25 Healthy Habits That Will Change Your Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowith, of “Redefining Strength” and “Strong At Every Age” fame, has compiled a list of the simple habits that make a big difference, and here they are!
The Tips
Her recommendations include…
- The healthy activities you’re most prone to skipping? Do those first
- Create staple meals… Consciously! This means: instead of getting into a rut of cooking the same few things in rotation because it’s what you have the ingredients in for, consciously and deliberately make a list of at least 7 meals that, between them, constitute a healthy balanced diet, and choose to make them your staples. That doesn’t mean don’t eat anything else (indeed, variety is good!) but having a robust collection of healthy staples to fall back on will help you avoid falling into unhealthy eating traps.
- Schedule time for healthy activities that you love. Instead of thinking “it would be nice to…”, actually figure out a timeslot, plan in advance, making it recurring, and do it!
- Have (healthy!) no-spoil food options always available. No-spoil doesn’t have to mean “won’t spoil ever”, but does mean at least that it has a long shelf-life. Nuts are a good example, assuming you’re not allergic. Sundried fruits are good too; not nearly as good as fresh fruit, but a lot better than some random processed snack because it’s what in. If you eat fish, then see if you can get dried fish in; it’s high in protein and keeps for a very long time indeed.
- Stock up on spices! Not only do they all have great health-giving properties (at least, we can’t think of a refutation by counterexample, Arrakis be damned), but also, they literally spice up our culinary repertoire, and bring joy to cooking and eating healthy food.
If you like these, check out the rest:
Click Here If The Embedded Video Doesn’t Load Automatically
Further reading
For more about actually making habits stick quickly and reliably,enjoy:
How To Really Pick Up (And Keep!) Those Habits
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Signs Of Iodine Deficiency You Might Not Expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Coach Kait (BSc Nutrition & Exercise) is a certified health and nutrition coach, and today she’s here to talk about iodine—which is important for many of our body functions, from thyroid hormone production to metabolic regulation to heart rate management, as well as more superficial-but-important-too things like our skin and hair.
Kait’s hitlist
Here’s what she recommends we look out for:
- Swollen neck: even a slightly swollen neck might indicate low iodine levels (this is because that’s where the thyroid glands are)
- Hair loss: iodine is needed for healthy hair growth, so a deficiency can lead to hair loss / thinning hair
- Dry and flaky skin: with iodine’s role in our homeostatic system not being covered, our skin can dry out as a result
- Feeling cold all the time: because of iodine’s temperature-regulating activities
- Slow heart rate: A metabolic slump due to iodine deficiency can slow down the heart rate, leading to fatigue and weakness (and worse, if it persists)
- Brain fog: trouble focusing can be a symptom of the same metabolic slump
- Fatigue: this is again more or less the same thing, but she said eight signs, so we’re giving you the eight!
- Irregular period (if you normally have such, of course): because iodine affects reproductive hormones too, an imbalance can disrupt menstrual cycles.
For more on each of these, as well as how to get more iodine in your diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might also like to read:
- A Fresh Take On Hypothyroidism
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Eat To Beat Hyperthyroidism!
Take care!
Share This Post
-
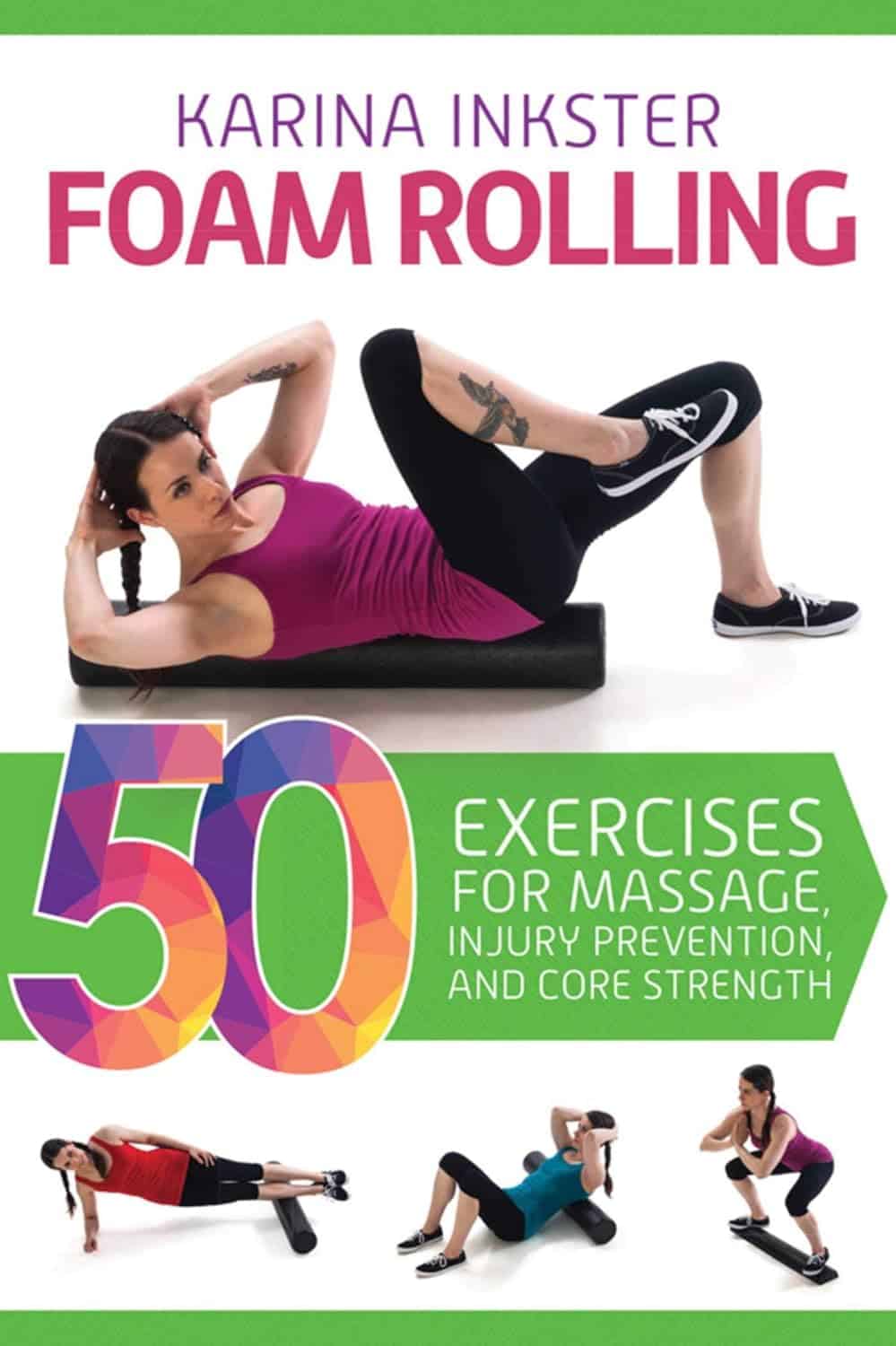
Foam Rolling – by Karina Inkster
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever bought a foam roller only to place it under your lower back once and then put it somewhere for safekeeping and never use it again, this book will help fix that.
Karina Inkster (what a cool name) is a personal trainer, and the book also features tips and advice from physiotherapists and sports medicine specialist doctors too, so all bases are well and truly covered.
This is not, in case you’re wondering, a book that could have been a pamphlet, with photos of the exercises and one-liner explanation and that’s it. Rather, Inkster takes us through the anatomy and physiology of what’s going on, so that we can actually use this thing correctly and get actual noticeable improvements to our health from it—as promised in the subtitle’s mention of “for massage, injury prevention, and core strength”. To be clear, a lot of it is also about soft tissue mobilization, and keeping our fascia healthy (an oft-underestimated aspect of general mobility).
We would mention that since the photos are pleasantly colorful (like those on the cover) and this adds to the clarity, we’d recommend springing for the (quite inexpensive) physical copy, rather than a Kindle edition (if your e-reader is a monochrome e-ink device like this reviewer’s, anyway).
Bottom line: this book will enable your foam roller to make a difference to your life.
Click here to check out Foam Rolling, and get rolling (correctly)!
Share This Post
-
They Were Injured at the Super Bowl Parade. A Month Later, They Feel Forgotten.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
KFF Health News and KCUR are following the stories of people injured during the Feb. 14 mass shooting at the Kansas City Chiefs Super Bowl celebration. Listen to how one Kansas family is coping with the trauma.
Jason Barton didn’t want to attend the Super Bowl parade this year. He told a co-worker the night before that he worried about a mass shooting. But it was Valentine’s Day, his wife is a Kansas City Chiefs superfan, and he couldn’t afford to take her to games since ticket prices soared after the team won the championship in 2020.
So Barton drove 50 miles from Osawatomie, Kansas, to downtown Kansas City, Missouri, with his wife, Bridget, her 13-year-old daughter, Gabriella, and Gabriella’s school friend. When they finally arrived home that night, they cleaned blood from Gabriella’s sneakers and found a bullet in Bridget’s backpack.
Gabriella’s legs were burned by sparks from a ricocheted bullet, Bridget was trampled while shielding Gabriella in the chaos, and Jason gave chest compressions to a man injured by gunfire. He believes it was Lyndell Mays, one of two men charged with second-degree felony murder.
“There’s never going to be a Valentine’s Day where I look back and I don’t think about it,” Gabriella said, “because that’s a day where we’re supposed to have fun and appreciate the people that we have.”
One month after the parade in which the U.S. public health crisis that is gun violence played out on live television, the Bartons are reeling from their role at its epicenter. They were just feet from 43-year-old Lisa Lopez-Galvan, who was killed. Twenty-four other people were injured. Although the Bartons aren’t included in that official victim number, they were traumatized, physically and emotionally, and pain permeates their lives: Bridget and Jason keep canceling plans to go out, opting instead to stay home together; Gabriella plans to join a boxing club instead of the dance team.
During this first month, Kansas City community leaders have weighed how to care for people caught in the bloody crossfire and how to divide more than $2 million donated to public funds for victims in the initial outpouring of grief.
The questions are far-reaching: How does a city compensate people for medical bills, recovery treatments, counseling, and lost wages? And what about those who have PTSD-like symptoms that could last years? How does a community identify and care for victims often overlooked in the first flush of reporting on a mass shooting: the injured?
The injured list could grow. Prosecutors and Kansas City police are mounting a legal case against four of the shooting suspects, and are encouraging additional victims to come forward.
“Specifically, we’re looking for individuals who suffered wounds from their trying to escape. A stampede occurred while people were trying to flee,” said Jackson County Prosecutor Jean Peters Baker. Anyone who “in the fleeing of this event that maybe fell down, you were trampled, you sprained an ankle, you broke a bone.”
Meanwhile, people who took charge of raising money and providing services to care for the injured are wrestling with who gets the money — and who doesn’t. Due to large donations from celebrities like Taylor Swift and Travis Kelce, some victims or their families will have access to hundreds of thousands of dollars for medical expenses. Other victims may simply have their counseling covered.
The overall economic cost of U.S. firearm injuries is estimated by a recent Harvard Medical School study at $557 billion annually. Most of that — 88% — represented quality-of-life losses among those injured by firearms and their families. The JAMA-published study found that each nonfatal firearm injury leads to roughly $30,000 in direct health care spending per survivor in the first year alone.
In the immediate aftermath of the shootings, as well-intentioned GoFundMe pages popped up to help victims, executives at United Way of Greater Kansas City gathered to devise a collective donation response. They came up with “three concentric circles of victims,” said Jessica Blubaugh, the United Way’s chief philanthropy officer, and launched the #KCStrong campaign.
“There were folks that were obviously directly impacted by gunfire. Then the next circle out is folks that were impacted, not necessarily by gunshots, but by physical impact. So maybe they were trampled and maybe they tore a ligament or something because they were running away,” Blubaugh said. “Then third is folks that were just adjacent and/or bystanders that have a lot of trauma from all of this.”
PTSD, Panic, and the Echo of Gunfire
Bridget Barton returned to Kansas City the day after the shooting to turn in the bullet she found in her backpack and to give a statement at police headquarters. Unbeknownst to her, Mayor Quinton Lucas and the police and fire chiefs had just finished a press conference outside the building. She was mobbed by the media assembled there — interviews that are now a blur.
“I don’t know how you guys do this every day,” she remembered telling a detective once she finally got inside.
The Bartons have been overwhelmed by well wishes from close friends and family as they navigate the trauma, almost to the point of exhaustion. Bridget took to social media to explain she wasn’t ignoring the messages, she’s just responding as she feels able — some days she can hardly look at her phone, she said.
A family friend bought new Barbie blankets for Gabriella and her friend after the ones they brought to the parade were lost or ruined. Bridget tried replacing the blankets herself at her local Walmart, but when she was bumped accidentally, it triggered a panic attack. She abandoned her cart and drove home.
“I’m trying to get my anxiety under control,” Bridget said.
That means therapy. Before the parade, she was already seeing a therapist and planning to begin eye movement desensitization and reprocessing, a form of therapy associated with treating post-traumatic stress disorder. Now the shooting is the first thing she wants to talk about in therapy.
Since Gabriella, an eighth grader, has returned to middle school, she has dealt with the compounding immaturity of adolescence: peers telling her to get over it, pointing finger guns at her, or even saying it should have been her who was shot. But her friends are checking on her and asking how she’s doing. She wishes more people would do the same for her friend, who took off running when the shooting started and avoided injury. Gabriella feels guilty about bringing her to what turned into a horrifying experience.
“We can tell her all day long, ‘It wasn’t your fault. She’s not your responsibility.’ Just like I can tell myself, ‘It wasn’t my fault or my responsibility,’” Bridget said. “But I still bawled on her mom’s shoulder telling her how sorry I was that I grabbed my kid first.”
The two girls have spent a lot of time talking since the shooting, which Gabriella said helps with her own stress. So does spending time with her dog and her lizard, putting on makeup, and listening to music — Tech N9ne’s performance was a highlight of the Super Bowl celebration for her.
In addition to the spark burns on Gabriella’s legs, when she fell to the concrete in the pandemonium she split open a burn wound on her stomach previously caused by a styling iron.
“When I see that, I just picture my mom trying to protect me and seeing everyone run,” Gabriella said of the wound.
It’s hard not to feel forgotten by the public, Bridget said. The shooting, especially its survivors, have largely faded from the headlines aside from court dates. Two additional high-profile shootings have occurred in the area since the parade. Doesn’t the community care, she wonders, that her family is still living with the fallout every day?
“I’m going to put this as plainly as possible. I’m f—ing pissed because my family went through something traumatic,” Bridget vented in a recent social media post. “I don’t really want anything other [than], ‘Your story matters, too, and we want to know how you’re doing.’ Have we gotten that? Abso-f—lutely not.”
‘What Is the Landscape of Need?’
Helped in part by celebrities like Swift and Kelce, donations for the family of Lopez-Galvan, the lone fatality, and other victims poured in immediately after the shootings. Swift and Kelce donated $100,000 each. With the help of an initial $200,000 donation from the Kansas City Chiefs, the United Way’s #KCStrong campaign took off, reaching $1 million in the first two weeks and sitting at $1.2 million now.
Six verified GoFundMe funds were established. One solely for the Lopez-Galvan family has collected over $406,000. Smaller ones were started by a local college student and Swift fans. Churches have also stepped up, and one local coalition had raised $183,000, money set aside for Lopez-Galvan’s funeral, counseling services for five victims, and other medical bills from Children’s Mercy Kansas City hospital, said Ray Jarrett, executive director of Unite KC.
Money for Victims Rolls In
Donations poured in for those injured at the Super Bowl Parade in Kansas City after the Feb. 14 shootings. The largest, starting with a $200,000 donation from the Kansas City Chiefs, is at the United Way of Greater Kansas City. Six GoFundMe sites also popped up, due in part to $100,000 donations each from Taylor Swift and Travis Kelce. Here’s a look at the totals as of March 12.United Way#KCStrong: $1.2 million.Six Verified GoFundMe AccountsLisa Lopez-Galvan GoFundMe (Taylor Swift donated): $406,142Reyes Family GoFundMe (Travis Kelce donated): $207,035Samuel Arellano GoFundMe: $11,896Emily Tavis GoFundMe: $9,518Cristian Martinez’s GoFundMe for United Way: $2,967Swifties’ GoFundMe for Children’s Mercy hospital: $1,060ChurchesResurrection (Methodist) “Victims of Violence Fund”: $53,358‘The Church Loves Kansas City’: $183,000
Meanwhile, those leading the efforts found models in other cities. The United Way’s Blubaugh called counterparts who’d responded to their own mass shootings in Orlando, Florida; Buffalo, New York; and Newtown, Connecticut.
“The unfortunate reality is we have a cadre of communities across the country who have already faced tragedies like this,” Blubaugh said. “So there is an unfortunate protocol that is, sort of, already in place.”
#KCStrong monies could start being paid out by the end of March, Blubaugh said. Hundreds of people called the nonprofit’s 211 line, and the United Way is consulting with hospitals and law enforcement to verify victims and then offer services they may need, she said.
The range of needs is staggering — several people are still recovering at home, some are seeking counseling, and many weren’t even counted in the beginning. For instance, a plainclothes police officer was injured in the melee but is doing fine now, said Police Chief Stacey Graves.
Determining who is eligible for assistance was one of the first conversations United Way officials had when creating the fund. They prioritized three areas of focus: first were the wounded victims and their families, second was collaborating with organizations already helping victims in violence intervention and prevention and mental health services, and third were the first responders.
Specifically, the funds will be steered to cover medical bills, or lost wages for those who haven’t been able to work since the shootings, Blubaugh said. The goal is to work quickly to help people, she said, but also to spend the money in a judicious, strategic way.
“We don’t have a clear sightline of the entire landscape that we’re dealing with,” Blubaugh said. “Not only of how much money do we have to work with, but also, what is the landscape of need? And we need both of those things to be able to make those decisions.”
Firsthand Experience of Daily Kansas City Violence
Jason used his lone remaining sick day to stay home with Bridget and Gabriella. An overnight automation technician, he is the family’s primary breadwinner.
“I can’t take off work, you know?” he said. “It happened. It sucked. But it’s time to move on.”
“He’s a guy’s guy,” Bridget interjected.
On Jason’s first night back at work, the sudden sound of falling dishes startled Bridget and Gabriella, sending them into each other’s arms crying.
“It’s just those moments of flashbacks that are kicking our butts,” Bridget said.
Tell Us About Your Experience
We are continuing to report on the effects of the parade shooting on the people who were injured and the community as a whole. Do you have an experience you want to tell us about, or a question you think we should look into? Message KCUR’s text line at (816) 601-4777. Your information will not be used in an article without your permission.
In a way, the shooting has brought the family closer. They’ve been through a lot recently. Jason survived a heart attack and cancer last year. Raising a teenager is never easy.
Bridget can appreciate that the bullet lodged in her backpack, narrowly missing her, and that Gabriella’s legs were burned by sparks but she wasn’t shot.
Jason is grateful for another reason: It wasn’t a terrorist attack, as he initially feared. Instead, it fits into the type of gun violence he’d become accustomed to growing up in Kansas City, which recorded its deadliest year last year, although he’d never been this close to it before.
“This crap happens every single day,” he said. “The only difference is we were here for it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
WHO Overturns Dogma on Airborne Disease Spread. The CDC Might Not Act on It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization has issued a report that transforms how the world understands respiratory infections like covid-19, influenza, and measles.
Motivated by grave missteps in the pandemic, the WHO convened about 50 experts in virology, epidemiology, aerosol science, and bioengineering, among other specialties, who spent two years poring through the evidence on how airborne viruses and bacteria spread.
However, the WHO report stops short of prescribing actions that governments, hospitals, and the public should take in response. It remains to be seen how the Centers for Disease Control and Prevention will act on this information in its own guidance for infection control in health care settings.
The WHO concluded that airborne transmission occurs as sick people exhale pathogens that remain suspended in the air, contained in tiny particles of saliva and mucus that are inhaled by others.
While it may seem obvious, and some researchers have pushed for this acknowledgment for more than a decade, an alternative dogma persisted — which kept health authorities from saying that covid was airborne for many months into the pandemic.
Specifically, they relied on a traditional notion that respiratory viruses spread mainly through droplets spewed out of an infected person’s nose or mouth. These droplets infect others by landing directly in their mouth, nose, or eyes — or they get carried into these orifices on droplet-contaminated fingers. Although these routes of transmission still happen, particularly among young children, experts have concluded that many respiratory infections spread as people simply breathe in virus-laden air.
“This is a complete U-turn,” said Julian Tang, a clinical virologist at the University of Leicester in the United Kingdom, who advised the WHO on the report. He also helped the agency create an online tool to assess the risk of airborne transmission indoors.
Peg Seminario, an occupational health and safety specialist in Bethesda, Maryland, welcomed the shift after years of resistance from health authorities. “The dogma that droplets are a major mode of transmission is the ‘flat Earth’ position now,” she said. “Hurray! We are finally recognizing that the world is round.”
The change puts fresh emphasis on the need to improve ventilation indoors and stockpile quality face masks before the next airborne disease explodes. Far from a remote possibility, measles is on the rise this year and the H5N1 bird flu is spreading among cattle in several states. Scientists worry that as the H5N1 virus spends more time in mammals, it could evolve to more easily infect people and spread among them through the air.
Traditional beliefs on droplet transmission help explain why the WHO and the CDC focused so acutely on hand-washing and surface-cleaning at the beginning of the pandemic. Such advice overwhelmed recommendations for N95 masks that filter out most virus-laden particles suspended in the air. Employers denied many health care workers access to N95s, insisting that only those routinely working within feet of covid patients needed them. More than 3,600 health care workers died in the first year of the pandemic, many due to a lack of protection.
However, a committee advising the CDC appears poised to brush aside the updated science when it comes to its pending guidance on health care facilities.
Lisa Brosseau, an aerosol expert and a consultant at the Center for Infectious Disease Research and Policy in Minnesota, warns of a repeat of 2020 if that happens.
“The rubber hits the road when you make decisions on how to protect people,” Brosseau said. “Aerosol scientists may see this report as a big win because they think everything will now follow from the science. But that’s not how this works and there are still major barriers.”
Money is one. If a respiratory disease spreads through inhalation, it means that people can lower their risk of infection indoors through sometimes costly methods to clean the air, such as mechanical ventilation and using air purifiers, and wearing an N95 mask. The CDC has so far been reluctant to press for such measures, as it updates foundational guidelines on curbing airborne infections in hospitals, nursing homes, prisons, and other facilities that provide health care. This year, a committee advising the CDC released a draft guidance that differs significantly from the WHO report.
Whereas the WHO report doesn’t characterize airborne viruses and bacteria as traveling short distances or long, the CDC draft maintains those traditional categories. It prescribes looser-fitting surgical masks rather than N95s for pathogens that “spread predominantly over short distances.” Surgical masks block far fewer airborne virus particles than N95s, which cost roughly 10 times as much.
Researchers and health care workers have been outraged about the committee’s draft, filing letters and petitions to the CDC. They say it gets the science wrong and endangers health. “A separation between short- and long-range distance is totally artificial,” Tang said.
Airborne viruses travel much like cigarette smoke, he explained. The scent will be strongest beside a smoker, but those farther away will inhale more and more smoke if they remain in the room, especially when there’s no ventilation.
Likewise, people open windows when they burn toast so that smoke dissipates before filling the kitchen and setting off an alarm. “You think viruses stop after 3 feet and drop to the ground?” Tang said of the classical notion of distance. “That is absurd.”
The CDC’s advisory committee is comprised primarily of infection control researchers at large hospital systems, while the WHO consulted a diverse group of scientists looking at many different types of studies. For example, one analysis examined the puff clouds expelled by singers, and musicians playing clarinets, French horns, saxophones, and trumpets. Another reviewed 16 investigations into covid outbreaks at restaurants, a gym, a food processing factory, and other venues, finding that insufficient ventilation probably made them worse than they would otherwise be.
In response to the outcry, the CDC returned the draft to its committee for review, asking it to reconsider its advice. Meetings from an expanded working group have since been held privately. But the National Nurses United union obtained notes of the conversations through a public records request to the agency. The records suggest a push for more lax protection. “It may be difficult as far as compliance is concerned to not have surgical masks as an option,” said one unidentified member, according to notes from the committee’s March 14 discussion. Another warned that “supply and compliance would be difficult.”
The nurses’ union, far from echoing such concerns, wrote on its website, “The Work Group has prioritized employer costs and profits (often under the umbrella of ‘feasibility’ and ‘flexibility’) over robust protections.” Jane Thomason, the union’s lead industrial hygienist, said the meeting records suggest the CDC group is working backward, molding its definitions of airborne transmission to fit the outcome it prefers.
Tang expects resistance to the WHO report. “Infection control people who have built their careers on this will object,” he said. “It takes a long time to change people’s way of thinking.”
The CDC declined to comment on how the WHO’s shift might influence its final policies on infection control in health facilities, which might not be completed this year. Creating policies to protect people from inhaling airborne viruses is complicated by the number of factors that influence how they spread indoors, such as ventilation, temperature, and the size of the space.
Adding to the complexity, policymakers must weigh the toll of various ailments, ranging from covid to colds to tuberculosis, against the burden of protection. And tolls often depend on context, such as whether an outbreak happens in a school or a cancer ward.
“What is the level of mortality that people will accept without precautions?” Tang said. “That’s another question.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
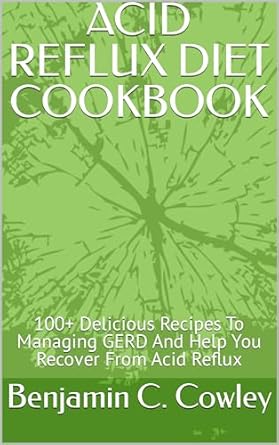
Acid Reflux Diet Cookbook – by Dr. Harmony Reynolds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, this is far more than just a recipe book. Of course, it is common for health-focused recipe books to begin with a preamble about the science that’s going to be applied, but in this case, the science makes up a larger portion of the book than usual, along with practical tips about how to best implement certain things, at home and when out and about.
Dr. Reynolds also gives a lot of information about such things as medications that could be having an effect one way or the other, and even other lifestyle factors such as exercise and so forth, and yes, even stress management. Because for many people, what starts as acid reflux can soon become ulcers, and that’s not good.
The recipes themselves are diverse and fairly simple; they’re written solely with acid reflux in mind and not other health considerations, but they are mostly heathy in the generalized sense too.
The style is straight to the point with zero padding sensationalism, or chit-chat. It can make for a slightly dry read, but let’s face it, nobody is buying this book for its entertainment value.
Bottom line: if you have been troubled by acid reflux, this book will help you to eat your way safely out of it.
Click here to check out the Acid Reflux Diet Cookbook, and enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’m feeling run down. Why am I more likely to get sick? And how can I boost my immune system?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It has been a long winter, filled with many viruses and cost-of-living pressures, on top of the usual mix of work, study, life admin and caring responsibilities.
Stress is an inevitable part of life. In short bursts, our stress response has evolved as a survival mechanism to help us be more alert in fight or flight situations.
But when stress is chronic, it weakens the immune system and makes us more vulnerable to illnesses such as the common cold, flu and COVID.
Pexels/Ketut Subiyanto Stress makes it harder to fight off viruses
When the immune system starts to break down, a virus that would normally have been under control starts to flourish.
Once you begin to feel sick, the stress response rises, making it harder for the immune system to fight off the disease. You may be sick more often and for longer periods of time, without enough immune cells primed and ready to fight.
In the 1990s, American psychology professor Sheldon Cohen and his colleagues conducted a number of studies where healthy people were exposed to an upper respiratory infection, through drops of virus placed directly into their nose.
These participants were then quarantined in a hotel and monitored closely to determine who became ill.
One of the most important factors predicting who got sick was prolonged psychological stress.
Cortisol suppresses immunity
“Short-term stress” is stress that lasts for a period of minutes to hours, while “chronic stress” persists for several hours per day for weeks or months.
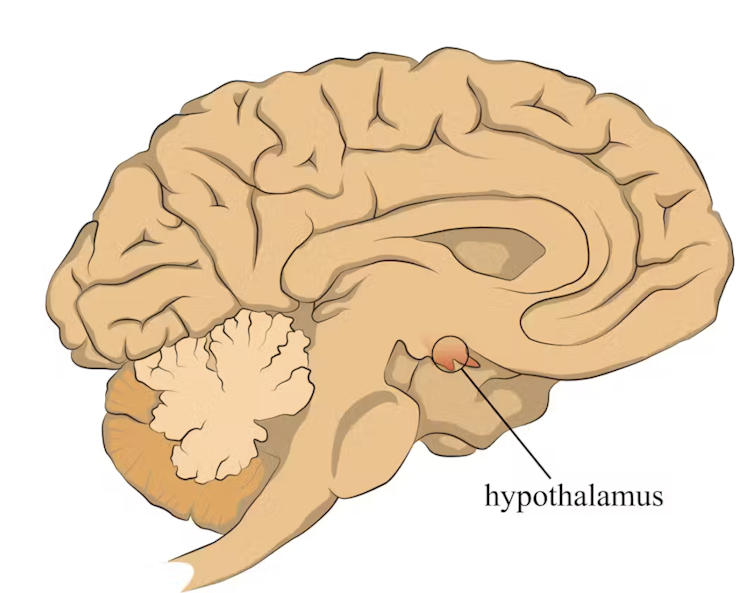
When faced with a perceived threat, psychological or physical, the hypothalamus region of the brain sets off an alarm system. This signals the release of a surge of hormones, including adrenaline and cortisol.
The hypothalamus sets off an alarm system in response to a real or perceived threat. stefan3andrei/Shutterstock In a typical stress response, cortisol levels quickly increase when stress occurs, and then rapidly drop back to normal once the stress has subsided. In the short term, cortisol suppresses inflammation, to ensure the body has enough energy available to respond to an immediate threat.
But in the longer term, chronic stress can be harmful. A Harvard University study from 2022 showed that people suffering from psychological distress in the lead up to their COVID infection had a greater chance of experiencing long COVID. They classified this distress as depression, probable anxiety, perceived stress, worry about COVID and loneliness.
Those suffering distress had close to a 50% greater risk of long COVID compared to other participants. Cortisol has been shown to be high in the most severe cases of COVID.
Stress causes inflammation
Inflammation is a short-term reaction to an injury or infection. It is responsible for trafficking immune cells in your body so the right cells are present in the right locations at the right times and at the right levels.
The immune cells also store a memory of that threat to respond faster and more effectively the next time.
Initially, circulating immune cells detect and flock to the site of infection. Messenger proteins, known as pro-inflammatory cytokines, are released by immune cells, to signal the danger and recruit help, and our immune system responds to neutralise the threat.
During this response to the infection, if the immune system produces too much of these inflammatory chemicals, it can trigger symptoms such as nasal congestion and runny nose.
Our immune response can trigger symptoms such as a runny nose. Alyona Mandrik/Shutterstock What about chronic stress?
Chronic stress causes persistently high cortisol secretion, which remains high even in the absence of an immediate stressor.
The immune system becomes desensitised and unresponsive to this cortisol suppression, increasing low-grade “silent” inflammation and the production of pro-inflammatory cytokines (the messenger proteins).
Immune cells become exhausted and start to malfunction. The body loses the ability to turn down the inflammatory response.
Over time, the immune system changes the way it responds by reprogramming to a “low surveillance mode”. The immune system misses early opportunities to destroy threats, and the process of recovery can take longer.
So how can you manage your stress?
We can actively strengthen our immunity and natural defences by managing our stress levels. Rather than letting stress build up, try to address it early and frequently by:
1) Getting enough sleep
Getting enough sleep reduces cortisol levels and inflammation. During sleep, the immune system releases cytokines, which help fight infections and inflammation.
2) Taking regular exercise
Exercising helps the lymphatic system (which balances bodily fluids as part of the immune system) circulate and allows immune cells to monitor for threats, while sweating flushes toxins. Physical activity also lowers stress hormone levels through the release of positive brain signals.
3) Eating a healthy diet
Ensuring your diet contains enough nutrients – such as the B vitamins, and the full breadth of minerals like magnesium, iron and zinc – during times of stress has a positive impact on overall stress levels. Staying hydrated helps the body to flush out toxins.
4) Socialising and practising meditation or mindfulness
These activities increase endorphins and serotonin, which improve mood and have anti-inflammatory effects. Breathing exercises and meditation stimulate the parasympathetic nervous system, which calms down our stress responses so we can “reset” and reduce cortisol levels.
Sathana Dushyanthen, Academic Specialist & Lecturer in Cancer Sciences & Digital Health| Superstar of STEM| Science Communicator, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: