Widen the Window – by Dr. Elizabeth Stanley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, about the title… That “window” that the author bids us “widen” is not a flowery metaphor, but rather, is referring to the window of exhibited resilience to stress/trauma; the “window” in question looks like an “inverted U” bell-curve on the graph.
In other words: Dr. Stanley’s main premise here is that we respond best to moderate stress (i.e: in that window, the area under the curve!), but if there is too little or too much, we don’t do so well. The key, she argues, is widening that middle part (expanding the area under the curve) in which we perform optimally. That way, we can still function in a motivated fashion without extrinsic threats, and we also don’t collapse under the weight of overwhelm, either.
The main strength of this book, however, lies in its practical exercises to accomplish that—and more.
“And more”, because the subtitle also promised recovery from trauma, and the author delivers in that regard too. In this case, it’s about widening that same window, but this time to allow one’s parasympathetic nervous system to recognize that the traumatic event is behind us, and no longer a threat; we are safe now.
Bottom line: if you would like to respond better to stress, and/or recover from trauma, this book is a very good tool.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
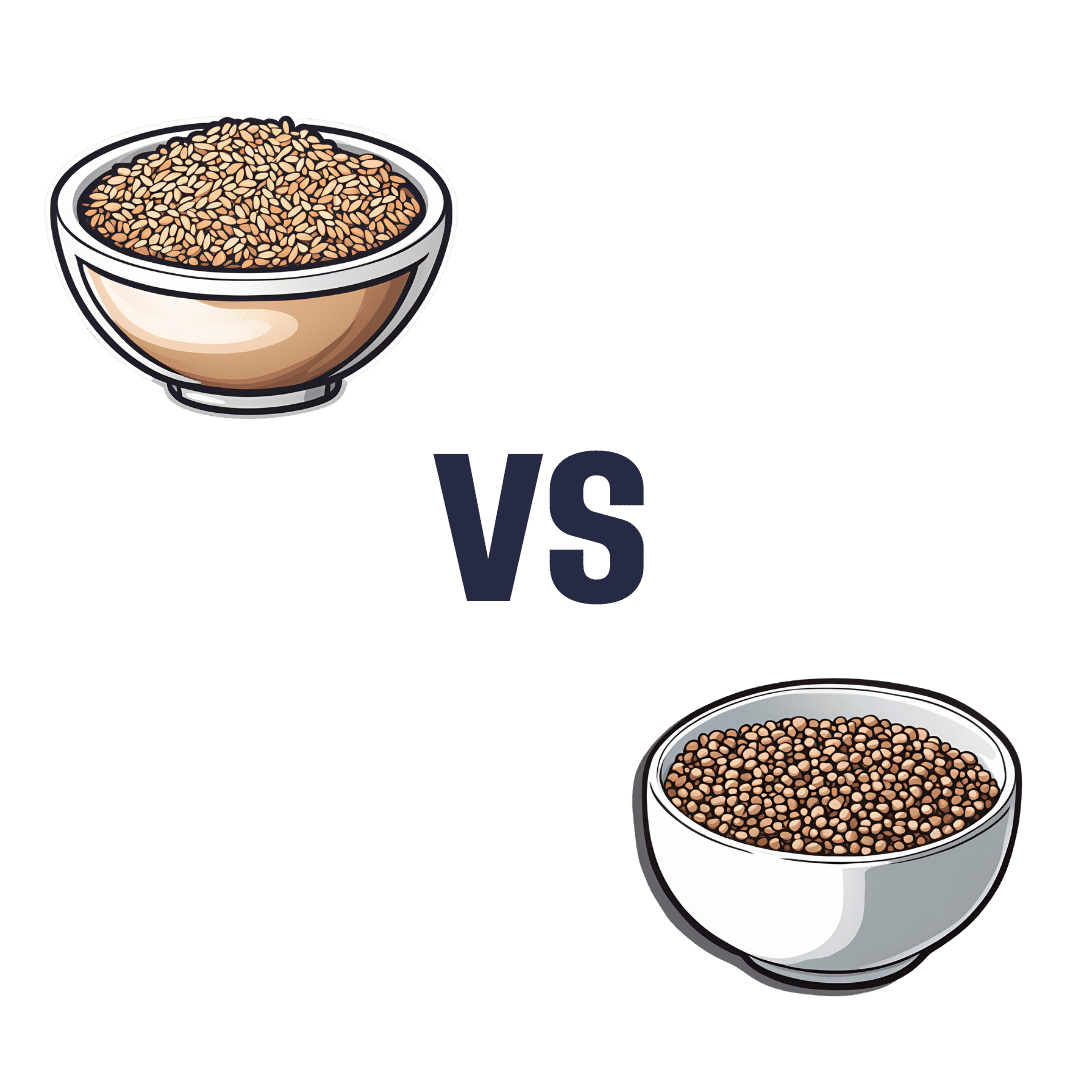
Brown Rice vs Buckwheat – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing brown rice to buckwheat, we picked the buckwheat.
Why?
In terms of macros, brown rice has more carbs, while buckwheat has nearly 2x the fiber, and more protein. An easy choice here: buckwheat for the win.
In the category of vitamins, brown rice has more of vitamins B1, B2, B3, B6, and E, while buckwheat has more of vitamins B9, K, and choline. A win for brown rice this time, although as a point in buckwheat’s favor, while most of the margins of difference are comparable, buckwheat has nearly 10x the vitamin K.
When it comes to minerals, brown rice has more manganese, phosphorus, selenium, and zinc, while buckwheat has more calcium, copper, iron, and magnesium. A win for buckwheat again this time.
A quick note on gluten: both of these are naturally gluten-free, so that’s not an issue here. Buckwheat, despite its name, is not a wheat, nor even closely related to wheat. It’s not even technically a grain; it’s a flowering plant of which we eat the groats. In taxonomic terms, buckwheat is about as related to wheat as a lionfish is to a lion.
Adding up the sections makes for an overall 2:1 win for buckwheat, though even if it weren’t for that, which is someone more likely to hear from a doctor, “you need to eat more fiber”, or “you need to eat more vitamin E”? Thus, even had the categories been tied (let’s imagine it had been tied on minerals, say) that’d have been a tiebreaker in favor of buckwheat. As it is, buckwheat already won by strength of numbers anyway.
Of course, do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Grains: Bread Of Life, Or Cereal Killer?
Enjoy!
Share This Post
-
How Aging Changes At 44 And Again At 60 (And What To Do About It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As it turns out, aging is not linear. Or rather: chronological aging may be, but biological aging isn’t, and there are parts of our life where it kicks into a different gear. This study looked at 108 people (65 of whom women) between the ages of 25 and 75, as part of a longitudinal cohort study, tracked for around 2–8 years (imprecise as not all follow-up durations were the same). They took frequent blood and urine samples, and tested them for thousands of different molecules and analyzing changes in gene expression, proteomic, blood biomarkers, and more. All things that are indicators of various kinds of health/disease, and which might seem more simple but it isn’t: aging.
Here’s what they found:
Landmark waypoints
At 44, significant changes occur in the metabolism, including notably the metabolism of carbs, caffeine, and alcohol. A large portion of this may be hormone related, as that’s a time of change not just for those undergoing the menopause, but also the andropause (not entirely analogous to the menopause, but it does usually entail a significant reduction in sex hormone production; in this case, testosterone).
However, the study authors also hypothesize that lifestyle factors may be relevant, as one’s 40s are often a stressful time, and an increase in alcohol consumption often occurs around the same time as one’s ability to metabolize it drops, resulting in further dysfunctional alcohol metabolism.
At 60, carb metabolism slows again, with big changes in glucose metabolism specifically, as well as an increased risk of cardiovascular disease, and a decline in kidney function. In case that wasn’t enough: also an increase free radical pathology, meaning a greatly increased risk of cancer. Immune function drops too.
What to do about this: the recommendation is of course to be proactive, and look after various aspects of your health before it becomes readily apparent that you need to. For example, good advice for anyone approaching 44 might be to quit alcohol, go easy on caffeine, and eat a diet that is conducive to good glucose metabolism. Similarly, good advice for anyone approaching 60 might be to do the same, and also pay close attention to keeping your kidneys healthy. Getting regular tests done is also key, including optional extras that your doctor might not suggest but you should ask for, such as blood urea nitrogen levels (biomarkers of kidney function). The more we look after each part of our body, the more they can look after us in turn, and the fewer/smaller problems we’ll have down the line.
If you, dear reader, are approaching the age 44 or 60… Be neither despondent nor complacent. We must avoid falling into the dual traps of “Well, that’s it, bad health is around the corner, nothing I can do about it; that’s nature”, vs “I’ll be fine, statistics are for other people, and don’t apply to me”.
Those are averages, and we do not have to be average. Every population has statistical outliers. But it would be hubris to think none of this will apply to us and we can just carry on regardless. So, for those of us who are approaching one of those two ages… It’s time to saddle up, knuckle down, and do our best!
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Also, if you’d like to read the actual paper by Dr. Xiaotao Shen et al., here it is:
Nonlinear dynamics of multi-omics profiles during human aging ← honestly, it’s a lot clearer and more informative than the video, and also obviously discusses things in a lot more detail than we have room to here
Take care!
Share This Post
-
SuperLife – by Darin Olien
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We mostly know more or less what we’re supposed to be doing, at least to a basic level, when it comes to diet and exercise. So why don’t we do it?
Where Darin Olien excels in this one is making healthy living—mostly the dietary aspects thereof—not just simple, but also easy.
He gives principles we can apply rather than having to memorize lots of information… And his “this will generally be better than that” format also means that the feeling is one of reducing harm, increasing benefits, without needing to get absolutist about anything. And that, too, makes healthy living easier.
The book also covers some areas that a lot of books of this genre don’t—such as blood oxygenation, and maintenance of healthy pH levels—and aspects such as those are elements that help this book to stand out too.
Don’t be put off and think this is a dry science textbook, though—it’s not. In fact, the tone is light and the style is easy-reading throughout.
Bottom line: if you want to take an easy, casual, but scientifically robust approach to tweaking your health for the better, this book will enable you to do that.
Click here to check out SuperLife and start upgrading your health!
Share This Post
Related Posts
-
Knit for Health & Wellness – by Betsan Corkhill
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Betsan Corkhill, a physiotherapist, has more than just physiotherapy in mind when it comes to the therapeutic potential of knitting (although yes, also physiotherapy!), and much of this book is about the more psychological benefits that go way beyond “it’s a relaxing pastime”.
She makes the case for how knitting (much like good mental health) requires planning, action, organization, persistence, focus, problem-solving, and flexibility—and thus the hobby develops and maintains all the appropriate faculties for those things, which will then be things you get to keep in the rest of your life, too.
Fun fact: knitting, along with other similar needlecrafts, was the forerunner technology for modern computer programming! And indeed, early computers, the kind with hole-punch data streams, used very similar pattern-storing methods to knitting patterns.
So, for something often thought of as a fairly mindless activity for those not in the know, knitting has a lot to offer for what’s between your ears, as well as potentially something for keeping your ears warm later.
One thing this book’s not, by the way: a “how to” guide for learning to knit. It assumes you either have that knowledge already, or will gain it elsewhere (there are many tutorials online).
Bottom line: if you’re in the market for a new hobby that’s good for your brain, this book will give you great motivation to give knitting a go!
Click here to check out Knit For Health & Wellness, and get knitting!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Milk Thistle For The Brain, Bones, & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Thistle Do Nicely”
Milk thistle is a popular supplement; it comes from the milk thistle plant (Silybum marianum), commonly just called thistles. There are other kinds of thistle too, but these are one of the most common.
So, what does it do?
Liver health
Milk thistle enjoys popular use to support liver health; the liver is a remarkably self-regenerative organ if given the chance, but sometimes it can use a helping hand.
See for example: How To Undo Liver Damage
As for milk thistle’s beneficence, it is very well established:
- Milk thistle in liver diseases: past, present, future
- Hepatoprotective effect of silymarin
- Silybum Marianum and Chronic Liver Disease: A Marriage of Many Years
Brain health
For this one the science is less well-established, as studies so far have been on non-human animals, or have been in vitro studies.
Nevertheless, the results so far are promising, and the mechanism of action seems to be a combination of reducing oxidative stress and neuroinflammation, as well as suppressing amyloid β-protein (Aβ) fibril formation, in other words, reducing amyloid plaques.
General overview: A Mini Review on the Chemistry and Neuroprotective Effects of Silymarin
All about the plaques, but these are non-human animal studies:
- Mouse model: Silymarin attenuated the amyloid β plaque burden and improved behavioral abnormalities in an Alzheimer’s disease mouse model
- Rat model: Silymarin effect on amyloid-β plaque accumulation and gene expression of APP in an Alzheimer’s disease rat model
Against diabetes
Milk thistle improves insulin sensitivity, and reduces fasting blood sugar levels and HbA1c levels. The research so far is mostly in type 2 diabetes, however (at least, so far as we could find). For example:
Studies we could find for T1D were very far from translatable to human usefulness, for example, “we poisoned these rats with streptozotocin then gave them megadoses of silymarin (10–15 times the dose usually recommended for humans) and found very small benefits to the lenses of their eyes” (source).
Against osteoporosis
In this case, milk thistle’s estrogenic effects may be of merit to those at risk of menopause-induced osteoporosis:
If you’d like a quick primer about such things as what antiosteoclastic activity is, here’s a quick recap:
Which Osteoporosis Medication, If Any, Is Right For You?
Is it safe?
It is “Generally Recognized As Safe”, and even when taken at high doses for long periods, side effects are very rare.
Contraindications include if you’re pregnant, nursing, or allergic.
Potential reasons for caution (but not necessarily contraindication) include if you’re diabetic (its blood-sugar lowering effects will decrease the risk of hyperglycemia while increasing the risk of hypoglycemia), or have a condition that could be exacerbated by its estrogenic effects—including if you are on HRT, because it’s an estrogen receptor agonist in some ways (for example those bone benefits we mentioned before) but an estrogen antagonist in others (for example, in the uterus, if you have one, or in nearby flat muscles, if you don’t).
As ever, speak with your doctor/pharmacist to be sure.
Want to try it?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women’s Strength Training Anatomy – by Frédéric Delavier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fitness guides for women tend to differ from fitness guides for men, in the wrong ways:
“Do some squats and jumping jacks, and here’s a exercise for your abs; you too can look like our model here”
In those other books we are left wonder: where’s the underlying information? Where are the explanations that aren’t condescending? Where, dare we ask, is the understanding that a woman might ever lift something heavier than a baby?
Delavier, in contrast, delivers. With 130 pages of detailed anatomical diagrams for all kinds of exercises to genuinely craft your body the way you want it for you. Bigger here, smaller there, functional strength, you decide.
And rest assured: no, you won’t end up looking like Arnold Schwarzenegger unless you not only eat like him, but also have his genes (and possibly his, uh, “supplement” regime).
What you will get though, is a deep understanding of how to tailor your exercise routine to actually deliver the personalized and specific results that you want.
Pick Up Today’s Book on Amazon!
Not looking for a feminine figure? You may like the same author’s book for men:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: