Can I take antihistamines everyday? More than the recommended dose? What if I’m pregnant? Here’s what the research says
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Allergies happen when your immune system overreacts to a normally harmless substance like dust or pollen. Hay fever, hives and anaphylaxis are all types of allergic reactions.
Many of those affected reach quickly for antihistamines to treat mild to moderate allergies (though adrenaline, not antihistamines, should always be used to treat anaphylaxis).
If you’re using oral antihistamines very often, you might have wondered if it’s OK to keep relying on antihistamines to control symptoms of allergies. The good news is there’s no research evidence to suggest regular, long-term use of modern antihistamines is a problem.
But while they’re good at targeting the early symptoms of a mild to moderate allergic reaction (sneezing, for example), oral antihistamines aren’t as effective as steroid nose sprays for managing hay fever. This is because nasal steroid sprays target the underlying inflammation of hay fever, not just the symptoms.
Here are the top six antihistamines myths – busted.

Myth 1. Oral antihistamines are the best way to control hay fever symptoms
Wrong. In fact, the recommended first line medical treatment for most patients with moderate to severe hay fever is intranasal steroids. This might include steroid nose sprays (ask your doctor or pharmacist if you’d like to know more).
Studies have shown intranasal steroids relieve hay fever symptoms better than antihistamine tablets or syrups.
To be effective, nasal steroids need to be used regularly, and importantly, with the correct technique.
In Australia, you can buy intranasal steroids without a doctor’s script at your pharmacy. They work well to relieve a blocked nose and itchy, watery eyes, as well as improve chronic nasal blockage (however, antihistamine tablets or syrups do not improve chronic nasal blockage).
Some newer nose sprays contain both steroids and antihistamines. These can provide more rapid and comprehensive relief from hay fever symptoms than just oral antihistamines or intranasal steroids alone. But patients need to keep using them regularly for between two and four weeks to yield the maximum effect.
For people with seasonal allergic rhinitis (hayfever), it may be best to start using intranasal steroids a few weeks before the pollen season in your regions hits. Taking an antihistamine tablet as well can help.
Antihistamine eye drops work better than oral antihistamines to relieve acutely itchy eyes (allergic conjunctivitis).
Myth 2. My body will ‘get used to’ antihistamines
Some believe this myth so strongly they may switch antihistamines. But there’s no scientific reason to swap antihistamines if the one you’re using is working for you. Studies show antihistamines continue to work even after six months of sustained use.
Myth 3. Long-term antihistamine use is dangerous
There are two main types of antihistamines – first-generation and second-generation.
First-generation antihistamines, such as chlorphenamine or promethazine, are short-acting. Side effects include drowsiness, dry mouth and blurred vision. You shouldn’t drive or operate machinery if you are taking them, or mix them with alcohol or other medications.
Most doctors no longer recommend first-generation antihistamines. The risks outweigh the benefits.
The newer second-generation antihistamines, such as cetirizine, fexofenadine, or loratadine, have been extensively studied in clinical trials. They are generally non-sedating and have very few side effects. Interactions with other medications appear to be uncommon and they don’t interact badly with alcohol. They are longer acting, so can be taken once a day.
Although rare, some side effects (such as photosensitivity or stomach upset) can happen. At higher doses, cetirizine can make some people feel drowsy. However, research conducted over a period of six months showed taking second-generation antihistamines is safe and effective. Talk to your doctor or pharmacist if you’re concerned.

Myth 4. Antihistamines aren’t safe for children or pregnant people
As long as it’s the second-generation antihistamine, it’s fine. You can buy child versions of second-generation antihistamines as syrups for kids under 12.
Though still used, some studies have shown certain first-generation antihistamines can impair childrens’ ability to learn and retain information.
Studies on second-generation antihistamines for children have found them to be safer and better than the first-generation drugs. They may even improve academic performance (perhaps by allowing kids who would otherwise be distracted by their allergy symptoms to focus). There’s no good evidence they stop working in children, even after long-term use.
For all these reasons, doctors say it’s better for children to use second-generation than first-generation antihistimines.
What about using antihistimines while you’re pregnant? One meta analysis of combined study data including over 200,000 women found no increase in fetal abnormalities.
Many doctors recommend the second-generation antihistamines loratadine or cetirizine for pregnant people. They have not been associated with any adverse pregnancy outcomes. Both can be used during breastfeeding, too.
Myth 5. It is unsafe to use higher than the recommended dose of antihistamines
Higher than standard doses of antihistamines can be safely used over extended periods of time for adults, if required.
But speak to your doctor first. These higher doses are generally recommended for a skin condition called chronic urticaria (a kind of chronic hives).
Myth 6. You can use antihistamines instead of adrenaline for anaphylaxis
No. Adrenaline (delivered via an epipen, for example) is always the first choice. Antihistamines don’t work fast enough, nor address all the problems caused by anaphylaxis.
Antihistamines may be used later on to calm any hives and itching, once the very serious and acute phase of anaphylaxis has been resolved.
In general, oral antihistamines are not the best treatment to control hay fever – you’re better off with steroid nose sprays. That said, second-generation oral antihistamines can be used to treat mild to moderate allergy symptoms safely on a regular basis over the long term.
Janet Davies, Respiratory Allergy Stream Co-chair, National Allergy Centre of Excellence; Professor and Head, Allergy Research Group, Queensland University of Technology; Connie Katelaris, Professor of Immunology and Allergy, Western Sydney University, and Joy Lee, Respiratory Allergy Stream member, National Allergy Centre of Excellence; Associate Professor, School of Public Health and Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pasteurization: What It Does And Doesn’t Do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pasteurization’s Effect On Risks & Nutrients
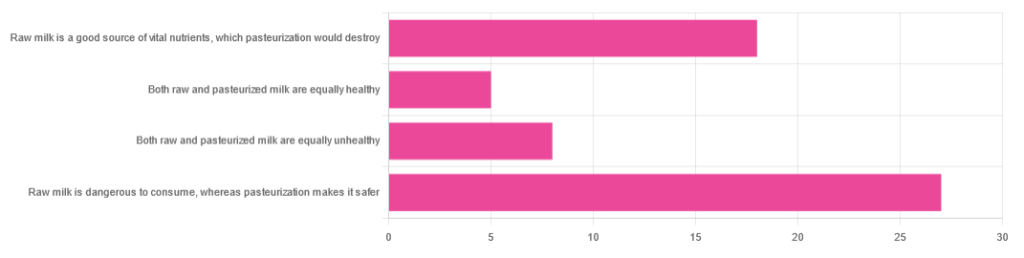
In Wednesday’s newsletter, we asked you for your health-related opinions of raw (cow’s) milk, and got the above-depicted, below-described, set of responses:
- About 47% said “raw milk is dangerous to consume, whereas pasteurization makes it safer”
- About 31% said “raw milk is a good source of vital nutrients which pasteurization would destroy”
- About 14% said “both raw milk and pasteurized milk are equally unhealthy”
- About 9% said “both raw milk and pasteurized milk are equally healthy”
Quite polarizing! So, what does the science say?
“Raw milk is dangerous to consume, whereas pasteurization makes it safer: True or False?”
True! Coincidentally, the 47% who voted for this are mirrored by the 47% of the general US population in a similar poll, deciding between the options of whether raw milk is less safe to drink (47%), just as safe to drink (15%), safer to drink (9%), or not sure (30%):
Public Fails to Appreciate Risk of Consuming Raw Milk, Survey Finds
As for what those risks are, by the way, unpasteurized dairy products are estimated to cause 840x more illness and 45x more hospitalizations than pasteurized products.
This is because unpasteurized milk can (and often does) contain E. coli, Listeria, Salmonella, Cryptosporidium, and other such unpleasantries, which pasteurization kills.
Source for both of the above claims:
(we know the title sounds vague, but all this information is easily visible in the abstract, specifically, the first two paragraphs)
Raw milk is a good source of vital nutrients which pasteurization would destroy: True or False?
False! Whether it’s a “good” source can be debated depending on other factors (e.g., if we considered milk’s inflammatory qualities against its positive nutritional content), but it’s undeniably a rich source. However, pasteurization doesn’t destroy or damage those nutrients.
Incidentally, in the same survey we linked up top, 16% of the general US public believed that pasteurization destroys nutrients, while 41% were not sure (and 43% knew that it doesn’t).
Note: for our confidence here, we are skipping over studies published by, for example, dairy farming lobbies and so forth. Those do agree, by the way, but nevertheless we like sources to be as unbiased as possible. The FDA, which is not completely unbiased, has produced a good list of references for this, about half of which we would consider biased, and half unbiased; the clue is generally in the journal names. For example, Food Chemistry and the Journal of Food Science and Journal of Nutrition are probably less biased than the International Dairy Association and the Journal of Dairy Science:
FDA | Raw Milk Misconceptions and the Danger of Raw Milk Consumption
this page covers a lot of other myths too, more than we have room to “bust” here, but it’s very interesting reading and we recommend to check it out!
Notably, we also weren’t able to find any refutation by counterexample on PubMed, with the very slight exception that some studies sometimes found that in the case of milks that were of low quality, pasteurization can reduce the vitamin E content while increasing the vitamin A content. For most milks however, no significant change was found, and in all cases we looked at, B-vitamins were comparable and vitamin D, popularly touted as a benefit of cow’s milk, is actually added later in any case. And, importantly, because this is a common argument, no change in lipid profiles appears to be findable either.
In science, when something has been well-studied and there aren’t clear refutations by counterexample, and the weight of evidence is clearly very much tipped into one camp, that usually means that camp has it right.
Milk generally is good/bad for the health: True or False?
True or False, depending on what we want to look at. It’s definitely not good for inflammation, but the whole it seems to be cancer-neutral and only increases heart disease risk very slightly:
- Keep Inflammation At Bay ← short version is milk is bad, fermented milk products are fine in moderation
- Is Dairy Scary? ← short version is that milk is neither good nor terrible; fermented dairy products however are health-positive in numerous ways when consumed in moderation
You may be wondering…
…how this goes for the safety of dairy products when it comes to the bird flu currently affecting dairy cows, so:
Take care!
Share This Post
-
Quit Like a Woman – by Holly Whitaker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed “quit drinking” books before, so what makes this one different?
While others focus on the science of addiction and the tips and tricks of habit breaking/forming, this one is more about environmental factors, and that because of society being as it is, we as women often face different challenges when it comes to drinking (or not). Not necessarily easier or harder than men’s in this case, but different. And that sometimes calls for different methods to deal with them. This book explores those.
She also looks at such matters as how to quit alcohol when you’ve never stuck to a diet, and other such very down-to-earth topics, in a well-researched and non-preachy fashion.
Bottom line: if you’ve sometimes tried to quit drinking or even just to cut back, but found the deck stacked against you and things conspire to undermine your efforts, this book will give you a clearer path forward.
Click here to check out Quite Like A Woman, And Take Care Of Yourself!
Share This Post
-
Loving Someone Who Has Dementia – by Dr. Pauline Boss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed Dr. Boss’s excellent book “Loss, Trauma, and Resilience: Therapeutic Work With Ambiguous Loss”, which partially overlaps in ideas with this one. In that case, it was about grief when a loved one is “gone, but are they really?”, which can include missing persons, people killed in ways that weren’t 100% confirmed (e.g. no body to bury), and in contrast, people who are present in body but not entirely present mentally: perhaps in a coma, for example. It also includes people are for other reasons not entirely present in the way they used to be, which includes dementia. And that latter case is what this book focuses on.
In the case of dementia, we cannot, of course, simply focus on ourselves. Well, not if we care about the person with dementia, anyway. Much like with the other kinds of ambiguous loss, we cannot fully come to terms with things while on the cusp of presence and absence, and we cannot, as such, “give up” on our loved one.
What then, of hope? The author makes the case for—in absence of any kind of closure—making our peace with the situation as it is, making our peace with the uncertainty of things. And that means not only “at any moment could come a more clearly complete loss”, but also on the flipside at least a faint candle of hope, that we should not grasp with both hands (that is not how to treat a candle, literally or metaphorically), but rather, hold gently, and enjoy its gentle light.
Dr. Boss also covers more practical considerations; family rituals, celebrations, gatherings, and the idea of “the good-enough relationship”. Particularly helpfully, she gives her “seven guidelines for the journey”, which even if one decides against adopting them all, are definitely all good things to at least have considered.
The style is much more tailored to the lay reader than the other book of hers that we reviewed, which was intended more for clinicians, but useful also for those of us who have been hit by such kinds of grief. In this case, however, her intention is first and foremost for the family of a person who has dementia—there are still footnotes throughout though, for those who still want to read scientific papers that support the various ideas discussed in the book.
Bottom line: if a loved one has dementia or that seems a likely possibility for you, this book can help a lot!
Share This Post
Related Posts
-
Sciatica Exercises & Home Treatment – by Dr. George Best
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Best is a doctor of chiropractic, but his work here is compelling. He starts by giving an overview of the relevant anatomy, and then the assorted possible causes of sciatica, before moving on to the treatments.
As is generally the case for chiropractic, nothing here will be “cured”, but it will give methods for ongoing management to keep you pain-free—which in the case of sciatica, is usually the single biggest thing that most people suffering from it most dearly want.
We get to read a lot about self-massage and exercises, of the (very well-evidenced; about the most well-evidenced thing there is for back pain) McKenzie technique exercises, as well as assorted acupressure-based techniques that are less well-evidenced but have good anecdotal support.
He also writes about preventing sciatica—which if you already have it, that doesn’t mean it’s too late; it just means, in that case do these things (along with the aforementioned exercises) to gradually reverse the harm done and get back to where you were pre-sciatica.
Lastly, he does also speak on when signs might point to your problems being beyond the scope of this book, and seeking professional examination if you haven’t already.
The style throughout is straight to the point, informative, and instructional. There is zero fluff or padding, and no sensationalization. There are diagrams and illustrative photos where appropriate.
Bottom line: if you have, or fear the threat of, sciatica, then this is an excellent book to have and use its exercises.
Click here to check out Sciatica Exercises & Home Treatment, and live pain-free!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Easy Ways To Fix Brittle, Dry, Wiry Hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sam Ellis, a dermatologist, specializes in skin, hair, and nail care—and she’s here with professional knowledge:
Tackling the problem at the root
As we age, hair becomes less shiny, more brittle, coarse, wiry, or gray. More concerningly for many, hair thinning and shedding increases due to shortened growth phases and hormonal changes.
The first set of symptoms there are largely because sebum production decreases, leading to dry hair. It’s worth bearing in mind though, that factors like UV radiation, smoking, stress, and genetics contribute to hair aging too. So while we can’t do much about genetics, the modifiable factors are worth addressing.
Menopause and the corresponding “andropause” impact hair health, and hormonal shifts, not just aging, drive many hair changes. Which is good to know, because it means that HRT (mostly: topping up estrogen or testosterone as appropriate) can make a big difference. Additionally, topical/oral minoxidil and DHT blockers (such as finasteride or dutasteride) can boost hair density. These things come with caveats though, so do research any possible treatment plan before embarking on it, to be sure you are comfortable with all aspects of it—including that if you use minoxidil, while on the one hand it indeed works wonders, on the other hand, you’ll then have to keep using minoxidil for the rest of your life or your hair will fall out when you stop. So, that’s a commitment to be thought through before beginning.
Nutritional deficiencies (iron, zinc, vitamin D) and insufficient protein intake hinder hair growth, so ensure proper nutrition, with sufficient protein and micronutrients.
While we’re on the topic of “from the inside” things: take care to manage stress healthily, as stress negatively affects hair health.
Now, as for “from the outside”…
Dr. Ellis recommends moisturizing shampoos/conditioners; Virtue and Dove brands she mentions positively. She also recommends bond repair products (such as K18 and Olaplex) that restore hair integrity, and heat protectants (she recommends: Unite 7 Seconds) as well as hair oils in general that improve hair condition.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cranberries vs Goji Berries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cranberries to goji berries, we picked the cranberries.
Why?
Both are great! And your priorities may differ. Here’s how they stack up:
In terms of macros, goji berries have more protein, carbs, and fiber. This is consistent with them generally being eaten very dried, whereas cranberries are more often eaten fresh or from frozen, or partially rehydrated. In any case, goji berries are the “more food per food” option, so it wins this category. The glycemic indices are both low, by the way, though goji berries are the lower.
When it comes to vitamins, cranberries have more of vitamins B1, B2, B3, B5, B6, B9, E, K, and choline, while goji berries have more of vitamins A and C. Admittedly it’s a lot more, but still, on strength of overall vitamin coverage, the clear winner here is cranberries.
We see a similar story when it comes to minerals: cranberries have more copper, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while goji berries have (a lot) more calcium and iron. Again, by strength of overall mineral coverage, the clear winner here is cranberries.
Cranberries do also have some extra phytochemical benefits, including their prevention/cure status when it comes to UTIs—see our link below for more on that.
At any rate, enjoy either or both, but those are the strengths and weaknesses of these two berries!
Want to learn more?
You might like to read:
- Health Benefits Of Cranberries (But: You’d Better Watch Out)
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars ← this is also about goji berries
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: