What is ‘breathwork’? And do I need to do it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From “breathwork recipes” to breathing techniques, many social media and health websites are recommending breathwork to reduce stress.
But breathwork is not new. Rather it is the latest in a long history of breathing techniques such as Pranayama from India and qigong from China. Such practices have been used for thousands of years to promote a healthy mind and body.
The benefits can be immediate and obvious. Try taking a deep breath in through your nose and exhaling slowly. Do you feel a little calmer?
So, what’s the difference between the breathing we do to keep us alive and breathwork?

Breathwork is about control
Breathwork is not the same as other mindfulness practices. While the latter focus on observing the breath, breathwork is about controlling inhalation and exhalation.
Normally, breathing happens automatically via messages from the brain, outside our conscious control. But we can control our breath, by directing the movement of our diaphragm and mouth.
The diaphragm is a large muscle that separates our thoracic (chest) and abdominal (belly) cavities. When the diaphragm contracts, it expands the thoracic cavity and pulls air into the lungs.
Controlling how deep, how often, how fast and through what (nose or mouth) we inhale is the crux of breathwork, from fire breathing to the humming bee breath.
Breathwork can calm or excite
Even small bits of breathwork can have physical and mental health benefits and complete the stress cycle to avoid burnout.
Calming breathwork includes diaphragmatic (belly) breathing, slow breathing, pausing between breaths, and specifically slowing down the exhale.
In diaphragmatic breathing, you consciously contract your diaphragm down into your abdomen to inhale. This pushes your belly outwards and makes your breathing deeper and slower.
You can also slow the breath by doing:
- box breathing (count to four for each of four steps: breathe in, hold, breathe out, hold), or
- coherent breathing (controlled slow breathing of five or six breaths per minute), or
- alternate nostril breathing (close the left nostril and breathe in slowly through the right nostril, then close the right nostril and breathe out slowly through the left nostril, then repeat the opposite way).
You can slow down the exhalation specifically by counting, humming or pursing your lips as you breathe out.
In contrast to these calming breathing practices, energising fast-paced breathwork increases arousal. For example, fire breathing (breathe in and out quickly, but not deeply, through your nose in a consistent rhythm) and Lion’s breath (breathe out through your mouth, stick your tongue out and make a strong “haa” sound).
What is happening in the body?
Deep and slow breathing, especially with a long exhale, is the best way to stimulate the vagus nerves. The vagus nerves pass through the diaphragm and are the main nerves of the parasympathetic nervous system.
Simulating the vagus nerves calms our sympathetic nervous system (fight or flight) stress response. This improves mood, lowers the stress hormone cortisol and helps to regulate emotions and responses. It also promotes more coordinated brain activity, improves immune function and reduces inflammation.
Taking deep, diaphragmatic breaths also has physical benefits. This improves blood flow, lung function and exercise performance, increases oxygen in the body, and strengthens the diaphragm.
Slow breathing reduces heart rate and blood pressure and increases heart rate variability (normal variation in time between heart beats). These are linked to better heart health.
Taking shallow, quick, rhythmic breaths in and out through your nose stimulates the sympathetic nervous system. Short-term, controlled activation of the stress response is healthy and develops resilience to stress.
Breathing in through the nose
We are designed to inhale through our nose, not our mouth. Inside our nose are lots of blood vessels, mucous glands and tiny hairs called cilia. These warm and humidify the air we breathe and filter out germs and toxins.
We want the air that reaches our airways and lungs to be clean and moist. Cold and dry air is irritating to our nose and throat, and we don’t want germs to get into the body.
Nasal breathing increases parasympathetic activity and releases nitric oxide, which improves airway dilation and lowers blood pressure.
Consistently breathing through our mouth is not healthy. It can lead to pollutants and infections reaching the lungs, snoring, sleep apnoea, and dental issues including cavities and jaw joint problems.

A free workout
Slow breathing – even short sessions at home – can reduce stress, anxiety and depression in the general population and among those with clinical depression or anxiety. Research on breathwork in helping post-traumatic stress disorder (PTSD) is also promising.
Diaphragmatic breathing to improve lung function and strengthen the diaphragm can improve breathing and exercise intolerance in chronic heart failure, chronic obstructive pulmonary disease and asthma. It can also improve exercise performance and reduce oxidative stress (an imbalance of more free radicals and/or less antioxidants, which can damage cells) after exercise.

A mind-body connection you can access any time
If you feel stressed or anxious, you might subconsciously take shallow, quick breaths, but this can make you feel more anxious. Deep diaphragmatic breaths through your nose and focusing on strong exhalations can help break this cycle and bring calm and mental clarity.
Just a few minutes a day of breathwork can improve your physical and mental health and wellbeing. Daily deep breathing exercises in the workplace reduce blood pressure and stress, which is important since burnout rates are high.
Bottom line: any conscious control of your breath throughout the day is positive.
So, next time you are waiting in a line, at traffic lights or for the kettle to boil, take a moment to focus on your breath. Breathe deeply into your belly through your nose, exhale slowly, and enjoy the benefits.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong and Judy Pickard, Senior Lecturer, Clinical Psychology, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Lessons For A Healthy Mind & Body
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sadia Badiei, food scientist of “Pick Up Limes” culinary fame, has advice in and out of the kitchen:
Pick up a zest for life
Here’s what she picked up, and we all can too:
- “I can’t do it… yet”: it’s never too late to adopt a growth mindset by adding “yet” to your self-doubt, focusing on progress and the possibility of improvement.
- The spotlight effect: people are generally too absorbed in their own lives to focus on you, so don’t worry too much about others’ perceptions.
- Nutrition by addition: focus on adding healthier foods to your diet rather than eliminating the less healthy ones to avoid restrictive mindsets. You can still eliminate the less healthy ones if you want to! It just shouldn’t be the primary focus. Focusing on a conceptually negative thing is rarely helpful.
- It’s ok to change: embrace change as a sign of growth and evolution, rather than seeing it as a failure or waste of time.
- The way you do one thing is the way you do everything: be mindful of how you approach small tasks, regular tasks, boring tasks, unwanted tasks—you can either create a habit of enthusiasm or a habit of suffering (it’s entirely your choice which)
- Setting goals for success: set goals based on actions you can control (inputs) rather than outcomes that are uncertain. Less “lose 10 lbs”, and more “eat fiber before starch”, for example.
- You probably can’t have it all at once: you can achieve all your dreams, but often not simultaneously; goals and desires unfold in stages over time.
- The five-year rule: before adopting a new lifestyle or habit, ask yourself if you can realistically sustain it for five years to ensure it’s not just a short-term fix. If you struggle with this prognostic, look backwards first instead. Which healthy habits have you maintained for decades, and which were you never able to make stick?
- Are you afraid or excited?: reframe fear as excitement, as both emotions share similar physical sensations and signify that you care about the outcome.
- The voice you hear most: speak kindly to yourself in self-talk to create a softer, more compassionate tone. Your subconscious is always listening, so reinforce healthy rather than unhealthy thought patterns.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
80-Year-Olds Share Their Biggest Regrets
Take care!
Share This Post
-
The Pain Relief Secret – by Sarah Warren
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one’s a book to not judge by the cover—or the title. The title is actually accurate, but it sounds like a lot of woo, doesn’t it?
Instead, what we find is a very clinical, research-led (40 pages of references!) explanation of:
- the causes of musculoskeletal pain
- how this will tend to drive us to make it worse
- what we can do instead to make it better
A lot of this, to give you an idea what to expect, hinges on the fact that bones only go where muscles allow/move them; muscles only behave as instructed by nerves, and with a good development of biofeedback and new habits to leverage neuroplasticity, we can take more charge of that than you might think.
Warning: you may want to jump straight into the part with the solutions, but if you do so without a very good grounding in anatomy and physiology, you may find yourself out of your depth with previously-explained terms and concepts that are now needed to understand (and apply) the solutions.
However, if you read it methodically cover-to-cover, you’ll find you need no prior knowledge to take full advantage of this book; the author is a very skilled educator.
Bottom line: while it’s not an overnight magic pill, the methodology described in this book is a very sound way to address the causes of musculoskeletal pain.
Click here to check out The Pain Relief Secret, and help your body undo damage done!
Share This Post
-
Boost Your Digestive Enzymes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ll Try To Make This Easy To Digest
Do you have a digestion-related problem?
If so, you’re far from alone; around 40% of Americans have digestive problems serious enough to disrupt everyday life:
New survey finds forty percent of Americans’ daily lives are disrupted by digestive troubles
…which puts Americans just a little over the global average of 35%:
Mostly likely on account of the Standard American Diet, or “SAD” as it often gets abbreviated in scientific literature.
There’s plenty we can do to improve gut health, for example:
- Making Friends With Your Gut (You Can Thank Us Later)
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- How Much Difference Do Probiotic Supplements Make?
Today we’re going to be examining digestive enzyme supplements!
What are digestive enzymes?
Digestive enzymes are enzymes that break down food into stuff we can use. Important amongst them are:
- Protease: breaks down proteins (into amino acids)
- Amylase: breaks down starches (into sugars)
- Lipase: breaks down fats (into fatty acids)
All three are available as popular supplements to aid digestion. How does the science stack up for them?
Protease
For this, we only found animal studies like this one, but the results have been promising:
Amylase
Again, the studies for this alone (not combined with other enzymes) have been solely from animal agriculture; here’s an example:
The Effect of Exogenous Amylase Supplementation on the Nutritional Value of Peas
Lipase
Unlike for protease and amylase, now we have human studies as well, and here’s what they had to say:
❝Lipase supplementation significantly reduced stomach fullness without change of EGG.
Furthermore, lipase supplementation may be helpful in control of FD symptom such as postprandial symptoms❞
~ Dr. Seon-Young Park & Dr. Jong-Sun Rew
Read more: Is Lipase Supplementation before a High Fat Meal Helpful to Patients with Functional Dyspepsia?
(short answer: yes, it is)
More studies found the same, such as:
Lipase Supplementation before a High-Fat Meal Reduces Perceptions of Fullness in Healthy Subjects
All together now!
When we look at studies for combination supplementation of digestive enzymes, more has been done, and/but it’s (as you might expect) less specific.
The following paper gives a good rundown:
Pancrelipase Therapy: A Combination Of Protease, Amylase, & Lipase
Is it safe?
For most people it is quite safe, but if taking high doses for a long time it can cause problems, and also there may be complications if you have diabetes, are otherwise immunocompromised, or have some other conditions (listed towards the end of the above-linked paper, along with further information that we can’t fit in here).
As ever, check with your doctor/pharmacist if you’re not completely sure!
Want some?
We don’t sell them, but for your convenience, here’s an example product on Amazon that contains all three
Enjoy!
We’ll Try To Make This Easy To Digest
Do you have a digestion-related problem?
If so, you’re far from alone; around 40% of Americans have digestive problems serious enough to disrupt everyday life:
New survey finds forty percent of Americans’ daily lives are disrupted by digestive troubles
…which puts Americans just a little over the global average of 35%:
Mostly likely on account of the Standard American Diet, or “SAD” as it often gets abbreviated in scientific literature.
There’s plenty we can do to improve gut health, for example:
- Making Friends With Your Gut (You Can Thank Us Later)
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- How Much Difference Do Probiotic Supplements Make?
Today we’re going to be examining digestive enzyme supplements!
What are digestive enzymes?
Digestive enzymes are enzymes that break down food into stuff we can use. Important amongst them are:
- Protease: breaks down proteins (into amino acids)
- Amylase: breaks down starches (into sugars)
- Lipase: breaks down fats (into fatty acids)
All three are available as popular supplements to aid digestion. How does the science stack up for them?
Protease
For this, we only found animal studies like this one, but the results have been promising:
Amylase
Again, the studies for this alone (not combined with other enzymes) have been solely from animal agriculture; here’s an example:
The Effect of Exogenous Amylase Supplementation on the Nutritional Value of Peas
Lipase
Unlike for protease and amylase, now we have human studies as well, and here’s what they had to say:
❝Lipase supplementation significantly reduced stomach fullness without change of EGG.
Furthermore, lipase supplementation may be helpful in control of FD symptom such as postprandial symptoms❞
~ Dr. Seon-Young Park & Dr. Jong-Sun Rew
Read more: Is Lipase Supplementation before a High Fat Meal Helpful to Patients with Functional Dyspepsia?
(short answer: yes, it is)
More studies found the same, such as:
Lipase Supplementation before a High-Fat Meal Reduces Perceptions of Fullness in Healthy Subjects
All together now!
When we look at studies for combination supplementation of digestive enzymes, more has been done, and/but it’s (as you might expect) less specific.
The following paper gives a good rundown:
Pancrelipase Therapy: A Combination Of Protease, Amylase, & Lipase
Is it safe?
For most people it is quite safe, but if taking high doses for a long time it can cause problems, and also there may be complications if you have diabetes, are otherwise immunocompromised, or have some other conditions (listed towards the end of the above-linked paper, along with further information that we can’t fit in here).
As ever, check with your doctor/pharmacist if you’re not completely sure!
Want some?
We don’t sell them, but for your convenience, here’s an example product on Amazon that contains all three
Enjoy!
Share This Post
Related Posts
-
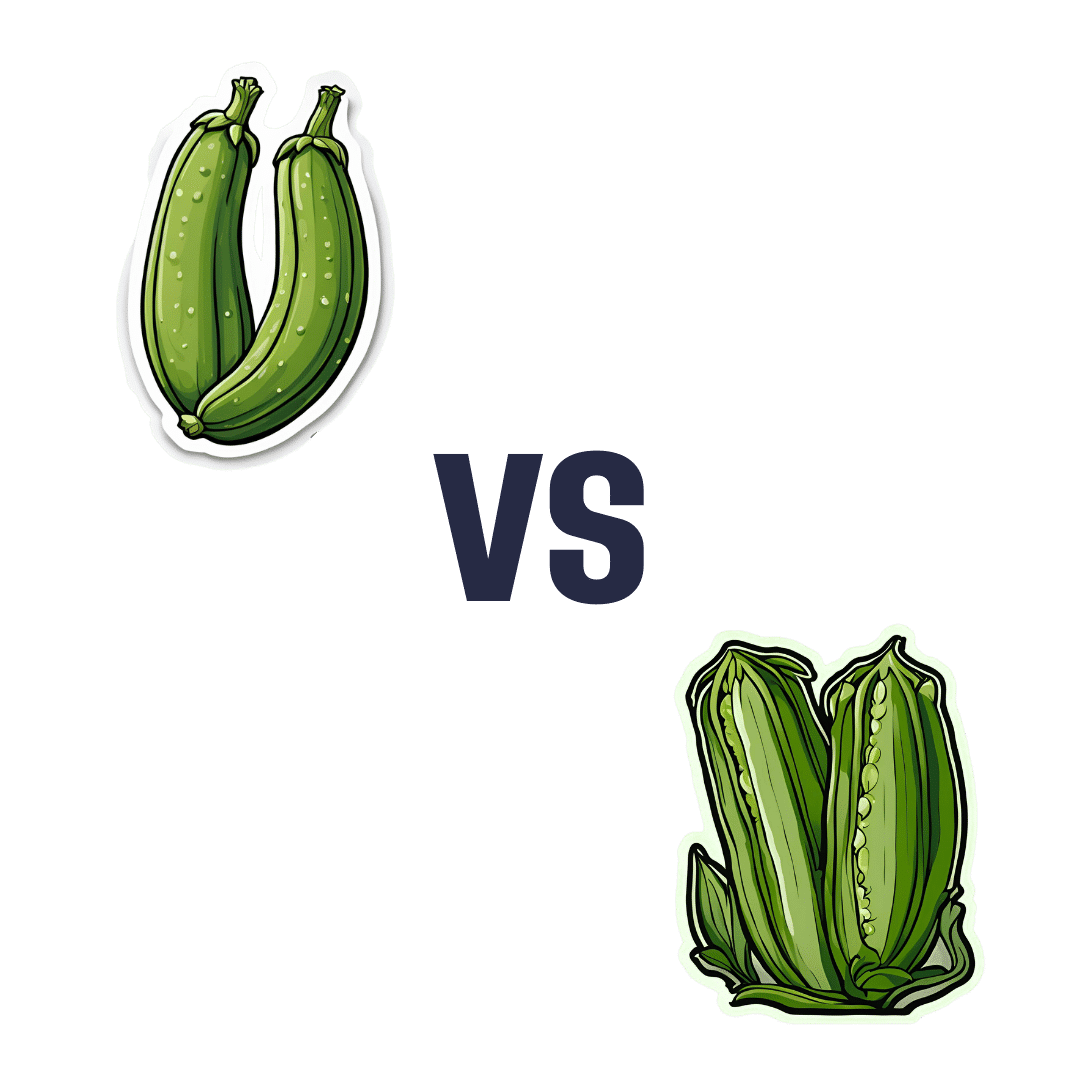
Zucchini vs Okra – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing zucchini to okra, we picked the okra.
Why?
Looking at the macros first, okra has nearly 2x the protein and more than 3x the fiber (for about 2x the carbs).
In terms of vitamins, things are also quite one-sided; zucchini has a little more vitamin B2, while okra has a lot more of vitamins A, B1, B3, B5, B6, B9, C, E, K, and choline.
Nor does the mineral situation make any compelling counterargument; zucchini is higher only in sodium, while okra has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium*, selenium, and zinc.
*Actually it’s only a little more potassium. But the rest are with big margins of difference.
Both of these on-the-cusp-of-being-pungent vegetables have beneficial antioxidant polyphenols (especially various forms of quercetin), but okra has more.
In short: enjoy both, of course, but there’s a clear winner here and it’s okra.
Want to learn more?
You might like to read:
Enjoy Bitter/Astringent/Pungent Foods For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How stigma perpetuates substance use
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2022, 54.6 million people 12 and older in the United States needed substance use disorder (SUD) treatment. Of those, only 24 percent received treatment, according to the most recent National Survey on Drug Use and Health.
SUD is a treatable, chronic medical condition that causes people to have difficulty controlling their use of legal or illegal substances, such as alcohol, tobacco, prescription opioids, heroin, methamphetamine, or cocaine. Using these substances may impact people’s health and ability to function in their daily life.
While help is available for people with SUD, the stigma they face—negative attitudes, stereotypes, and discrimination—often leads to shame, worsens their condition, and keeps them from seeking help.
Read on to find out more about how stigma perpetuates substance use.
Stigma can keep people from seeking treatment
Suzan M. Walters, assistant professor at New York University’s Grossman School of Medicine, has seen this firsthand in her research on stigma and health disparities.
She explains that people with SUD may be treated differently at a hospital or another health care setting because of their drug use, appearance (including track marks on their arms), or housing situation, which may discourage them from seeking care.
“And this is not just one case; this is a trend that I’m seeing with people who use drugs,” Walters tells PGN. “Someone said, ‘If I overdose, I’m not even going to the [emergency room] to get help because of this, because of the way I’m treated. Because I know I’m going to be treated differently.’”
People experience stigma not only because of their addiction, but also because of other aspects of their identities, Walters says, including “immigration or race and ethnicity. Hispanic folks, brown folks, Black folks [are] being treated differently and experiencing different outcomes.”
And despite the effective harm reduction tools and treatment options available for SUD, research has shown that stigma creates barriers to access.
Syringe services programs, for example, provide infectious disease testing, Narcan, and fentanyl test strips. These programs have been proven to save lives and reduce the spread of HIV and hepatitis C. SSPs don’t increase crime, but they’re often mistakenly “viewed by communities as potential settings of drug-related crime;” this myth persists despite decades of research proving that SSPs make communities safer.
To improve this bias, Walters says it’s helpful for people to take a step back and recognize how we use substances, like alcohol, in our own lives, while also humanizing those with addiction. She says, “There’s a lack of understanding that these are human beings and people … [who] are living lives, and many times very functional lives.”
Misconceptions lead to stigma
SUD results from changes in the brain that make it difficult for a person to stop using a substance. But research has shown that a big misconception that leads to stigma is that addiction is a choice and reflects a person’s willpower.
Michelle Maloney, executive clinical director of mental health and addiction recovery services for Rogers Behavioral Health, tells PGN that statements such as “you should be able to stop” can keep a patient from seeking treatment. This belief goes back to the 1980s and the War on Drugs, she adds.
“We think about public service announcements that occurred during that time: ‘Just say no to drugs,’” Maloney says. “People who have struggled, whether that be with nicotine, alcohol, or opioids, [know] it’s not as easy as just saying no.”
Stigma can worsen addiction
Stigma can also lead people with SUD to feel guilt and shame and blame themselves for their medical condition. These feelings, according to the National Institute on Drug Abuse, may “reinforce drug-seeking behavior.”
In a 2020 article, Dr. Nora D. Volkow, the director of NIDA, said that “when internalized, stigma and the painful isolation it produces encourage further drug taking, directly exacerbating the disease.”
Overall, research agrees that stigma harms people experiencing addiction and can make the condition worse. Experts also agree that debunking myths about the condition and using non-stigmatizing language (like saying someone is a person with a substance use disorder, not an addict) can go a long way toward reducing stigma.
Resources to mitigate stigma:
- CDC: Stigma Reduction
- National Harm Reduction Coalition: Respect To Connect: Undoing Stigma
- NIDA:
- Shatterproof: Addiction language guide (Disclosure: The Public Good Projects, PGN’s parent company, is a Shatterproof partner)
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Magnesium Glycinate vs Magnesium Citrate – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing magnesium glycinate to magnesium citrate, we picked the citrate.
Why?
Both are fine sources of magnesium, a nutrient in which it’s very common to be deficient—a lot of people don’t eat many leafy greens, beans, nuts, and so forth that contain it.
A quick word on a third contender we didn’t include here: magnesium oxide is probably the most widely-sold magnesium supplement because it’s cheapest to make. It also has woeful bioavailability, to the point that there seems to be negligible benefit to taking it. So we don’t recommend that.
Magnesium glycinate and magnesium citrate are both absorbed well, but magnesium citrate is the most well-absorbed form of magnesium supplement.
In terms of the relative merits of the glycine or the citric acid (the “other part” of magnesium glycinate and magnesium citrate, respectively), both are also great nutrients, but the amount delivered with the magnesium is quite small in each case, and so there’s nothing here to swing it one way or the other.
For this reason, we went with the magnesium citrate, as the most readily bioavailable!
Want to try them out?
Here they are on Amazon:
Magnesium glycinate | Magnesium citrate
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: