Mental illness, psychiatric disorder or psychological problem. What should we call mental distress?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talk about mental health more than ever, but the language we should use remains a vexed issue.
Should we call people who seek help patients, clients or consumers? Should we use “person-first” expressions such as person with autism or “identity-first” expressions like autistic person? Should we apply or avoid diagnostic labels?
These questions often stir up strong feelings. Some people feel that patient implies being passive and subordinate. Others think consumer is too transactional, as if seeking help is like buying a new refrigerator.
Advocates of person-first language argue people shouldn’t be defined by their conditions. Proponents of identity-first language counter that these conditions can be sources of meaning and belonging.
Avid users of diagnostic terms see them as useful descriptors. Critics worry that diagnostic labels can box people in and misrepresent their problems as pathologies.
Underlying many of these disagreements are concerns about stigma and the medicalisation of suffering. Ideally the language we use should not cast people who experience distress as defective or shameful, or frame everyday problems of living in psychiatric terms.
Our new research, published in the journal PLOS Mental Health, examines how the language of distress has evolved over nearly 80 years. Here’s what we found.

Generic terms for the class of conditions
Generic terms – such as mental illness, psychiatric disorder or psychological problem – have largely escaped attention in debates about the language of mental ill health. These terms refer to mental health conditions as a class.
Many terms are currently in circulation, each an adjective followed by a noun. Popular adjectives include mental, mental health, psychiatric and psychological, and common nouns include condition, disease, disorder, disturbance, illness, and problem. Readers can encounter every combination.
These terms and their components differ in their connotations. Disease and illness sound the most medical, whereas condition, disturbance and problem need not relate to health. Mental implies a direct contrast with physical, whereas psychiatric implicates a medical specialty.
Mental health problem, a recently emerging term, is arguably the least pathologising. It implies that something is to be solved rather than treated, makes no direct reference to medicine, and carries the positive connotations of health rather than the negative connotation of illness or disease.

Arguably, this development points to what cognitive scientist Steven Pinker calls the “euphemism treadmill”, the tendency for language to evolve new terms to escape (at least temporarily) the offensive connotations of those they replace.
English linguist Hazel Price argues that mental health has increasingly come to replace mental illness to avoid the stigma associated with that term.
How has usage changed over time?
In the PLOS Mental Health paper, we examine historical changes in the popularity of 24 generic terms: every combination of the nouns and adjectives listed above.
We explore the frequency with which each term appears from 1940 to 2019 in two massive text data sets representing books in English and diverse American English sources, respectively. The findings are very similar in both data sets.
The figure presents the relative popularity of the top ten terms in the larger data set (Google Books). The 14 least popular terms are combined into the remainder.
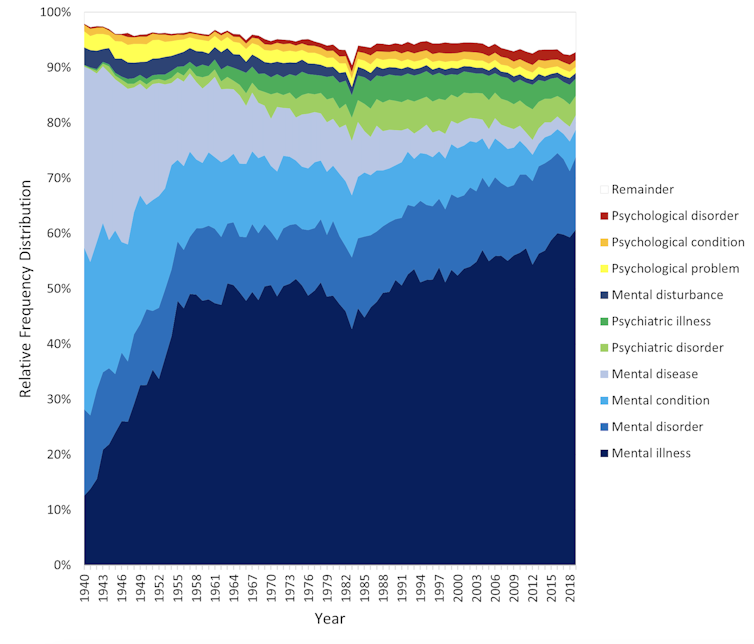
Several trends appear. Mental has consistently been the most popular adjective component of the generic terms. Mental health has become more popular in recent years but is still rarely used.
Among nouns, disease has become less widely used while illness has become dominant. Although disorder is the official term in psychiatric classifications, it has not been broadly adopted in public discourse.
Since 1940, mental illness has clearly become the preferred generic term. Although an assortment of alternatives have emerged, it has steadily risen in popularity.
Does it matter?
Our study documents striking shifts in the popularity of generic terms, but do these changes matter? The answer may be: not much.
One study found people think mental disorder, mental illness and mental health problem refer to essentially identical phenomena.
Other studies indicate that labelling a person as having a mental disease, mental disorder, mental health problem, mental illness or psychological disorder makes no difference to people’s attitudes toward them.
We don’t yet know if there are other implications of using different generic terms, but the evidence to date suggests they are minimal.

Is ‘distress’ any better?
Recently, some writers have promoted distress as an alternative to traditional generic terms. It lacks medical connotations and emphasises the person’s subjective experience rather than whether they fit an official diagnosis.
Distress appears 65 times in the 2022 Victorian Mental Health and Wellbeing Act, usually in the expression “mental illness or psychological distress”. By implication, distress is a broad concept akin to but not synonymous with mental ill health.
But is distress destigmatising, as it was intended to be? Apparently not. According to one study, it was more stigmatising than its alternatives. The term may turn us away from other people’s suffering by amplifying it.
So what should we call it?
Mental illness is easily the most popular generic term and its popularity has been rising. Research indicates different terms have little or no effect on stigma and some terms intended to destigmatise may backfire.
We suggest that mental illness should be embraced and the proliferation of alternative terms such as mental health problem, which breed confusion, should end.
Critics might argue mental illness imposes a medical frame. Philosopher Zsuzsanna Chappell disagrees. Illness, she argues, refers to subjective first-person experience, not to an objective, third-person pathology, like disease.
Properly understood, the concept of illness centres the individual and their connections. “When I identify my suffering as illness-like,” Chappell writes, “I wish to lay claim to a caring interpersonal relationship.”
As generic terms go, mental illness is a healthy option.
Nick Haslam, Professor of Psychology, The University of Melbourne and Naomi Baes, Researcher – Social Psychology/ Natural Language Processing, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Spice Of Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Great newsletter. Am taking turmeric for inflammation of hips and feet. Works like magic. Would like to know how it works, and what tumeric is best combined with – also whether there any risks in longterm use.❞
Glad you’re enjoying! As for turmeric, it sure is great, isn’t it? To answer your questions in a brief fashion:
- How it works: it does a lot of things, but perhaps its most key feature is its autoxidative metabolites that mediate its anti-inflammatory effect. Thus, it slows or inhibits oxidative stress that would otherwise cause inflammation, increase cancer risk, and advance aging.
- Best combined with: black pepper
- Any risks in long-term use: there are no known risks in long-term use ← that’s just one study, but there are lots. Some studies were prompted by reported hepatotoxicity of curcumin supplements, but a) the reports themselves seem to be without evidence b) the reported hepatoxicity was in relation to contaminants in the supplements, not the curcumin itself c) clinical trials were unable to find any hepatotoxicity (or other) risks anyway. Here’s an example of such a study.
You might also like our previous main feature: Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Share This Post
-
They Were Injured at the Super Bowl Parade. A Month Later, They Feel Forgotten.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
KFF Health News and KCUR are following the stories of people injured during the Feb. 14 mass shooting at the Kansas City Chiefs Super Bowl celebration. Listen to how one Kansas family is coping with the trauma.
Jason Barton didn’t want to attend the Super Bowl parade this year. He told a co-worker the night before that he worried about a mass shooting. But it was Valentine’s Day, his wife is a Kansas City Chiefs superfan, and he couldn’t afford to take her to games since ticket prices soared after the team won the championship in 2020.
So Barton drove 50 miles from Osawatomie, Kansas, to downtown Kansas City, Missouri, with his wife, Bridget, her 13-year-old daughter, Gabriella, and Gabriella’s school friend. When they finally arrived home that night, they cleaned blood from Gabriella’s sneakers and found a bullet in Bridget’s backpack.
Gabriella’s legs were burned by sparks from a ricocheted bullet, Bridget was trampled while shielding Gabriella in the chaos, and Jason gave chest compressions to a man injured by gunfire. He believes it was Lyndell Mays, one of two men charged with second-degree felony murder.
“There’s never going to be a Valentine’s Day where I look back and I don’t think about it,” Gabriella said, “because that’s a day where we’re supposed to have fun and appreciate the people that we have.”
One month after the parade in which the U.S. public health crisis that is gun violence played out on live television, the Bartons are reeling from their role at its epicenter. They were just feet from 43-year-old Lisa Lopez-Galvan, who was killed. Twenty-four other people were injured. Although the Bartons aren’t included in that official victim number, they were traumatized, physically and emotionally, and pain permeates their lives: Bridget and Jason keep canceling plans to go out, opting instead to stay home together; Gabriella plans to join a boxing club instead of the dance team.
During this first month, Kansas City community leaders have weighed how to care for people caught in the bloody crossfire and how to divide more than $2 million donated to public funds for victims in the initial outpouring of grief.
The questions are far-reaching: How does a city compensate people for medical bills, recovery treatments, counseling, and lost wages? And what about those who have PTSD-like symptoms that could last years? How does a community identify and care for victims often overlooked in the first flush of reporting on a mass shooting: the injured?
The injured list could grow. Prosecutors and Kansas City police are mounting a legal case against four of the shooting suspects, and are encouraging additional victims to come forward.
“Specifically, we’re looking for individuals who suffered wounds from their trying to escape. A stampede occurred while people were trying to flee,” said Jackson County Prosecutor Jean Peters Baker. Anyone who “in the fleeing of this event that maybe fell down, you were trampled, you sprained an ankle, you broke a bone.”
Meanwhile, people who took charge of raising money and providing services to care for the injured are wrestling with who gets the money — and who doesn’t. Due to large donations from celebrities like Taylor Swift and Travis Kelce, some victims or their families will have access to hundreds of thousands of dollars for medical expenses. Other victims may simply have their counseling covered.
The overall economic cost of U.S. firearm injuries is estimated by a recent Harvard Medical School study at $557 billion annually. Most of that — 88% — represented quality-of-life losses among those injured by firearms and their families. The JAMA-published study found that each nonfatal firearm injury leads to roughly $30,000 in direct health care spending per survivor in the first year alone.
In the immediate aftermath of the shootings, as well-intentioned GoFundMe pages popped up to help victims, executives at United Way of Greater Kansas City gathered to devise a collective donation response. They came up with “three concentric circles of victims,” said Jessica Blubaugh, the United Way’s chief philanthropy officer, and launched the #KCStrong campaign.
“There were folks that were obviously directly impacted by gunfire. Then the next circle out is folks that were impacted, not necessarily by gunshots, but by physical impact. So maybe they were trampled and maybe they tore a ligament or something because they were running away,” Blubaugh said. “Then third is folks that were just adjacent and/or bystanders that have a lot of trauma from all of this.”
PTSD, Panic, and the Echo of Gunfire
Bridget Barton returned to Kansas City the day after the shooting to turn in the bullet she found in her backpack and to give a statement at police headquarters. Unbeknownst to her, Mayor Quinton Lucas and the police and fire chiefs had just finished a press conference outside the building. She was mobbed by the media assembled there — interviews that are now a blur.
“I don’t know how you guys do this every day,” she remembered telling a detective once she finally got inside.
The Bartons have been overwhelmed by well wishes from close friends and family as they navigate the trauma, almost to the point of exhaustion. Bridget took to social media to explain she wasn’t ignoring the messages, she’s just responding as she feels able — some days she can hardly look at her phone, she said.
A family friend bought new Barbie blankets for Gabriella and her friend after the ones they brought to the parade were lost or ruined. Bridget tried replacing the blankets herself at her local Walmart, but when she was bumped accidentally, it triggered a panic attack. She abandoned her cart and drove home.
“I’m trying to get my anxiety under control,” Bridget said.
That means therapy. Before the parade, she was already seeing a therapist and planning to begin eye movement desensitization and reprocessing, a form of therapy associated with treating post-traumatic stress disorder. Now the shooting is the first thing she wants to talk about in therapy.
Since Gabriella, an eighth grader, has returned to middle school, she has dealt with the compounding immaturity of adolescence: peers telling her to get over it, pointing finger guns at her, or even saying it should have been her who was shot. But her friends are checking on her and asking how she’s doing. She wishes more people would do the same for her friend, who took off running when the shooting started and avoided injury. Gabriella feels guilty about bringing her to what turned into a horrifying experience.
“We can tell her all day long, ‘It wasn’t your fault. She’s not your responsibility.’ Just like I can tell myself, ‘It wasn’t my fault or my responsibility,’” Bridget said. “But I still bawled on her mom’s shoulder telling her how sorry I was that I grabbed my kid first.”
The two girls have spent a lot of time talking since the shooting, which Gabriella said helps with her own stress. So does spending time with her dog and her lizard, putting on makeup, and listening to music — Tech N9ne’s performance was a highlight of the Super Bowl celebration for her.
In addition to the spark burns on Gabriella’s legs, when she fell to the concrete in the pandemonium she split open a burn wound on her stomach previously caused by a styling iron.
“When I see that, I just picture my mom trying to protect me and seeing everyone run,” Gabriella said of the wound.
It’s hard not to feel forgotten by the public, Bridget said. The shooting, especially its survivors, have largely faded from the headlines aside from court dates. Two additional high-profile shootings have occurred in the area since the parade. Doesn’t the community care, she wonders, that her family is still living with the fallout every day?
“I’m going to put this as plainly as possible. I’m f—ing pissed because my family went through something traumatic,” Bridget vented in a recent social media post. “I don’t really want anything other [than], ‘Your story matters, too, and we want to know how you’re doing.’ Have we gotten that? Abso-f—lutely not.”
‘What Is the Landscape of Need?’
Helped in part by celebrities like Swift and Kelce, donations for the family of Lopez-Galvan, the lone fatality, and other victims poured in immediately after the shootings. Swift and Kelce donated $100,000 each. With the help of an initial $200,000 donation from the Kansas City Chiefs, the United Way’s #KCStrong campaign took off, reaching $1 million in the first two weeks and sitting at $1.2 million now.
Six verified GoFundMe funds were established. One solely for the Lopez-Galvan family has collected over $406,000. Smaller ones were started by a local college student and Swift fans. Churches have also stepped up, and one local coalition had raised $183,000, money set aside for Lopez-Galvan’s funeral, counseling services for five victims, and other medical bills from Children’s Mercy Kansas City hospital, said Ray Jarrett, executive director of Unite KC.
Money for Victims Rolls In
Donations poured in for those injured at the Super Bowl Parade in Kansas City after the Feb. 14 shootings. The largest, starting with a $200,000 donation from the Kansas City Chiefs, is at the United Way of Greater Kansas City. Six GoFundMe sites also popped up, due in part to $100,000 donations each from Taylor Swift and Travis Kelce. Here’s a look at the totals as of March 12.United Way#KCStrong: $1.2 million.Six Verified GoFundMe AccountsLisa Lopez-Galvan GoFundMe (Taylor Swift donated): $406,142Reyes Family GoFundMe (Travis Kelce donated): $207,035Samuel Arellano GoFundMe: $11,896Emily Tavis GoFundMe: $9,518Cristian Martinez’s GoFundMe for United Way: $2,967Swifties’ GoFundMe for Children’s Mercy hospital: $1,060ChurchesResurrection (Methodist) “Victims of Violence Fund”: $53,358‘The Church Loves Kansas City’: $183,000
Meanwhile, those leading the efforts found models in other cities. The United Way’s Blubaugh called counterparts who’d responded to their own mass shootings in Orlando, Florida; Buffalo, New York; and Newtown, Connecticut.
“The unfortunate reality is we have a cadre of communities across the country who have already faced tragedies like this,” Blubaugh said. “So there is an unfortunate protocol that is, sort of, already in place.”
#KCStrong monies could start being paid out by the end of March, Blubaugh said. Hundreds of people called the nonprofit’s 211 line, and the United Way is consulting with hospitals and law enforcement to verify victims and then offer services they may need, she said.
The range of needs is staggering — several people are still recovering at home, some are seeking counseling, and many weren’t even counted in the beginning. For instance, a plainclothes police officer was injured in the melee but is doing fine now, said Police Chief Stacey Graves.
Determining who is eligible for assistance was one of the first conversations United Way officials had when creating the fund. They prioritized three areas of focus: first were the wounded victims and their families, second was collaborating with organizations already helping victims in violence intervention and prevention and mental health services, and third were the first responders.
Specifically, the funds will be steered to cover medical bills, or lost wages for those who haven’t been able to work since the shootings, Blubaugh said. The goal is to work quickly to help people, she said, but also to spend the money in a judicious, strategic way.
“We don’t have a clear sightline of the entire landscape that we’re dealing with,” Blubaugh said. “Not only of how much money do we have to work with, but also, what is the landscape of need? And we need both of those things to be able to make those decisions.”
Firsthand Experience of Daily Kansas City Violence
Jason used his lone remaining sick day to stay home with Bridget and Gabriella. An overnight automation technician, he is the family’s primary breadwinner.
“I can’t take off work, you know?” he said. “It happened. It sucked. But it’s time to move on.”
“He’s a guy’s guy,” Bridget interjected.
On Jason’s first night back at work, the sudden sound of falling dishes startled Bridget and Gabriella, sending them into each other’s arms crying.
“It’s just those moments of flashbacks that are kicking our butts,” Bridget said.
Tell Us About Your Experience
We are continuing to report on the effects of the parade shooting on the people who were injured and the community as a whole. Do you have an experience you want to tell us about, or a question you think we should look into? Message KCUR’s text line at (816) 601-4777. Your information will not be used in an article without your permission.
In a way, the shooting has brought the family closer. They’ve been through a lot recently. Jason survived a heart attack and cancer last year. Raising a teenager is never easy.
Bridget can appreciate that the bullet lodged in her backpack, narrowly missing her, and that Gabriella’s legs were burned by sparks but she wasn’t shot.
Jason is grateful for another reason: It wasn’t a terrorist attack, as he initially feared. Instead, it fits into the type of gun violence he’d become accustomed to growing up in Kansas City, which recorded its deadliest year last year, although he’d never been this close to it before.
“This crap happens every single day,” he said. “The only difference is we were here for it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
What causes food cravings? And what can we do about them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Many of us try to eat more fruits and vegetables and less ultra-processed food. But why is sticking to your goals so hard?
High-fat, sugar-rich and salty foods are simply so enjoyable to eat. And it’s not just you – we’ve evolved that way. These foods activate the brain’s reward system because in the past they were rare.
Now, they’re all around us. In wealthy modern societies we are bombarded by advertising which intentionally reminds us about the sight, smell and taste of calorie-dense foods. And in response to these powerful cues, our brains respond just as they’re designed to, triggering an intense urge to eat them.
Here’s how food cravings work and what you can do if you find yourself hunting for sweet or salty foods.
Fascinadora/Shutterstock What causes cravings?
A food craving is an intense desire or urge to eat something, often focused on a particular food.
We are programmed to learn how good a food tastes and smells and where we can find it again, especially if it’s high in fat, sugar or salt.
Something that reminds us of enjoying a certain food, such as an eye-catching ad or delicious smell, can cause us to crave it.
Our brains learn to crave foods based on what we’ve enjoyed before. fon thachakul/Shutterstock The cue triggers a physical response, increasing saliva production and gastric activity. These responses are relatively automatic and difficult to control.
What else influences our choices?
While the effect of cues on our physical response is relatively automatic, what we do next is influenced by complex factors.
Whether or not you eat the food might depend on things like cost, whether it’s easily available, and if eating it would align with your health goals.But it’s usually hard to keep healthy eating in mind. This is because we tend to prioritise a more immediate reward, like the pleasure of eating, over one that’s delayed or abstract – including health goals that will make us feel good in the long term.
Stress can also make us eat more. When hungry, we choose larger portions, underestimate calories and find eating more rewarding.
Looking for something salty or sweet
So what if a cue prompts us to look for a certain food, but it’s not available?
Previous research suggested you would then look for anything that makes you feel good. So if you saw someone eating a doughnut but there were none around, you might eat chips or even drink alcohol.
But our new research has confirmed something you probably knew: it’s more specific than that.
If an ad for chips makes you look for food, it’s likely a slice of cake won’t cut it – you’ll be looking for something salty. Cues in our environment don’t just make us crave food generally, they prompt us to look for certain food “categories”, such as salty, sweet or creamy.
Food cues and mindless eating
Your eating history and genetics can also make it harder to suppress food cravings. But don’t beat yourself up – relying on willpower alone is hard for almost everyone.
Food cues are so powerful they can prompt us to seek out a certain food, even if we’re not overcome by a particularly strong urge to eat it. The effect is more intense if the food is easily available.
This helps explain why we can eat an entire large bag of chips that’s in front of us, even though our pleasure decreases as we eat. Sometimes we use finishing the packet as the signal to stop eating rather than hunger or desire.
Is there anything I can do to resist cravings?
We largely don’t have control over cues in our environment and the cravings they trigger. But there are some ways you can try and control the situations you make food choices in.
- Acknowledge your craving and think about a healthier way to satisfy it. For example, if you’re craving chips, could you have lightly-salted nuts instead? If you want something sweet, you could try fruit.
- Avoid shopping when you’re hungry, and make a list beforehand. Making the most of supermarket “click and collect” or delivery options can also help avoid ads and impulse buys in the aisle.
- At home, have fruit and vegetables easily available – and easy to see. Also have other nutrient dense, fibre-rich and unprocessed foods on hand such as nuts or plain yoghurt. If you can, remove high-fat, sugar-rich and salty foods from your environment.
- Make sure your goals for eating are SMART. This means they are specific, measurable, achievable, relevant and time-bound.
- Be kind to yourself. Don’t beat yourself up if you eat something that doesn’t meet your health goals. Just keep on trying.
Gabrielle Weidemann, Associate Professor in Psychological Science, Western Sydney University and Justin Mahlberg, Research Fellow, Pyschology, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Diet Tips for Crohn’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We’re the ‘allergy capital of the world’. But we don’t know why food allergies are so common in Australian children
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia has often been called the “allergy capital of the world”.
An estimated one in ten Australian children develop a food allergy in their first 12 months of life. Research has previously suggested food allergies are more common in infants in Australia than infants living in Europe, the United States or Asia.
So why are food allergies so common in Australia? We don’t know exactly – but local researchers are making progress in understanding childhood allergies all the time.
Miljan Zivkovic/Shutterstock What causes food allergies?
There are many different types of reactions to foods. When we refer to food allergies in this article, we’re talking about something called IgE-mediated food allergy. This type of allergy is caused by an immune response to a particular food.
Reactions can occur within minutes of eating the food and may include swelling of the face, lips or eyes, “hives” or welts on the skin, and vomiting. Signs of a severe allergic reaction (anaphylaxis) include difficulty breathing, swelling of the tongue, swelling in the throat, wheeze or persistent cough, difficulty talking or a hoarse voice, and persistent dizziness or collapse.
Recent results from Australia’s large, long-running food allergy study, HealthNuts, show one in ten one-year-olds have a food allergy, while around six in 100 children have a food allergy at age ten.
A food allergy can present with skin reactions. comzeal images/Shutterstock In Australia, the most common allergy-causing foods include eggs, peanuts, cow’s milk, shellfish (for example, prawn and lobster), fish, tree nuts (for example, walnuts and cashews), soybeans and wheat.
Allergies to foods like eggs, peanuts and cow’s milk often present for the first time in infancy, while allergies to fish and shellfish may be more common later in life. While most children will outgrow their allergies to eggs and milk, allergy to peanuts is more likely to be lifelong.
Findings from HealthNuts showed around three in ten children grew out of their peanut allergy by age six, compared to nine in ten children with an allergy to egg.
Are food allergies becoming more common?
Food allergies seem to have become more common in many countries around the world over recent decades. The exact timing of this increase is not clear, because in most countries food allergies were not well measured 40 or 50 years ago.
We don’t know exactly why food allergies are so common in Australia, or why we’re seeing a rise around the world, despite extensive research.
But possible reasons for rising allergies around the world include changes in the diets of mothers and infants and increasing sanitisation, leading to fewer infections as well as less exposure to “good” bacteria. In Australia, factors such as increasing vitamin D deficiency among infants and high levels of migration to the country could play a role.
In several Australian studies, children born in Australia to parents who were born in Asia have higher rates of food allergies compared to non-Asian children. On the other hand, children who were born in Asia and later migrated to Australia appear to have a lower risk of nut allergies.
Meanwhile, studies have shown that having pet dogs and siblings as a young child may reduce the risk of food allergies. This might be because having pet dogs and siblings increases contact with a range of bacteria and other organisms.
This evidence suggests that both genetics and environment play a role in the development of food allergies.
We also know that infants with eczema are more likely to develop a food allergy, and trials are underway to see whether this link can be broken.
Can I do anything to prevent food allergies in my kids?
One of the questions we are asked most often by parents is “can we do anything to prevent food allergies?”.
We now know introducing peanuts and eggs from around six months of age makes it less likely that an infant will develop an allergy to these foods. The Australasian Society of Clinical Immunology and Allergy introduced guidelines recommending giving common allergy-causing foods including peanut and egg in the first year of life in 2016.
Our research has shown this advice had excellent uptake and may have slowed the rise in food allergies in Australia. There was no increase in peanut allergies between 2007–11 to 2018–19.
Introducing other common allergy-causing foods in the first year of life may also be helpful, although the evidence for this is not as strong compared with peanuts and eggs.
Giving kids peanuts early can reduce the risk of a peanut allergy. Madame-Moustache/Shutterstock What next?
Unfortunately, some infants will develop food allergies even when the relevant foods are introduced in the first year of life. Managing food allergies can be a significant burden for children and families.
Several Australian trials are currently underway testing new strategies to prevent food allergies. A large trial, soon to be completed, is testing whether vitamin D supplements in infants reduce the risk of food allergies.
Another trial is testing whether the amount of eggs and peanuts a mother eats during pregnancy and breastfeeding has an influence on whether or not her baby will develop food allergies.
For most people with food allergies, avoidance of their known allergens remains the standard of care. Oral immunotherapy, which involves gradually increasing amounts of food allergen given under medical supervision, is beginning to be offered in some facilities around Australia. However, current oral immunotherapy methods have potential side effects (including allergic reactions), can involve high time commitment and cost, and don’t cure food allergies.
There is hope on the horizon for new food allergy treatments. Multiple clinical trials are underway around Australia aiming to develop safer and more effective treatments for people with food allergies.
Jennifer Koplin, Group Leader, Childhood Allergy & Epidemiology, The University of Queensland and Desalegn Markos Shifti, Postdoctoral Research Fellow, Child Health Research Centre, Faculty of Medicine, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Older, Faster, Stronger – by Margaret Webb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, now in her 60s, made it her mission in her 50s to become the best runner she could. Before that, she’d been a keen runner previously, but let things slip rather in her 40s. But the book’s not about her 40s, it’s about her 50s and onwards, and other female runners in their 50s, 60s, 70s, 80s, and even 90s.
There’s a lot of this book that’s about people’s individual stories, and those should certainly be enough to prompt almost any reader that “if they can do it, I can”.
A lot, meanwhile, is about health and exercise science, training methods, and what has worked for various later-life athletes, including the author. So, it’s also partway instruction manual, with plenty of reference to science and medical considerations too.
Bottom line: sometimes, life throws us challenges. Sometimes, the best response is “Yeah? Bet” and surprise everyone.
Click here to check out Older, Faster, Stronger, and become all those cool things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: