Qigong: A Breath Of Fresh Air?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Qigong: Breathing Is Good (Magic Remains Unverified)
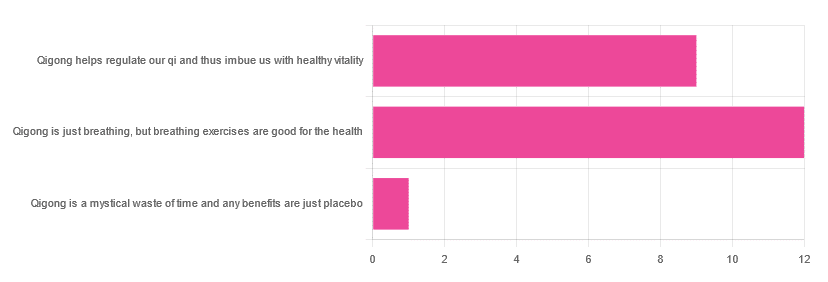
In Tuesday’s newsletter, we asked you for your opinions of qigong, and got the above-depicted, below-described, set of responses:
- About 55% said “Qigong is just breathing, but breathing exercises are good for the health”
- About 41% said “Qigong helps regulate our qi and thus imbue us with healthy vitality”
- One (1) person said “Qigong is a mystical waste of time and any benefits are just placebo”
The sample size was a little low for this one, but the results were quite clearly favorable, one way or another.
So what does the science say?
Qigong is just breathing: True or False?
True or False, depending on how we want to define it—because qigong ranges in its presentation from indeed “just breathing exercises”, to “breathing exercises with visualization” to “special breathing exercises with visualization that have to be exactly this way, with these hand and sometimes body movements also, which also must be just right”, to far more complex definitions that involve qi by various mystical definitions, and/or an appeal to a scientific analog of qi; often some kind of bioelectrical field or such.
There is, it must be said, no good quality evidence for the existence of qi.
Writer’s note, lest 41% of you want my head now: I’ve been practicing qigong and related arts for about 30 years and find such to be of great merit. This personal experience and understanding does not, however, change the state of affairs when it comes to the availability (or rather, the lack) of high quality clinical evidence to point to.
Which is not to say there is no clinical evidence, for example:
Acute Physiological and Psychological Effects of Qigong Exercise in Older Practitioners
…found that qigong indeed increased meridian electrical conductance!
Except… Electrical conductance is measured with galvanic skin responses, which increase with sweat. But don’t worry, to control for that, they asked participants to dry themselves with a towel. Unfortunately, this overlooks the fact that a) more sweat can come where that came from, because the body will continue until it is satisfied of adequate homeostasis, and b) drying oneself with a towel will remove the moisture better than it’ll remove the salts from the skin—bearing in mind that it’s mostly the salts, rather than the moisture itself, that improve the conductivity (pure distilled water does conduct electricity, but not very well).
In other words, this was shoddy methodology. How did it pass peer review? Well, here’s an insight into that journal’s peer review process…
❝The peer-review system of EBCAM is farcical: potential authors who send their submissions to EBCAM are invited to suggest their preferred reviewers who subsequently are almost invariably appointed to do the job. It goes without saying that such a system is prone to all sorts of serious failures; in fact, this is not peer-review at all, in my opinion, it is an unethical sham.❞
~ Dr. Edzard Ernst, a founding editor of EBCAM (he since left, and decries what has happened to it since)
One of the other key problems is: how does one test qigong against placebo?
Scientists have looked into this question, and their answers have thus far been unsatisfying, and generally to the tune of the true-but-unhelpful statement that “future research needs to be better”:
Problems of scientific methodology related to placebo control in Qigong studies: A systematic review
Most studies into qigong are interventional studies, that is to say, they measure people’s metrics (for example, blood pressure, heart rate, maybe immune function biomarkers, sleep quality metrics of various kinds, subjective reports of stress levels, physical biomarkers of stress levels, things like that), then do a course of qigong (perhaps 6 weeks, for example), then measure them again, and see if the course of qigong improved things.
This almost always results in an improvement when looking at the before-and-after, but it says nothing for whether the benefits were purely placebo.
We did find one study that claimed to be placebo-controlled:
…but upon reading the paper itself carefully, it turned out that while the experimental group did qigong, the control group did a reading exercise. Which is… Saying how well qigong performs vs reading (qigong did outperform reading, for the record), but nothing for how well it performs vs placebo, because reading isn’t a remotely credible placebo.
See also: Placebo Effect: Making Things Work Since… Well, A Very Long Time Ago ← this one explains a lot about how placebo effect does work
Qigong is a mystical waste of time: True or False?
False! This one we can answer easily. Interventional studies invariably find it does help, and the fact remains that even if placebo is its primary mechanism of action, it is of benefit and therefore not a waste of time.
Which is not to say that placebo is its only, or even necessarily primary, mechanism of action.
Even from a purely empirical evidence-based medicine point of view, qigong is at the very least breathing exercises plus (usually) some low-impact body movement. Those are already two things that can be looked at, mechanistic processes pointed to, and declarations confidently made of “this is an activity that’s beneficial for health”.
See for example:
- Effects of Qigong practice in office workers with chronic non-specific low back pain: A randomized control trial
- Qigong for the Prevention, Treatment, and Rehabilitation of COVID-19 Infection in Older Adults
- Impact of Medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial
…and those are all from respectable journals with meaningful peer review processes.
None of them are placebo-controlled, because there is no real option of “and group B will only be tricked into believing they are doing deep breathing exercises with low-impact movements”; that’s impossible.
But! They each show how doing qigong reliably outperforms not doing qigong for various measurable metrics of health.
And, we chose examples with physical symptoms and where possible empirically measurable outcomes (such as COVID-19 infection levels, or inflammatory responses); there are reams of studies showings qigong improves purely subjective wellbeing—but the latter could probably be claimed for any enjoyable activity, whereas changes in inflammatory biomarkers, not such much.
In short: for most people, it indeed reliably helps with many things. And importantly, it has no particular risks associated with it, and it’s almost universally framed as a complementary therapy rather than an alternative therapy.
This is critical, because it means that whereas someone may hold off on taking evidence-based medicines while trying out (for example) homeopathy, few people are likely to hold off on other treatments while trying out qigong—since it’s being viewed as a helper rather than a Hail-Mary.
Want to read more about qigong?
Here’s the NIH’s National Center for Complementary and Integrative Health has to say. It cites a lot of poor quality science, but it does mention when the science it’s citing is of poor quality, and over all gives quite a rounded view:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
CLA for Weight Loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Conjugated Linoleic Acid for Weight Loss?
You asked us to evaluate the use of CLA for weight loss, so that’s today’s main feature!
First, what is CLA?
Conjugated Linoleic Acid (CLA) is a fatty acid made by grazing animals. Humans don’t make it ourselves, and it’s not an essential nutrient.
Nevertheless, it’s a popular supplement, mostly sold as a fat-burning helper, and thus enjoyed by slimmers and bodybuilders alike.
❝CLA reduces bodyfat❞—True or False?
True! Contingently. Specifically, it will definitely clearly help in some cases. For example:
- This study found it doubled fat loss in chickens
- It significantly increased delipidation of white adipose tissue in these mice
- The mice in this study enjoyed a 43–88% reduction in (fatty) weight gain
- Over the course of a six-week weight-loss program, these mice got 70% more weight loss on CLA, compared to placebo
- In this study, pigs that took CLA on a high-calorie diet gained 50% less weight than those not taking CLA
- On a heart-unhealthy diet, these hamsters taking CLA gained much less white adipose tissue than their comrades not taking CLA
- Another study with pigs found that again, CLA supplementation resulted in much less weight gained
- These hamsters being fed a high-cholesterol diet found that those taking CLA ended up with a leaner body mass than those not taking CLA
- This study with mice found that CLA supplementation promoted fat loss and lean muscle gain
Did you notice a theme? It’s Animal Farm out there!
❝CLA reduces bodyfat in humans❞—True or False?
False—practically. Technically it appears to give non-significantly better results than placebo.
A comprehensive meta-analysis of 18 different studies (in which CLA was provided to humans in randomized, double-blinded, placebo-controlled trials and in which body composition was assessed by using a validated technique) found that, on average, human CLA-takers lost…
Drumroll please…
00.00–00.05 kg per week. That’s between 0–50g per week. That’s less than two ounces. Put it this way: if you were to quickly drink an espresso before stepping on the scale, the weight of your very tiny coffee would cover your fat loss.
The reviewers concluded:
❝CLA produces a modest loss in body fat in humans❞
Modest indeed!
See for yourself: Efficacy of conjugated linoleic acid for reducing fat mass: a meta-analysis in humans
But what about long-term? Well, as it happens (and as did show up in the non-human animal studies too, by the way) CLA works best for the first four weeks or so, and then effects taper off.
Another review of longer-term randomized clinical trials (in humans) found that over the course of a year, CLA-takers enjoyed on average a 1.33kg total weight loss benefit over placebo—so that’s the equivalent of about 25g (0.8 oz) per week. We’re talking less than a shot glass now.
They concluded:
❝The evidence from RCTs does not convincingly show that CLA intake generates any clinically relevant effects on body composition on the long term❞
A couple of other studies we’ll quickly mention before closing this section:
- CLA supplementation does not affect waist circumference in humans (at all).
- Amongst obese women doing aerobic exercise, CLA supplementation has no effect (at all) on body fat reduction compared to placebo
What does work?
You may remember this headline from our “What’s happening in the health world” section a few days ago:
Research reveals self-monitoring behaviors and tracking tools key to long-term weight loss success
On which note, we’ve mentioned before, we’ll mention again, and maybe one of these days we’ll do a main feature on it, there’s a psychology-based app/service “Noom” that’s very personalizable and helps you reach your own health goals, whatever they might be, in a manner consistent with any lifestyle considerations you might want to give it.
Curious to give it a go? Check it out at Noom.com (you can get the app there too, if you want)
Share This Post
-
The Diet Myth – by Dr. Tim Spector
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why are we supposed to go low-carb, but get plenty of whole grains? Avoid saturated fat, but olive oil is one of the healthiest fats around? Will cheese kill us or save us? Even amongst the well-informed, there’s a lot of confusion. This book addresses these and many such topics.
A main theme of the book is howa lot of it relates to the state of our gut microbiome, and what is good or bad for that. He also discusses, for example, how microbes predict obesity better than genes, and the good news is: we can change our microbes a lot more easily than we can change our genes!
In the category of criticism, he repeats some decades-old bad science in some areas outside of his field (i.e. unrelated to nutrition), so that’s unfortunate, and/but doesn’t detract from the value of the book if we keep to the main topic.
Bottom line: if you’d like to understand better the physiology and microbiology behind why dieting does work for most people (and how to do it better), then this is a great book for that.
Click here to check out The Diet Myth, and learn the science behind the confusion!
Share This Post
-
Woman Petitions Health Insurer After Company Approves — Then Rejects — Her Infusions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When KFF Health News published an article in August about the “prior authorization hell” Sally Nix said she went through to secure approval from her insurance company for the expensive monthly infusions she needs, we thought her story had a happy ending.
That’s because, after KFF Health News sent questions to Nix’s insurance company, Blue Cross Blue Shield of Illinois, it retroactively approved $36,000 worth of treatments she thought she owed. Even better, she also learned she would qualify for the infusions moving forward.
Good news all around — except it didn’t last for long. After all, this is the U.S. health care system, where even patients with good insurance aren’t guaranteed affordable care.
To recap: For more than a decade, Nix, of Statesville, North Carolina, has suffered from autoimmune diseases, chronic pain, and fatigue, as well as a condition called trigeminal neuralgia, which is marked by bouts of electric shock-like pain that’s so intense it’s commonly known as the “suicide disease.”
“It is a pain that sends me to my knees,” Nix said in October. “My entire family’s life is controlled by the betrayal of my body. We haven’t lived normally in 10 years.”
Late in 2022, Nix started receiving intravenous immunoglobulin infusions to treat her diseases. She started walking two miles a day with her service dog. She could picture herself celebrating, free from pain, at her daughter’s summer 2024 wedding.
“I was so hopeful,” she said.
But a few months after starting those infusions, she found out that her insurance company wouldn’t cover their cost anymore. That’s when she started “raising Cain about it” on Instagram and Facebook.
You probably know someone like Sally Nix — someone with a chronic or life-threatening illness whose doctor says they need a drug, procedure, or scan, and whose insurance company has replied: No.
Prior authorization was conceived decades ago to rein in health care costs by eliminating duplicative and ineffective treatment. Not only does overtreatment waste billions of dollars every year, but doctors acknowledge it also potentially harms patients.
However, critics worry that prior authorization has now become a way for health insurance companies to save money, sometimes at the expense of patients’ lives. KFF Health News has heard from hundreds of people in the past year relating their prior authorization horror stories.
When we first met Nix, she was battling her insurance company to regain authorization for her infusions. She’d been forced to pause her treatments, unable to afford $13,000 out-of-pocket for each infusion.
Finally, it seemed like months of her hard work had paid off. In July, Nix was told by staff at both her doctor’s office and her hospital that Blue Cross Blue Shield of Illinois would allow her to restart treatment. Her balance was marked “paid” and disappeared from the insurer’s online portal.
But the day after the KFF Health News story was published, Nix said, she learned the message had changed. After restarting treatment, she received a letter from the insurer saying her diagnoses didn’t actually qualify her for the infusions. It felt like health insurance whiplash.
“They’re robbing me of my life,” she said. “They’re robbing me of so much, all because of profit.”
Dave Van de Walle, a spokesperson for Blue Cross Blue Shield of Illinois, said the company would not discuss individual patients’ cases.
“Prior authorization is often a requirement for certain treatments,” Van de Walle said in a written statement, “and BCBSIL administers benefits according to medical policy and the employer’s benefit.”
But Nix is a Southern woman of the “Steel Magnolia” variety. In other words, she’s not going down without a fight.
In September, she called out her insurance company’s tactics in a http://change.org/ campaign that has garnered more than 21,000 signatures. She has also filed complaints against her insurance company with the U.S. Department of Health and Human Services, U.S. Department of Labor, Illinois Department of Insurance, and Illinois attorney general.
Even so, Nix said, she feels defeated.
Not only is she still waiting for prior authorization to restart her immunoglobulin infusions, but her insurance company recently required Nix to secure preapproval for another treatment — routine numbing injections she has received for nearly 10 years to treat the nerve pain caused by trigeminal neuralgia.
“It is reprehensible what they’re doing. But they’re not only doing it to me,” said Nix, who is now reluctantly taking prescription opioids to ease her pain. “They’re doing it to other patients. And it’s got to stop.”
Do you have an experience with prior authorization you’d like to share? Click here to tell your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Share This Post
Related Posts
-
Dentists Are Pulling ‘Healthy’ and Treatable Teeth To Profit From Implants, Experts Warn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Becky Carroll was missing a few teeth, and others were stained or crooked. Ashamed, she smiled with lips pressed closed. Her dentist offered to fix most of her teeth with root canals and crowns, Carroll said, but she was wary of traveling a long road of dental work.
Then Carroll saw a TV commercial for another path: ClearChoice Dental Implant Centers. The company advertises that it can give patients “a new smile in as little as one day” by surgically replacing teeth instead of fixing them.
So Carroll saved and borrowed for the surgery, she said. In an interview and a lawsuit, Carroll said that at a ClearChoice clinic in New Jersey in 2021, she agreed to pay $31,000 to replace all her natural upper teeth with pearly-white prosthetic ones. What came next, Carroll said, was “like a horror movie.”
Carroll alleged that her anesthesia wore off during implant surgery, so she became conscious as her teeth were removed and titanium screws were twisted into her jawbone. Afterward, Carroll’s prosthetic teeth were so misaligned that she was largely unable to chew for more than two years until she could afford corrective surgery at another clinic, according to a sworn deposition from her lawsuit.
ClearChoice has denied Carroll’s claims of malpractice and negligence in court filings and did not respond to requests for comment on the ongoing case.
“I thought implants would be easier, and all at once, so you didn’t have to keep going back to the dentist,” Carroll, 52, said in an interview. “But I should have asked more questions … like, Can they save these teeth?”
Dental implants have been used for more than half a century to surgically replace missing or damaged teeth with artificial duplicates, often with picture-perfect results. While implant dentistry was once the domain of a small group of highly trained dentists and specialists, tens of thousands of dental providers now offer the surgery and place millions of implants each year in the U.S.
Amid this booming industry, some implant experts worry that many dentists are losing sight of dentistry’s fundamental goal of preserving natural teeth and have become too willing to remove teeth to make room for expensive implants, according to a months-long investigation by KFF Health News and CBS News. In interviews, 10 experts said they had each given second opinions to multiple patients who had been recommended for mouths full of implants that the experts ultimately determined were not necessary. Separately, lawsuits filed across the country have alleged that implant patients like Carroll have experienced painful complications that have required corrective surgery, while other lawsuits alleged dentists at some implant clinics have persuaded, pressured, or forced patients to remove teeth unnecessarily.
The experts warn that implants, for a single tooth or an entire mouth, expose patients to costs and surgery complications, plus a new risk of future dental problems with fewer treatment options because their natural teeth are forever gone.
“There are many cases where teeth, they’re perfectly fine, and they’re being removed unnecessarily,” said William Giannobile, dean of the Harvard School of Dental Medicine. “I really hate to say it, but many of them are doing it because these procedures, from a monetary standpoint, they’re much more beneficial to the practitioner.”
Giannobile and nine other experts say they are combating a false public perception that implants are more durable and longer-lasting than natural teeth, which some believe stems in part from advertising on TV and social media. Implants require upkeep, and although they can’t get cavities, studies have shown that patients can be susceptible to infections in the gums and bone around their implants.
“Just because somebody can afford implants doesn’t necessarily mean that they’re a good candidate,” said George Mandelaris, a Chicago-area periodontist and member of the American Academy of Periodontology Board of Trustees. “When an implant has infection, or when an implant has bone loss, an implant dies a much quicker death than do teeth.”
In its simplest form, implant surgery involves extracting a single tooth and replacing it with a metal post that is screwed into the jaw and then affixed with a prosthetic tooth commonly made of porcelain, also known as a crown. Patients can also use “full-arch” or “All-on-4” implants to replace all their upper or lower teeth — or all their teeth.
For this story, KFF Health News and CBS News sought interviews with large dental chains whose clinics offer implant surgery — ClearChoice, Aspen Dental, Affordable Care, and Dental Care Alliance — each of which declined to be interviewed or did not respond to multiple requests for comment. The Association of Dental Support Organizations, which represents these companies and others like them, also declined an interview request.
ClearChoice, which specializes in full-arch implants, did not answer more than two dozen questions submitted in writing. In an emailed statement, the company said full-arch implants “have become a well-accepted standard of care for patients with severe tooth loss and teeth with poor prognosis.”
“The use of full-arch restorations reflects the evolution of modern dentistry, offering patients a solution that restores their ability to eat, speak, and live comfortably — far beyond what traditional dentures can provide,” the company said.
Carroll said she regrets not letting her dentist try to fix her teeth and rushing to ClearChoice for implants.
“Because it was a nightmare,” she said.
‘They Are Not Teeth’
Dental implant surgery can be a godsend for patients with unsalvageable teeth. Several experts said implants can be so transformative that their invention should have contended for a Nobel Prize. And yet, these experts still worry that implants are overused, because it is generally better for patients to have their natural teeth.
Paul Rosen, a Pennsylvania periodontist who said he has worked with implants for more than three decades, said many patients believe a “fallacy” that implants are “bulletproof.”
“You can’t just have an implant placed and go off riding into the sunset,” Rosen said. “In many instances, they need more care than teeth because they are not teeth.”
Generally, a single implant costs a few thousand dollars while full-arch implants cost tens of thousands. Neither procedure is well covered by dental insurance, so many clinics partner with credit companies that offer loans for implant surgeries. At ClearChoice, for example, loans can be as large as $65,000 paid off over 10 years, according to the company’s website.
Despite the price, implants are more popular than ever. Sales increased by more than 6% on average each year since 2010, culminating in more than 3.7 million implants sold in the U.S. in 2022, according to a 2023 report produced by iData Research, a health care market research firm.
Some worry implant dentistry has gone too far. In 10 interviews, dentists and dental specialists with expertise in implants said they had witnessed the overuse of implants firsthand. Each expert said they’d examined multiple patients in recent years who were recommended for full-arch implants by other dentists despite their teeth being treatable with conventional dentistry.
Giannobile, the Harvard dean, said he had given second opinions to “dozens” of patients who were recommended for implants they did not need.
“I see many of these patients now that are coming in and saying, ‘I’ve been seen, and they are telling me to get my entire dentition — all of my teeth — extracted.’ And then I’ll take a look at them and say that we can preserve most of your teeth,” Giannobile said.
Tim Kosinski, who is a representative of the Academy of General Dentistry and said he has placed more than 19,000 implants, said he examines as many as five patients a month who have been recommended for full-arch implants that he deems unnecessary.
“There is a push in the profession to remove teeth that could be saved,” Kosinski said. “But the public isn’t aware.”
Luiz Gonzaga, a periodontist and prosthodontist at the University of Florida, said he, too, had turned away patients who wanted most or all their teeth extracted. Gonzaga said some had received implant recommendations that he considered “an atrocity.”
“You don’t go to the hospital and tell them ‘I broke my finger a couple of times. This is bothering me. Can you please cut my finger off?’ No one will do that,” Gonzaga said. “Why would I extract your tooth because you need a root canal?”
Jaime Lozada, director of an elite dental implant residency program at Loma Linda University, said he’d not only witnessed an increase in dentists extracting “perfectly healthy teeth” but also treated a rash of patients with mouths full of ill-fitting implants that had to be surgically replaced.
Lozada said in August that he’d treated seven such patients in just three months.
“When individuals just make a decision of extracting teeth to make it simple and make money quick, so to speak, that’s where I have a problem,” Lozada said. “And it happens quite often.”
When full-arch implants fail, patients sometimes don’t have enough jawbone left to anchor another set. These patients have little choice but to get implants that reach into cheekbones, said Sohail Saghezchi, an oral and maxillofacial surgeon at the University of California-San Francisco.
“It’s kind of like a last resort,” Saghezchi said. “If those fail, you don’t have anywhere else to go.”
‘It Was Horrendous Dentistry’
Most of the experts interviewed for this article said their rising alarm corresponded with big changes in the availability of dental implants. Implants are now offered by more than 70,000 dental providers nationwide, two-thirds of whom are general dentists, according to the iData Research report.
Dentists are not required to learn how to place implants in dental school, nor are they required to complete implant training before performing the surgery in nearly all states. This year, Oregon started requiring dentists to complete 56 hours of hands-on training before placing any implants. Stephen Prisby, executive director of the Oregon Board of Dentistry, said the requirement — the first and only of its kind in the U.S. — was a response to dozens of investigations in the state into botched surgeries and other implant failures, split evenly between general dentists and specialists.
“I was frankly stunned at how bad some of these dentists were practicing,” Prisby said. “It was horrendous dentistry.”
Many dental clinics that offer implants have consolidated into chains owned by private equity firms that have bought out much of implant dentistry. In health care, private equity investment is sometimes criticized for overtreatment and prioritizing short-term profit over patients.
Private equity firms have spent about $5 billion in recent years to buy large dental chains that offer implants at hundreds of clinics owned by individual dentists and dental specialists. ClearChoice was bought for an estimated $1.1 billion in 2020 by Aspen Dental, which is owned by three private equity firms, according to PitchBook, a research firm focused on the private equity industry. Private equity firms also bought Affordable Care, whose largest clinic brand is Affordable Dentures & Implants, for an estimated $2.7 billion in 2021, according to PitchBook. And the private equity wing of the Abu Dhabi government bought Dental Care Alliance, which offers implants at many of its affiliated clinics, for an estimated $1 billion in 2022, according to PitchBook.
ClearChoice and Aspen Dental each said in email statements that the companies’ private equity owners “do not have influence or control over treatment recommendations.” Both companies said dentists or dental specialists make all clinical decisions.
Private equity deals involving dental practices increased ninefold from 2011 to 2021, according to an American Dental Association study published in August. The study also said investors showed an interest in oral surgery, possibly because of the “high prices” of implants.
“Some argue this is a negative thing,” said Marko Vujicic, vice president of the association’s Health Policy Institute, who co-authored the study. “On the other hand, some would argue that involvement of private equity and outside capital brings economies of scale, it brings efficiency.”
Edwin Zinman, a San Francisco dental malpractice attorney and former periodontist who has filed hundreds of dental lawsuits over four decades, said he believed many of the worst fears about private equity owners had already come true in implant dentistry.
“They’ve sold a lot of [implants], and some of it unnecessarily, and too often done negligently, without having the dentists who are doing it have the necessary training and experience,” Zinman said. “It’s for five simple letters: M-O-N-E-Y.”
Hundreds of Implant Clinics With No Specialists
For this article, journalists from KFF Health News and CBS News analyzed the webpages for more than 1,000 clinics in the nation’s largest private equity-owned dental chains, all of which offer some implants. The analysis found that more than 70% of those clinics listed only general dentists on their websites and did not appear to employ the specialists — oral surgeons, periodontists, or prosthodontists — who traditionally have more training with implants.
Affordable Dentures & Implants listed specialists at fewer than 5% of its more than 400 clinics, according to the analysis. The rest were staffed by general dentists, most of whom did not list credentialing from implant training organizations, according to the analysis.
ClearChoice, on the other hand, employs at least one oral surgeon or prosthodontist at each of its more than 100 centers, according to the analysis. But its new parent company, Aspen Dental, which offers implants in many of its more than 1,100 clinics, does not list any specialists at many of those locations.
Not everyone is worried about private equity in implant dentistry. In interviews arranged by the American Academy of Implant Dentistry, which trains dentists to use implants, two other implant experts did not express concerns about private equity firms.
Brian Jackson, a former academy president and implant specialist in New York, said he believed dentists are too ethical and patients are too smart to be pressured by private equity owners “who will never see a patient.”
Jumoke Adedoyin, a chief clinical officer for Affordable Care, who has placed implants at an Affordable Dentures & Implants clinic in the Atlanta suburbs for 15 years, said she had never felt pressure from above to sell implants.
“I’ve actually felt more pressure sometimes from patients who have gone around and been told they need to take their teeth out,” she said. “They come in and, honestly, taking a look at them, maybe they don’t need to take all their teeth out.”
Still, lawsuits filed across the country have alleged that dentists at implant clinics have extracted patients’ teeth unnecessarily.
For example, in Texas, a patient alleged in a 2020 lawsuit that an Affordable Care dentist removed “every single tooth from her mouth when such was not necessary,” then stuffed her mouth with gauze and left her waiting in the lobby as he and his staff left for lunch. In Maryland, a patient alleged in a 2021 lawsuit that ClearChoice “convinced” her to extract “eight healthy upper teeth,” by “greatly downplay[ing] the risks.” In Florida, a patient alleged in a 2023 lawsuit that ClearChoice provided her with no other treatment options before extracting all her teeth, “which was totally unnecessary.”
ClearChoice and Affordable Care denied wrongdoing in their respective lawsuits, then privately settled out of court with each patient. ClearChoice and Affordable Care did not respond to requests for comment submitted to the companies or attorneys. Lawyers for all three plaintiffs declined to comment on these lawsuits or did not respond to requests for comment.
Fred Goldberg, a Maryland dental malpractice attorney who said he has represented at least six clients who sued ClearChoice, said each of his clients agreed to get implants after meeting with a salesperson — not a dentist.
“Every client I’ve had who has gone to ClearChoice has started off meeting a salesperson and actually signing up to get their financing through ClearChoice before they ever meet with a dentist,” Goldberg said. “You meet with a salesperson who sells you on what they like to present as the best choice, which is almost always that they’re going to take out all your natural teeth.”
Becky Carroll, the ClearChoice patient from New Jersey, told a similar story.
Carroll said in her lawsuit that she met first with a ClearChoice salesperson referred to as a “patient education consultant.” In an interview, Carroll said the salesperson encouraged her to borrow money from family members for the surgery and it was not until after she agreed to a loan and passed a credit check that a ClearChoice dentist peered into her mouth.
“It seems way backwards,” Carroll said. “They just want to know you’re approved before you get to talk to a dentist.”
CBS News producer Nicole Keller contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Circadian Diabetes Code – by Dr. Satchin Panda
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previously reviewed Dr. Panda’s “The Circadian Code” which pertains to the circadian rhythms (yes, plural) in general; this one uses much of the same research, but with a strong focus on the implications for blood sugar management.
It’s first a primer in diabetes (and prediabetes, and, in contrast, what things should look like if healthy). You’ll understand about glucose metabolism and glycogen and insulin and more; you’ll understand what blood sugar readings mean, and you’ll know what an Hb1AC count actually is and what it should look like too, things like that.
After that, it’s indeed about what the subtitle promises: the right times to eat (and what to eat), when to exercise (and how, at which time), and how to optimize your sleep in the context of circadian rhythm and blood sugar management.
You may be wondering: why does circadian rhythm matter for blood sugars? And the answer is explained at some length in the first part of the book, but to oversimplify greatly: your body needs energy all the time, no matter when it was that you last ate. Thus, it has to organize its energy reserves to that at all times you can 1) function, on a cellular level 2) maintain a steady balance of sugar in your blood despite using it at slightly higher or lower levels at different times of day. Because the basal metabolic rate accounts for most of our energy use, the body has to plan for a base rate of so much energy per day, and to do that, it needs to know what a day is. Dr. Panda explains this in detail (the marvels of PER proteins and all that), but basically, that’s the relevance of circadian rhythm.
However, it’s not all theory and biochemistry; there is also a 12-week program to reverse prediabetes and type 2 diabetes (it will not, of course, reverse Type 1 Diabetes, sorry—but the program will still be beneficial even in that case, since more even blood sugars means fewer woes).
They style is friendly and clear, explaining the science simply, yet without patronizing the reader. References are given, with claims sourced in an extensive bibliography.
Bottom line: if you or a loved one have diabetes or prediabetes, or just have a strong desire to avoid getting such and generally keep your metabolic health in good order, this book will definitely help.
Click here to check out The Diabetes Code, and enjoy better blood sugar health than ever!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Edam vs Gouda – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edam to gouda, we picked the edam.
Why?
There’s not a lot between them, but there are some differences:
In terms of macros, their numbers are all close enough that one may beat the other by decimal place rounding, so we’ll call this a tie. Same goes for their fat type breakdowns; per 100g they both have 18g saturated, 8g monounsaturated, and 1g polyunsaturated.
In the category of vitamins, edam has slightly more of vitamins A, B1, B2, and B3, while gouda has slightly more of vitamins B5 and B9. A modest 4:2 win for edam.
When it comes to minerals, edam has more calcium, iron, and potassium, while gouda is not higher in any minerals. A more convincing win for edam.
In short, enjoy either or both in moderation, but if you’re going to choose one over the other, edam is the way to go.
Want to learn more?
You might like to read:
Can Saturated Fats Be Healthy?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: