Cure – by Dr. Jo Marchant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The subtitle here, “a journey into the science of mind over body”, prompts an immediate question: is this book actually about science?
And yes, yes it is. It’s not about “positive energy” or “tapping into your divine essence” or anysuch. It’s about science, and scientific studies.
The author’s PhD is in genetics and medical microbiology, not metaphysics or something.
For those of us who read a lot of clinical studies about a lot of things (hi, regular researcher/writer here), we’re very used to placebo being used as a control in medical science.
“This drug performed no better than placebo” is generally considered a disappointing statement… But what if the placebo was already having a profound effect? Shouldn’t that be worthy of note too?
Dr. Marchant looks at more than just drugs, though, and also looks into the science (complete with EEGs and such) of hypnosis and virtual reality.
The writing style here is very accessible without skimping on science. This is to be expected; Dr. Marchant also has an MSc in science communication, and spent a time as senior editor of New Scientist magazine.
This isn’t a how-to book, but there are some practical takeaways too, specific things we can do to augment (or avoid sabotaging) any medications we take, for example.
Bottom line: placebo effect (and its evil twin, the nocebo effect) has a profound impact on all of us whether we want it or not, so we might as well learn about how it works and how to leverage it. This book gives a very good, hard science grounding.
Click here to check out “Cure” and get the most out of whatever you take (or do) for your health!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Should Diversify Your Nuts!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Time to go nuts for nuts!
Nuts, in popular perception, range from “basically the healthiest food anyone can eat” to “basically high calorie salty snacks”. And, they can be either!
Some notes, then:
- Raw is generally better that not
- Dry roasted is generally better than the kind with added oils
- Added salt is neither necessary nor good
Quick tip: if “roasted salted” are the cheapest or most convenient to buy, you can at least mitigate that by soaking them in warm water for 5 minutes, before rinsing and (if you don’t want wet nuts) drying.
You may be wondering: who does want wet nuts? And the answer is, if for example you’re making a delicious cashew and chickpea balti, the fact you didn’t dry them before throwing them in won’t make a difference.
Now, let’s do a quick run-down; we don’t usually do “listicles” but it seemed a good format here, so we’ve picked a top 5 for nutritional potency:
Almonds
We may have a bias. We accept it. But almonds are also one of the healthiest nuts around, and generally considered by most popular metrics the healthiest.
Not only are they high in protein, healthy fat, fiber, vitamins, and minerals, but they’re even a natural prebiotic that increases the populations of healthy gut bacteria, while simultaneously keeping down the populations of gut pathogens—what more can we ask of a nut?
Read more: Prebiotic effects of almonds and almond skins on intestinal microbiota in healthy adult humans
Pistachios
Not only are these super tasty and fun to eat (and mindful eating is all but guaranteed, as shelling them by hand slows us down and makes us more likely to eat them one at a time rather than by the handful), but also they contain lots of nutrients and are lower in calories than most nuts, so they’re a great option for anyone who’d like to eat more nuts but is doing a calorie-controlled diet and doesn’t want to have half a day’s calories in a tiny dish of nuts.
Walnuts
Popularly associated with brain health (perhaps easy to remember because of their appearance), they really are good for the brain:
Check it out: Beneficial Effects of Walnuts on Cognition and Brain Health
Cashews
A personal favorite of this writer for their versatility in cooking, food prep, or just as a snack, they also do wonders for metabolic health:
Brazil nuts
The most exciting thing about these nuts is that they’re an incredibly potent source of selenium, which is important not just for hair/skin/nails as popularly marketed, but also for thyroid hormone production and DNA synthesis.
But don’t eat too many, because selenium is definitely one of those “you can have too much of a good thing” nutrients, and selenium poisoning can make your hair (however beautiful and shiny it got because of the selenium) fall out if you take too much.
Know the numbers: Brazil nuts and selenium—health benefits and risks
Bottom line on nuts:
- Nuts are a great and healthful part of almost anyone’s diet
- Obviously, if you have a nut allergy, then we’re sorry; this one won’t have helped you so much
- Almonds are one of the most healthful nuts out there
- Brazil nuts are incredibly potent, to the point where moderation is recommended
- A handful of mixed nuts per day is a very respectable option—when it comes to food and health, diversity is almost always good!
Share This Post
-
Acid Reflux After Meals? Here’s How To Stop It Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Harvard-trained gastroenterologist Dr. Saurabh Sethi advises:
Calming it down
First of all, what it actually is and how it happens: acid reflux occurs when the lower esophageal sphincter (LES) doesn’t close properly, allowing stomach acid to flow back into the esophagus. Chronic acid reflux is known as gastroesophageal reflux disease (GERD). Symptoms can include heartburn, an acid taste in the mouth, belching, bloating, sore throat, and a persistent cough—but most people do not get all of the symptoms, usually just some.
Things that help it acutely (as in, you can do them today and they will help today): consider skipping certain foods/substances like peppermint, tomatoes, chocolate, alcohol, and caffeine, which can worsen acid reflux. Eating smaller, more frequent meals instead of large ones and leaving a gap of 3–4 hours before lying down after meals can also help manage symptoms.
Things that can help it chronically (as in, you do them in an ongoing fashion and they will help in an ongoing fashion): lifestyle changes like quitting smoking, reducing alcohol intake, and wearing loose clothing can strengthen the LES. Maintaining a healthy weight and avoiding large meals, especially close to bedtime, can also reduce symptoms. Elevating the upper body while sleeping (using a wedge pillow or raising the bed by 10–20°) can make a big difference.
Medications to avoid, if possible, include: aspirin, ibuprofen, and calcium channel blockers.
Some drinks you can enjoy that will help: drinking water can quickly dilute stomach acid and provide relief. Herbal teas like basil tea, fennel tea, and ginger tea are also effective. But notably: not peppermint tea! Since, as mentioned earlier, peppermint is a known trigger for acid reflux (despite peppermint’s usual digestion-improving properties).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Coughing/Wheezing After Dinner? Here’s How To Fix It ← this is about acid reflux and more
Take care!
Share This Post
-
Spiked Acupressure Mat: Trial & Report
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are you ready for the least comfortable bed? The reviews are in, and…
Let’s get straight to the point
“Laura Try” tries out health things and reports on her findings. And in this case…
- She noted up front that the claims for this are to improve relaxation, alleviate muscle pain, and improve sleep.
- It also is said to help with myofascial release specifically, which can improve flexibility and mobility (as well as contributing to the alleviation of muscle pain previously mentioned)
- She did not enjoy it at first! Shocking nobody, it was uncomfortable and even somewhat painful. However, after a while, it became less painful and more comfortable—except for trying standing on it, which still hurt (this writer has one too, and I often stand on it at my desk, whenever I feel my feet need a little excitement—it’s probably good for the circulation, but that is just a hypothesis)
- Soon, it became relaxing. Writer’s note: that raised hemicylindrical pillow she’s using? Try putting it under your neck instead, to stimulate the vagus nerve.
- While it is best use on bare skin, the effect can be softened by wearing a thin later of clothing between you and the mat.
- She got hers for £71 GBP (this writer got hers for a fraction of that price from Aldi—and here’s an example product on Amazon, at a more mid-range price)
For more details on all of the above and a blow-by-blow account, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fascia: Why (And How) You Should Take Care Of Yours
Take care!
Share This Post
Related Posts
-
Winter Wellness – by Rachel de Thample
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Winter is often the season of comfort foods and, in much of the Western world, there’s a holiday season slide of forgotten diets and instead sugar, alcohol, pastry, and the like.
What de Thample does here is an antidote to all that, without sacrificing happiness and celebration.
Before the recipes get started, she has a chapter on “food as medicine“, and to our immense surprise, proceeds to detail, accurately, many categories such as
- Foods for immune health
- Foods against inflammation
- Foods for gut health
- Foods against aging
- Foods for energy levels
- Foods against anxiety
- Foods for hormonal balance
…and so forth, with lists of ingredients that fit into each category.
Then in the rest of the book, she lays out beautiful recipes for wonderful dishes (and drinks) that use those ingredients, without unhealthy additions.
The recipes are, by the way, what could best be categorized as “fancy”. However, they are fancy in the sense that they will be impressive for entertaining, and (again, to our great surprise) they don’t actually call for particularly expensive/rare ingredients, nor for arcane methods and special equipment.Instead, everything’s astonishingly accessible to put together and easy to execute.
Bottom line: if you’d like to indulge this winter, but would like to do so healthily, this is an excellent way to do so.
Click here to check out Winter Wellness, and level-up your seasonal health and happiness!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
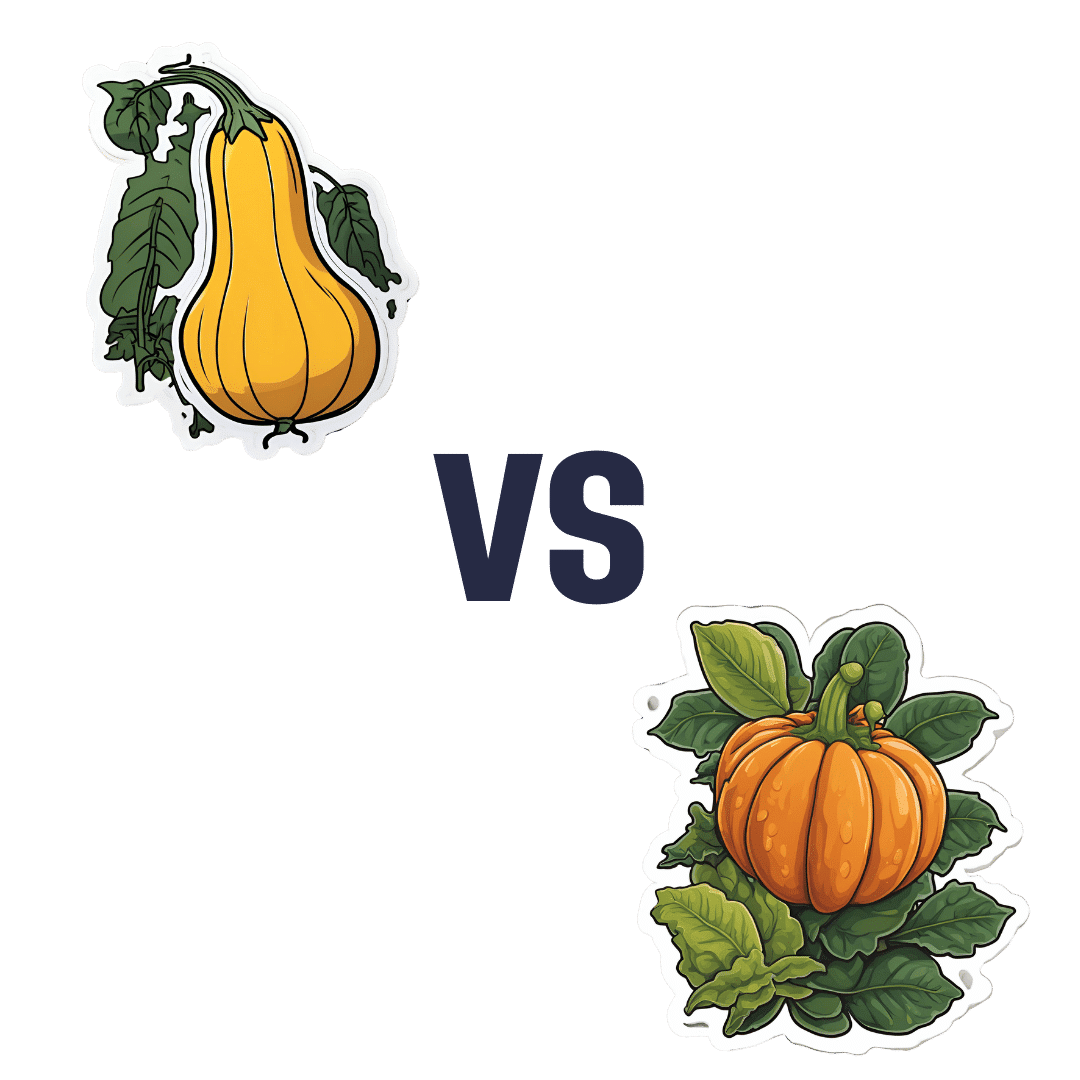
Butternut Squash vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing butternut squash to pumpkin, we picked the butternut squash.
Why?
Both are great! But the butternut squash manages a moderate win in most categories.
In terms of macros, butternut squash has more of everything except water. Most notably, it has more protein and more fiber. Yes, more carbs too, but the fiber content means that it also has the lower glycemic index, by quite a bit.
When it comes to vitamins, pumpkin does have a little more of vitamin B1 and a lot more of vitamin E, while butternut squash has more of vitamins B3, B5, B9, C, K, and choline. They’re about equal in the other vitamins they both contain. A fair win for butternut squash.
In the category of minerals, butternut squash has more calcium, magnesium, manganese, and selenium, while pumpkin has more copper, iron, and phosphorus. They’re about equal in potassium and zinc. A marginal win for butternut squash.
Adding up the strong win, the fair win, and the marginal win, makes for an easy overall win for butternut squash!
Want to learn more?
You might like to read:
Superfood-Stuffed Squash Recipe
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Genius Foods – by Max Lugavere
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There is a lot of seemingly conflicting (or sometimes: actually conflicting!) information out there with regard to nutrition and various aspects of health. Why, for example, are we told:
- Be sure to get plenty of good healthy fats from nuts and seeds, for metabolic health and brain health too!
- But these terrible nut and seed oils lead to heart disease and dementia! Avoid them at all costs!
Max Lugavere demystifies this and more.
His science-led approach is primarily focused on avoiding dementia, and/but is at least not bad when it comes to other areas of health too.
He takes us on a tour of different parts of our nutrition, including:
- Perhaps the clearest explanation of “healthy” vs “unhealthy” fats this reviewer has read
- Managing carbs (simple and complex) for healthy glucose management—essential for good brain health
- What foods to improve or reduce—a lot you might guess, but this is a comprehensive guide to brain health so it’d be remiss to skip it
- The role that intermittent fasting can play as a bonus extra
While the main thrust of the book is about avoiding cognitive impairment in the long-term (including later-life dementia), he makes good, evidence-based arguments for how this same dietary plan improves cognitive function in the short-term, too.
Speaking of that dietary plan: he does give a step-by-step guide in a “make this change first, then this, then this” fashion, and offers some sample recipes too. This is by no means a recipe book though—most of the book is taking us through the science, not the kitchen.
Bottom line: this is the book for getting unconfused with regard to diet and brain health, making a lot of good science easy to understand. Which we love!
Click here to check out “Genius Foods” on Amazon today, give your brain a boost!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: