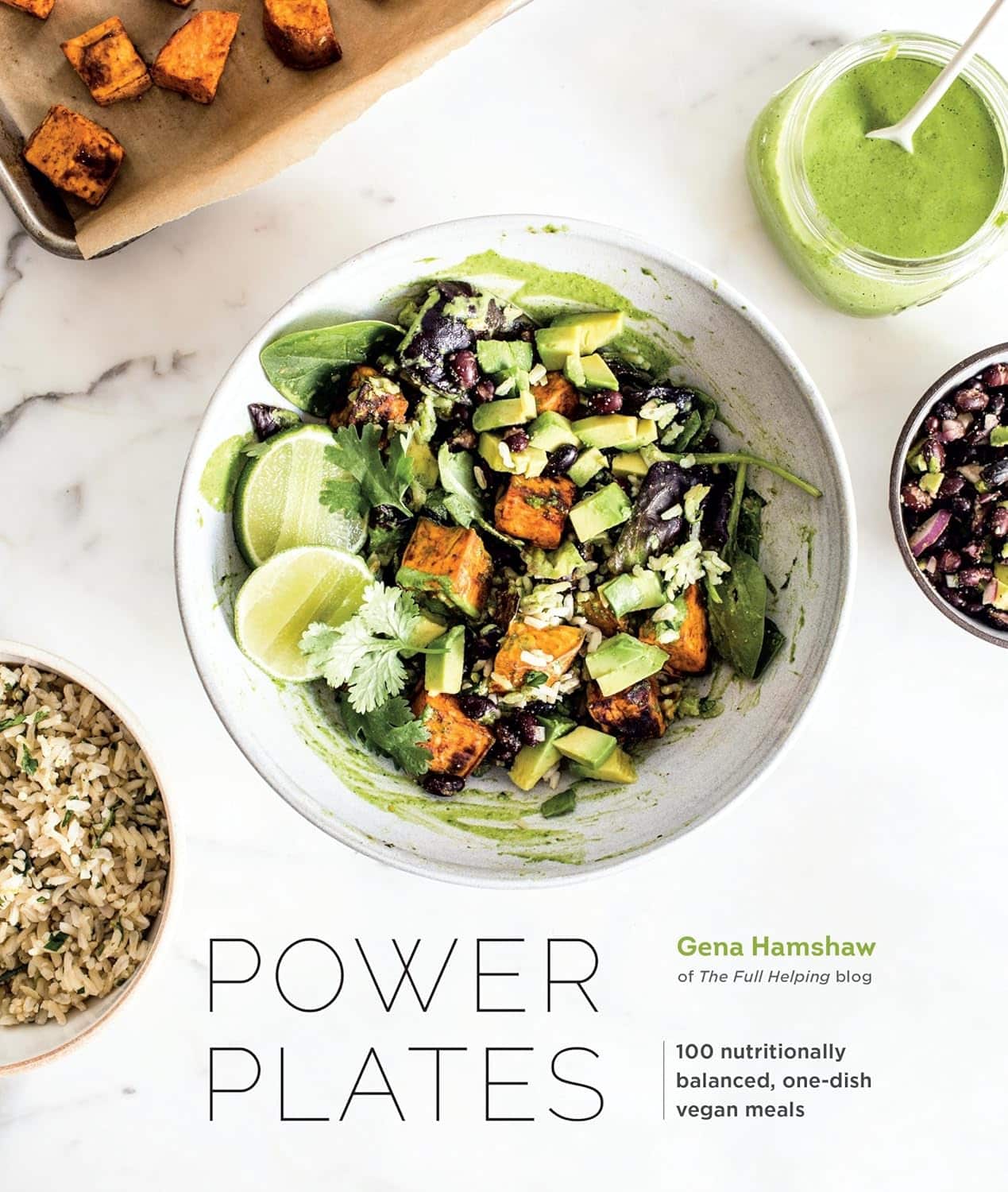
Power Plates – by Gena Hamshaw
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods are all well and good, but there are only so many ways one can reasonably include watercress before it starts becoming a chore.
Happily, Gena Hamshaw is here with a hundred single-dish vegan meals, that are not only nutritionally balanced as the subtitle promises, but also, as the title suggests, are nutritional powerhouses too.
In the category of criticism, some ingredients are not so universally available as others. For example, depending on where you live, your local supermarket might not have freekeh, gochujang, or pomegranate molasses.
However, most of the recipes have ingredients that are easy enough to source in any medium-sized supermarket, and for the ones that aren’t, we do recommend ordering the ingredient online and trying something you might not otherwise have experienced—that’s an important thing in life, after all!
Bottom line: if you’d like plant-based meals that are packed full of nutrients and are delicious too, this is a top-tier recipe book.
Click here to check out Power Plates, and enjoy a wide variety of plant-based cuisine!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Actually Start A Healthy Lifestyle In The New Year
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Faye Bate cuts through the trends to give advice that’ll last past January the 2nd:
What actually works
…and is actually easy to implement:
Avoid an All-or-Nothing Mindset
- Strict, perfectionist approaches often lead to failure and guilt.
- Small, balanced efforts can be imperfect without being failures!
- Sustainable habits should integrate seamlessly into daily life..
Focus on Unprocessed vs. Processed Foods
- Don’t worry overly about calorie counts unless you have a very specific medical reason to do so.
- Prioritize minimally processed, nutrient-dense foods over highly processed, empty-calorie-dense options.
- Moderation is key—processed foods don’t need to be eliminated entirely; taking things down by just one tier of processing is already an improvement.
Choose Enjoyable Exercise
- The best exercise is one you enjoy and can maintain long-term. If something’s not enjoyable, you’ll soon give it up.
- Trends in fitness shouldn’t dictate your routine—do what works for you.
- Same goes for “body goals”—fashions come and go, while you’re still going to have more or less the same basic body, so work with it rather than against it.
Prioritize Convenience
- Convenience plays a critical role in maintaining healthy habits, for similar reasons to the enjoyment (very few people enjoy inconvenience)
- Example from Dr. Bate: switching to a closer gym led to consistent workouts despite a busy schedule.
- Apply the same principle to food: plan ahead and stock convenient, healthy options (e.g. frozen vegetables etc).
Keep It Simple
- Do follow basic health advice: drink water, eat fruits and vegetables, move your body, and see a doctor if needed.
- Avoid being swayed by sensationalized health trends and headlines designed to sell products—if you want it for a good while first, then maybe you’ll actually use it more than twice.
- Stick to evidence-based, straightforward habits for long-term health. And check the evidence for yourself! Do not just believe claims!
In short: you will more likely tend to do things that are enjoyable and not too difficult. Start there and work up, keeping things simple along the way. It doesn’t matter if it’s not how everyone else does it; if it works for you, it works for you!
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Science Of New Year’s Pre-Resolutions
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
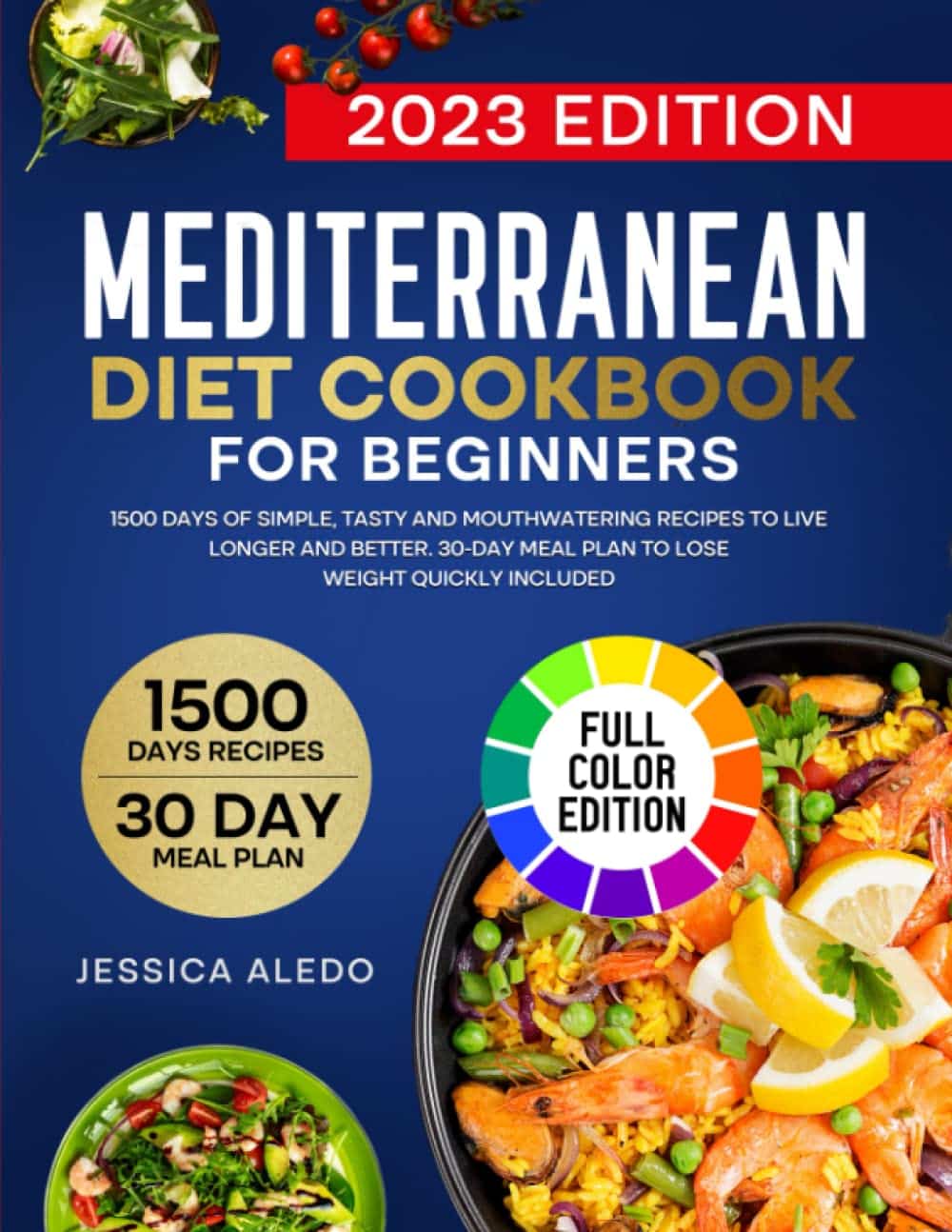
The Mediterranean Diet Cookbook for Beginners – by Jessica Aledo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of Mediterranean Diet books on the market, and not all of them actually stick to the Mediterranean Diet. There’s a common mistake of thinking “Well, this dish is from the Mediterranean region, so…”, but that doesn’t make, for example, bacon-laden carbonara part of the Mediterranean Diet!
Jessica Aledo does better, and sticks unwaveringly to the Mediterranean Diet principles.
First, she gives a broad introduction, covering:
- The Mediterranean Diet pyramid
- Foods to eat on the Mediterranean Diet
- Foods to avoid on the Mediterranean Diet
- Benefits of the Mediterranean Diet
Then, it’s straight into the recipes, of which there are 201 (as with many recipe books, the title is a little misleading about this).
They’re divided into sections, thus:
- Breakfasts
- Lunches
- Snacks
- Dinners
- Desserts
The recipes are clear and simple, one per double-page, with high quality color illustrations. They give ingredients/directions/nutrients. There’s no padding!
Helpfully, she does include a shopping list as an appendix, which is really useful!
Bottom line: if you’re looking to build your Mediterranean Diet repertoire, this book is an excellent choice.
Get your copy of The Mediterranean Diet Cookbook for Beginners from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: