Energize! – by Dr. Michael Breus & Stacey Griffith
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed another book book by Dr. Breus, The Power Of When. So what’s different in this one?
While the chronotypes featured in The Power Of When also feature here (and sufficient explanation is given to make this a fine stand-alone book), this book has a lot to do with metabolism also. By considering a person’s genetically predisposed metabolic rate to be fast, medium, or slow (per being an ectomorph, mesomorph, or endomorph), and then putting that next to one’s sleep chronotype, we get 12 sub-categories that in this book each get an optimized protocol of sleep, exercise (further divided into: what kind of exercise when), and eating/fasting.
Which, in effect, amounts to a personalized coaching program for optimized energy!
The guidance is based on a combination of actual science plus “if this then that” observation-based principles—of the kind that could be described as science if they had been studied clinically instead of informally. Dr. Breus is a sleep scientist, by the way, and his co-author Stacey Griffith is a fitness coach. So between the two of them, they have sleep and exercise covered, and the fasting content is very reasonable and entirely consistent with current consensus of good practice.
The style is very pop-psychology, and very readable, and has a much more upbeat feel than The Power Of When, which seems to be because of Griffith’s presence as a co-author (most of the book is written from a neutral perspective, and some parts have first-person sections by each of the authors, so the style becomes distinct accordingly).
Bottom line: if you’d like to be more energized but [personal reason why not here] then this book may not fix all your problems, but it’ll almost certainly make a big difference and help you to stop sabotaging things and work with your body rather than against it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Psychedelics and Psychotherapy – Edited by Dr. Tim Read & Maria Papaspyrou
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note on authorship, first: this book is edited by the psychiatrist and psychotherapist credited above, but after the introductory section, the rest of the chapters are written by experts on the individual topics.As such, the style will vary somewhat, from chapter to chapter.
What this book isn’t: “try drugs and feel better!”
Rather, the book explores the various ways in which assorted drugs can help people to—even if just briefly—shed things they didn’t know they were carrying, or otherwise couldn’t put down, and access parts of themselves they otherwise couldn’t.
We also get to read a lot about the different roles the facilitator can play in guiding the therapeutic process, and what can be expected out of each kind of experience. This varies a lot from one drug to another, so it makes for very worthwhile reading, if that’s something you might consider pursuing. Knowledge makes for much more informed choices!
Bottom line: if you’re curious about the therapeutic potential of psychedelics, and want a reference that’s more personal than dry clinical studies, but still more “safe and removed” than diving in by yourself, this is the book for you.
Click here to check out Psychedelics and Psychotherapy, and expand your understanding!
Share This Post
-
Come Together – by Dr. Emily Nagoski
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From Dr. Emily Nagoski, author of the bestseller “Come As You Are” (which we reviewed very favorably before) we now present: Come Together.
What it is not about: simultaneous orgasms. The title is just a play on words.
What it is about: improving sexual wellbeing, particularly in long-term relationships where one or more partner(s) may be experiencing low desire.
Hence: come together, in the closeness sense.
A lot of books (or advice articles) out there take the Cosmo approach of “spicing things up”, and that can help for a night perhaps, but relying on novelty is not a sustainable approach.
Instead, what Dr. Nagoski outlines here is a method for focusing on shared comfort and pleasure over desire, creating the right state of mind that’s more conducive to sexuality, and reducing things that put the brakes on sexuality.
She also covers things whereby sexuality can often be obliged to change (for example, with age and/or disability), but that with the right attitude, change can sometimes just be growth in a different way, as you explore the new circumstances together, and continue to find shared pleasure in the ways that best suit your changing circumstances,
Bottom line: if you and/or your partner(s) would like to foster and maintain intimacy and pleasure, then this is a top-tier book for you.
Click here to check out Come Together, and, well, come together!
Share This Post
-
It’s OK That You’re Not OK – by Megan Devine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, be aware: this is not a cheerful book. If you’re looking for something to life your mood after a loss, it will not be this.
What, then, will you find? A reminder that grief is also the final translation of love, and not necessarily something to be put aside as quickly as possible—or even ever, if we don’t want to.
Too often, society (and even therapists) will correctly note that no two instances of grief are the same (after all, no two people are, so definitely no two relationships are, so how could two instances of grief be?), but will still expect that if most people can move on quickly from most losses, that you should too, and that if you don’t then there is something pathological at hand that needs fixing.
Part one of the book covers this (and more) in a lot of detail; critics have called it a diatribe against the current status quo in the field of grief.
Part two of the book is about “what to do with your grief”, and addresses the reality of grief, how (and why) to stay alive when not doing so feels like a compelling option, dealing with grief’s physical side effects, and calming your mind in ways that actually work (without trying to sweep your grief under a rug).
Parts three and four are more about community—how to navigate the likely unhelpful efforts a lot of people may make in the early days, and when it comes to those people who can and will actually be a support, how to help them to help you.
In the category of criticism, she also plugs her own (paid, subscription-based) online community, which feels a little mercenary, especially as while community definitely can indeed help, the prospect of being promptly exiled from it if you stop paying, doesn’t.
Bottom line: if you have experienced grief and felt like moving on was the right thing to do, then this book isn’t the one for you. If, on the other hand, your grief feels more like something you will carry just as you carry the love you feel for them, then you’ll find a lot about that here.
Share This Post
Related Posts
-
The Power of Hormones – by Dr. Max Nieuwdorp
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First a quick note on the author: he’s an MD & PhD, internist, endocrinologist, and professor. He knows his stuff.
There are a lot of books with “the new science of” in the title, and they don’t often pertain to science that is actually new, and in this case, for the most part the science contained within this book is quite well-established.
A strength of this book is that it’s not talking about hormones in just one specific aspect (e.g. menopause, pregnancy, etc) but rather, in the full span of human health, across the spectra of ages and sexes—and yes, also covering hormones that are not sex hormones, so for example also demystifying the different happiness-related neurotransmitters, as well as the hormones responsible for hunger and satiety, weight loss and gain, sleep and wakefulness, etc.
Which is all very good, because there’s a lot of overlap and several hormones fall into several categories there.
Moreover, the book covers how your personal cocktail of hormones impacts how you look, feel, behave, and more—there’s a lot about chronic health issues here too, and how to use the information in this book to if not outright cure, then at least ameliorate, many conditions.
Bottom line: this is an information-dense book with a lot of details great and small; if you read this, you’ll come away with a much better understanding of hormones than you had previously!
Click here to check out The Power of Hormones, and harness that power for yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Not to Diet – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked before about Dr. Greger’s famous “How Not To Die” book, and we love it and recommend it… But… It is, primarily, a large, dry textbook. Full of incredibly good science and information about what is statistically most likely to kill us and how to avoid that… but it’s not the most accessible.
“How Not To Diet“, on the other hand, is a diet book, is very readable, and assumes the reader would simply like to know how to healthily lose weight.
By focussing on this one problem, rather than the many (admittedly important) mortality risks, the reading is a lot easier and lighter. And, because it’s still Dr. Greger advocating for the same diet, you’ll still get to reduce all those all-cause mortality risks. You won’t be reading about them in this book; it will now just be a happy side effect.
While in “How Not To Die”, Dr. Greger looked at what was killing people and then tackled those problems, here he’s taken the same approach to just one problem… Obesity.
So, he looks at what is causing people to be overweight, and methodically tackles those problems.
We’ll not list them all here—there are many, and this is a book review, not a book summary. But suffice it to say, the work is comprehensive.
Bottom line: this book methodically and clinically (lots of science!) looks at what makes us overweight… And tackles those problems one by one, giving us a diet optimized for good health and weight loss. If you’d like to shed a few pounds in a healthy, sustainable way (that just happens to significantly reduce mortality risk from other causes too) then this is a great book for you!
Click here to check out “How Not To Diet” on Amazon and get healthy for life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
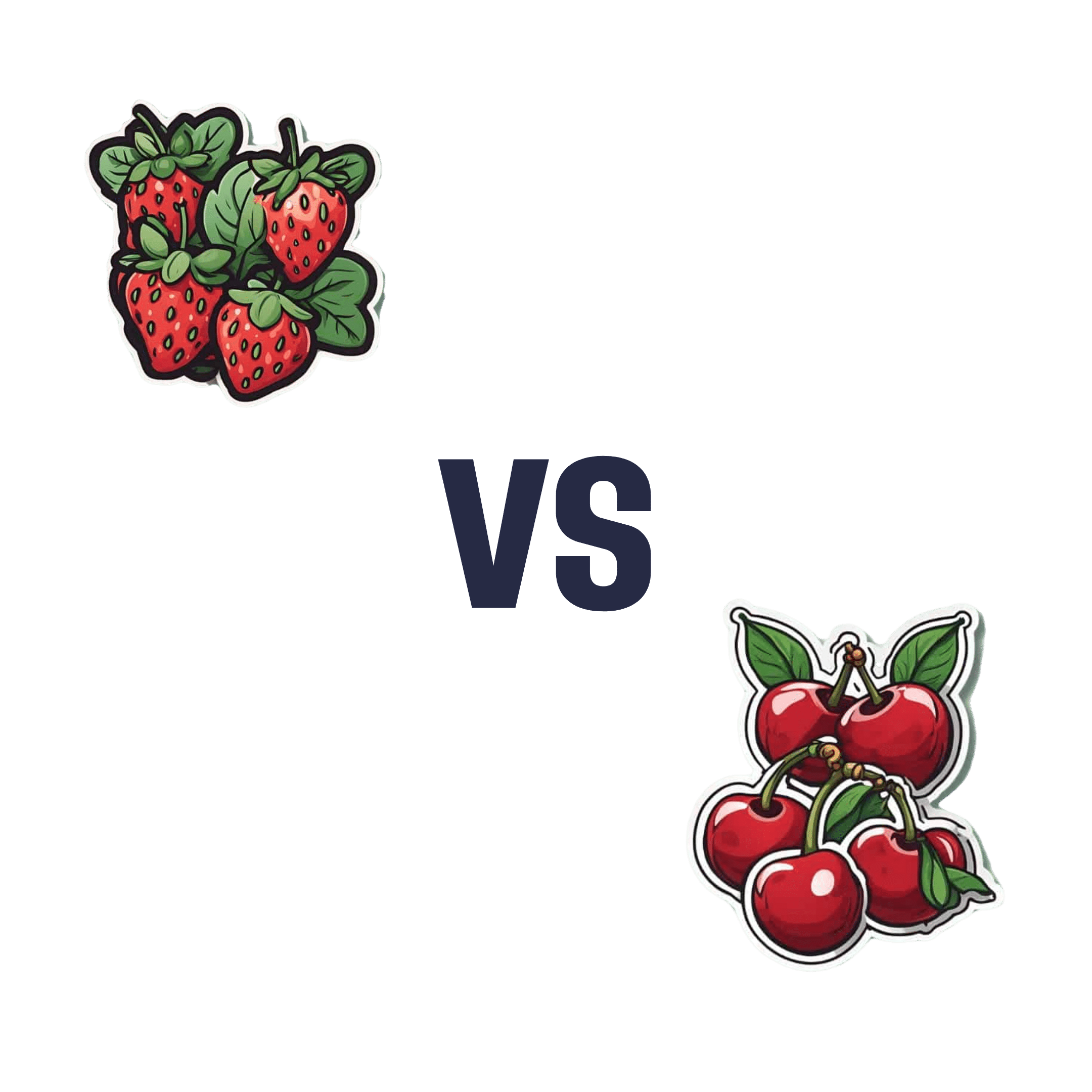
Strawberries vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing strawberries to cherries, we picked the cherries.
Why?
It was close, and certainly both are great!
When it comes to vitamins and minerals, each fruit has its strengths (and both are excellent sources of vitamins and minerals), but on balance, strawberry comes out a little higher—especially for vitamin C, as a cup of strawberries can provide the daily recommended amount already.
In terms of macros, strawberries have less sugar, but this isn’t really a big deal when it comes to fruit, as the fiber content and polyphenols more than offset any negative effects.
Speaking of which, the fiber content is comparable for each fruit, and both contain a lot of antioxidants.
What swings it into cherries’ favor is cherries’ slew of specific phytochemical benefits, including cherry-specific anti-inflammatory properties, sleep-improving abilities, and post-exercise recovery boosts, as well as anti-diabetic benefits above and beyond the normal “this is a fruit” level.
In short, both are very respectable fruits, but cherries have some qualities that are just special, and that we feel outweigh the “has more vitamin C” of strawberries.
We’ll do a main feature on cherries’ medicinal properties sometime soon, but in the meantime, if you’d like to try a tart cherry supplement, here’s an example product on Amazon
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: