What Too Much Exercise Does To Your Body And Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Get more exercise” is a common rallying-cry for good health, but it is possible to overdo it. And, this is not just a matter of extreme cases of “exercise addiction”, but even going much above certain limits can already result in sabotaging one’s healthy gains. But how, and where does the line get drawn?
Too Much Of A Good Thing
The famous 150 minutes per week of moderate exercise (or 75 minutes of intense exercise) is an oft-touted figure. This video, on the other hand, springs for 5 hours of moderate exercise or 2.5 hours intense exercise as a good guideline.
We’re advised that going over those guidelines doesn’t necessarily increase health benefits, and on the contrary, may reduce or even reverse them. For example, we are told…
- Light to moderate running reduces the risk of death, but running intensely more than 3 times a week can negate these benefits.
- Extreme endurance exercises, like ultra-marathons, may cause heart damage, heart rhythm disorders, and artery enlargement.
- Women who exercise strenuously every day have a higher risk of heart attacks and strokes compared to those who exercise moderately.
- Excessive exercise in women can lead to the “female athlete triad” (loss of menstruation, osteoporosis, and eating disorders).
- In men, intense exercise can lower libido due to fatigue and reduced testosterone levels.
- Both men and women are at increased risk of overuse injuries (e.g., tendinitis, stress fractures) and impaired immunity from excessive exercise.
- There is a 72-hour window of impaired immunity after intense exercise, increasing the risk of infections.
Exercise addiction is rare, though, with this video citing “around 1 million people in the US suffer from exercise addiction”.
For more on finding the right balance, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cardiac Failure Explained – by Dr. Warrick Bishop
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The cover of this book makes it look like it’ll be a flashy semi-celebrity doctor keen to sell his personalized protocol, along with eleventy-three other books, but actually, what’s inside this one is very different:
We (hopefully) all know the basics of heart health, but this book takes it a lot further. Starting with the basics, then the things that it’s easy to feel like you should know but actually most people don’t, then into much more depth.
The format is much more like a university textbook than most pop-science books, and everything about the way it’s written is geared for maximum learning. The one thing it does keep in common with pop-science books as a genre is heavy use of anecdotes to illustrate points—but he’s just as likely to use tables, diagrams, callout boxes, emboldening of key points, recap sections, and so forth. And for the most part, this book is very information-dense.
Dr. Bishop also doesn’t just stick to what’s average, and talks a lot about aberrations from the norm, what they mean and what they do and yes, what to do about them.
On the one hand, it’s more information dense than the average reader can reasonably expect to need… On the other hand, isn’t it great to finish reading a book feeling like you just did a semester at medical school? No longer will you be baffled by what is going on in your (or perhaps a loved one’s) cardiac health.
Bottom line: if you’d like to know cardiac health inside out, this book is an excellent place to start.
Click here to check out Cardiac Failure Explained, and get to the heart of things!
Share This Post
-
Exercise, therapy and diet can all improve life during cancer treatment and boost survival. Here’s how
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With so many high-profile people diagnosed with cancer we are confronted with the stark reality the disease can strike any of us at any time. There are also reports certain cancers are increasing among younger people in their 30s and 40s.
On the positive side, medical treatments for cancer are advancing very rapidly. Survival rates are improving greatly and some cancers are now being managed more as long-term chronic diseases rather than illnesses that will rapidly claim a patient’s life.
The mainstays of cancer treatment remain surgery, chemotherapy, radiation therapy, immunotherapy, targeted therapy and hormone therapy. But there are other treatments and strategies – “adjunct” or supportive cancer care – that can have a powerful impact on a patient’s quality of life, survival and experience during cancer treatment.
PeopleImages.com – Yuri A/Shutterstock Keep moving if you can
Physical exercise is now recognised as a medicine. It can be tailored to the patient and their health issues to stimulate the body and build an internal environment where cancer is less likely to flourish. It does this in a number of ways.
Exercise provides a strong stimulus to our immune system, increasing the number of cancer-fighting immune cells in our blood circulation and infusing these into the tumour tissue to identify and kill cancer cells.
Our skeletal muscles (those attached to bone for movement) release signalling molecules called myokines. The larger the muscle mass, the more myokines are released – even when a person is at rest. However, during and immediately after bouts of exercise, a further surge of myokines is secreted into the bloodstream. Myokines attach to immune cells, stimulating them to be better “hunter-killers”. Myokines also signal directly to cancer cells slowing their growth and causing cell death.
Exercise can also greatly reduce the side effects of cancer treatment such as fatigue, muscle and bone loss, and fat gain. And it reduces the risk of developing other chronic diseases such as heart disease and type 2 diabetes. Exercise can maintain or improve quality of life and mental health for patients with cancer.
Emerging research evidence indicates exercise might increase the effectiveness of mainstream treatments such as chemotherapy and radiation therapy. Exercise is certainly essential for preparing the patient for any surgery to increase cardio-respiratory fitness, reduce systemic inflammation, and increase muscle mass, strength and physical function, and then rehabilitating them after surgery.
These mechanisms explain why cancer patients who are physically active have much better survival outcomes with the relative risk of death from cancer reduced by as much as 40–50%.
Mental health helps
The second “tool” which has a major role in cancer management is psycho-oncology. It involves the psychological, social, behavioural and emotional aspects of cancer for not only the patient but also their carers and family. The aim is to maintain or improve quality of life and mental health aspects such as emotional distress, anxiety, depression, sexual health, coping strategies, personal identity and relationships.
Supporting quality of life and happiness is important on their own, but these barometers can also impact a patient’s physical health, response to exercise medicine, resilience to disease and to treatments.
If a patient is highly distressed or anxious, their body can enter a flight or fight response. This creates an internal environment that is actually supportive of cancer progression through hormonal and inflammatory mechanisms. So it’s essential their mental health is supported.
Chemotherapy can be stressful on the body and emotional reserves. Shutterstock Putting the good things in: diet
A third therapy in the supportive cancer care toolbox is diet. A healthy diet can support the body to fight cancer and help it tolerate and recover from medical or surgical treatments.
Inflammation provides a more fertile environment for cancer cells. If a patient is overweight with excessive fat tissue then a diet to reduce fat which is also anti-inflammatory can be very helpful. This generally means avoiding processed foods and eating predominantly fresh food, locally sourced and mostly plant based.
Some cancer treatments cause muscle loss. Avoiding processed foods may help. Shutterstock Muscle loss is a side effect of all cancer treatments. Resistance training exercise can help but people may need protein supplements or diet changes to make sure they get enough protein to build muscle. Older age and cancer treatments may reduce both the intake of protein and compromise absorption so supplementation may be indicated.
Depending on the cancer and treatment, some patients may require highly specialised diet therapy. Some cancers such as pancreatic, stomach, esophageal, and lung cancer can cause rapid and uncontrolled drops in body weight. This is called cachexia and needs careful management.
Other cancers and treatments such as hormone therapy can cause rapid weight gain. This also needs careful monitoring and guidance so that, when a patient is clear of cancer, they are not left with higher risks of other health problems such as cardiovascular disease and metabolic syndrome (a cluster of conditions that boost your risk of heart disease, stroke and type 2 diabetes).
Working as a team
These are three of the most powerful tools in the supportive care toolbox for people with cancer. None of them are “cures” for cancer, alone or together. But they can work in tandem with medical treatments to greatly improve outcomes for patients.
If you or someone you care about has cancer, national and state cancer councils and cancer-specific organisations can provide support.
For exercise medicine support it is best to consult with an accredited exercise physiologist, for diet therapy an accredited practising dietitian and mental health support with a registered psychologist. Some of these services are supported through Medicare on referral from a general practitioner.
For free and confidential cancer support call the Cancer Council on 13 11 20.
Rob Newton, Professor of Exercise Medicine, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Biological Mind – by Dr. Alan Jasanoff
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How special is our brain? According to Dr. Alan Jasanoff, it’s not nearly as special as we think it is.
In this work, he outlines the case for how we have collectively overstated the brain’s importance. That it’s just another organ like a heart or a kidney, and that who we are is as much a matter of other factors, as what goes on in our brain.
In this reviewer’s opinion, he overcorrects a bit. The heart and kidneys are very simple organs, as organs go. The brain is not. And while everything from our gut microbiota to our environment to our hormones may indeed contribute to what is us, our brain is one thing that can’t just be swapped out.
Nevertheless, this very well-written book can teach us a lot about everything else that makes us us, including many biological factors that many people don’t know about or consider.
Towards the end of the book, he switches into futurist speculation, and his speculation can be summed up as “we cannot achieve anything worthwhile in the future”.
Bottom line: if you’ve an interest in such things as how transplanting glial cells can give a 30% cognitive enhancement, and how a brain transplant wouldn’t result in the same us in a different body, this is the book for you.
Click here to check out The Biological Mind, and learn about yours!
Share This Post
Related Posts
-
Bird flu has been detected in a pig in the US. Why does that matter?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States Department of Agriculture last week reported that a pig on a backyard farm in Oregon was infected with bird flu.
As the bird flu situation has evolved, we’ve heard about the A/H5N1 strain of the virus infecting a range of animals, including a variety of birds, wild animals and dairy cattle.
Fortunately, we haven’t seen any sustained spread between humans at this stage. But the detection of the virus in a pig marks a worrying development in the trajectory of this virus.
David MG/Shutterstock How did we get here?
The most concerning type of bird flu currently circulating is clade 2.3.4.4b of A/H5N1, a strain of influenza A.
Since 2020, A/H5N1 2.3.4.4b has spread to a vast range of birds, wild animals and farm animals that have never been infected with bird flu before.
While Europe is a hotspot for A/H5N1, attention is currently focused on the US. Dairy cattle were infected for the first time in 2024, with more than 400 herds affected across at least 14 US states.
Bird flu has enormous impacts on farming and commercial food production, because infected poultry flocks have to be culled, and infected cows can result in contaminated diary products. That said, pasteurisation should make milk safe to drink.
While farmers have suffered major losses due to H5N1 bird flu, it also has the potential to mutate to cause a human pandemic.
Birds and humans have different types of receptors in their respiratory tract that flu viruses attach to, like a lock (receptors) and key (virus). The attachment of the virus allows it to invade a cell and the body and cause illness. Avian flu viruses are adapted to birds, and spread easily among birds, but not in humans.
So far, human cases have mainly occurred in people who have been in close contact with infected farm animals or birds. In the US, most have been farm workers.
The concern is that the virus will mutate and adapt to humans. One of the key steps for this to happen would be a shift in the virus’ affinity from the bird receptors to those found in the human respiratory tract. In other words, if the virus’ “key” mutated to better fit with the human “lock”.
A recent study of a sample of A/H5N1 2.3.4.4b from an infected human had worrying findings, identifying mutations in the virus with the potential to increase transmission between human hosts.
Why are pigs a problem?
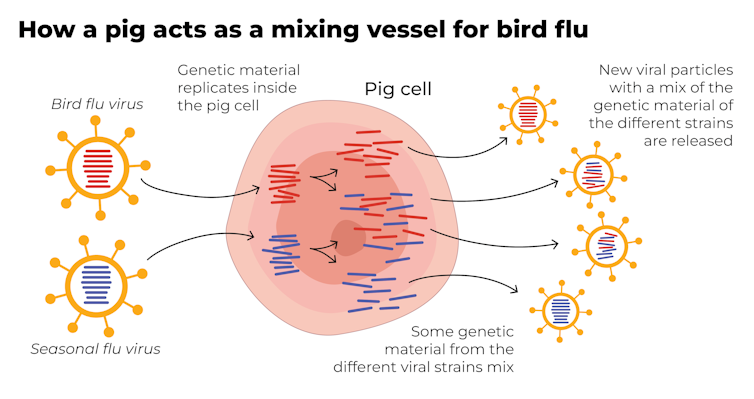
A human pandemic strain of influenza can arise in several ways. One involves close contact between humans and animals infected with their own specific flu viruses, creating opportunities for genetic mixing between avian and human viruses.
Pigs are the ideal genetic mixing vessel to generate a human pandemic influenza strain, because they have receptors in their respiratory tracts which both avian and human flu viruses can bind to.
This means pigs can be infected with a bird flu virus and a human flu virus at the same time. These viruses can exchange genetic material to mutate and become easily transmissible in humans.
The Conversation, CC BY-SA Interestingly, in the past pigs were less susceptible to A/H5N1 viruses. However, the virus has recently mutated to infect pigs more readily.
In the recent case in Oregon, A/H5N1 was detected in a pig on a non-commercial farm after an outbreak occurred among the poultry housed on the same farm. This strain of A/H5N1 was from wild birds, not the one that is widespread in US dairy cows.
The infection of a pig is a warning. If the virus enters commercial piggeries, it would create a far greater level of risk of a pandemic, especially as the US goes into winter, when human seasonal flu starts to rise.
How can we mitigate the risk?
Surveillance is key to early detection of a possible pandemic. This includes comprehensive testing and reporting of infections in birds and animals, alongside financial compensation and support measures for farmers to encourage timely reporting.
Strengthening global influenza surveillance is crucial, as unusual spikes in pneumonia and severe respiratory illnesses could signal a human pandemic. Our EPIWATCH system looks for early warnings of such activity, which can speed up vaccine development.
If a cluster of human cases occurs, and influenza A is detected, further testing (called subtyping) is essential to ascertain whether it’s a seasonal strain, an avian strain from a spillover event, or a novel pandemic strain.
Early identification can prevent a pandemic. Any delay in identifying an emerging pandemic strain enables the virus to spread widely across international borders.
Australia’s first human case of A/H5N1 occurred in a child who acquired the infection while travelling in India, and was hospitalised with illness in March 2024. At the time, testing revealed Influenza A (which could be seasonal flu or avian flu), but subtyping to identify A/H5N1 was delayed.
This kind of delay can be costly if a human-transmissible A/H5N1 arises and is assumed to be seasonal flu because the test is positive for influenza A. Only about 5% of tests positive for influenza A are subtyped further in Australia and most countries.
In light of the current situation, there should be a low threshold for subtyping influenza A strains in humans. Rapid tests which can distinguish between seasonal and H5 influenza A are emerging, and should form part of governments’ pandemic preparedness.
A higher risk than ever before
The US Centers for Disease Control and Prevention states that the current risk posed by H5N1 to the general public remains low.
But with H5N1 now able to infect pigs, and showing worrying mutations for human adaptation, the level of risk has increased. Given the virus is so widespread in animals and birds, the statistical probability of a pandemic arising is higher than ever before.
The good news is, we are better prepared for an influenza pandemic than other pandemics, because vaccines can be made in the same way as seasonal flu vaccines. As soon as the genome of a pandemic influenza virus is known, the vaccines can be updated to match it.
Partially matched vaccines are already available, and some countries such as Finland are vaccinating high-risk farm workers.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney and Haley Stone, Research Associate, Biosecurity Program, Kirby Institute & CRUISE lab, Computer Science and Engineering, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Many Nonprofit (Wink, Wink) Hospitals Are Rolling in Money
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One owns a for-profit insurer, a venture capital company, and for-profit hospitals in Italy and Kazakhstan; it has just acquired its fourth for-profit hospital in Ireland. Another owns one of the largest for-profit hospitals in London, is partnering to build a massive training facility for a professional basketball team, and has launched and financed 80 for-profit start-ups. Another partners with a wellness spa where rooms cost $4,000 a night and co-invests with “leading private equity firms.”
Do these sound like charities?
These diversified businesses are, in fact, some of the country’s largest nonprofit hospital systems. And they have somehow managed to keep myriad for-profit enterprises under their nonprofit umbrella — a status that means they pay little or no taxes, float bonds at preferred rates, and gain numerous other financial advantages.
Through legal maneuvering, regulatory neglect, and a large dollop of lobbying, they have remained tax-exempt charities, classified as 501(c)(3)s.
“Hospitals are some of the biggest businesses in the U.S. — nonprofit in name only,” said Martin Gaynor, an economics and public policy professor at Carnegie Mellon University. “They realized they could own for-profit businesses and keep their not-for-profit status. So the parking lot is for-profit; the laundry service is for-profit; they open up for-profit entities in other countries that are expressly for making money. Great work if you can get it.”
Many universities’ most robust income streams come from their technically nonprofit hospitals. At Stanford University, 62% of operating revenue in fiscal 2023 was from health services; at the University of Chicago, patient services brought in 49% of operating revenue in fiscal 2022.
To be sure, many hospitals’ major source of income is still likely to be pricey patient care. Because they are nonprofit and therefore, by definition, can’t show that thing called “profit,” excess earnings are called “operating surpluses.” Meanwhile, some nonprofit hospitals, particularly in rural areas and inner cities, struggle to stay afloat because they depend heavily on lower payments from Medicaid and Medicare and have no alternative income streams.
But investments are making “a bigger and bigger difference” in the bottom line of many big systems, said Ge Bai, a professor of health care accounting at the Johns Hopkins University Bloomberg School of Public Health. Investment income helped Cleveland Clinic overcome the deficit incurred during the pandemic.
When many U.S. hospitals were founded over the past two centuries, mostly by religious groups, they were accorded nonprofit status for doling out free care during an era in which fewer people had insurance and bills were modest. The institutions operated on razor-thin margins. But as more Americans gained insurance and medical treatments became more effective — and more expensive — there was money to be made.
Not-for-profit hospitals merged with one another, pursuing economies of scale, like joint purchasing of linens and surgical supplies. Then, in this century, they also began acquiring parts of the health care systems that had long been for-profit, such as doctors’ groups, as well as imaging and surgery centers. That raised some legal eyebrows — how could a nonprofit simply acquire a for-profit? — but regulators and the IRS let it ride.
And in recent years, partnerships with, and ownership of, profit-making ventures have strayed further and further afield from the purported charitable health care mission in their community.
“When I first encountered it, I was dumbfounded — I said, ‘This not charitable,’” said Michael West, an attorney and senior vice president of the New York Council of Nonprofits. “I’ve long questioned why these institutions get away with it. I just don’t see how it’s compliant with the IRS tax code.” West also pointed out that they don’t act like charities: “I mean, everyone knows someone with an outstanding $15,000 bill they can’t pay.”
Hospitals get their tax breaks for providing “charity care and community benefit.” But how much charity care is enough and, more important, what sort of activities count as “community benefit” and how to value them? IRS guidance released this year remains fuzzy on the issue.
Academics who study the subject have consistently found the value of many hospitals’ good work pales in comparison with the value of their tax breaks. Studies have shown that generally nonprofit and for-profit hospitals spend about the same portion of their expenses on the charity care component.
Here are some things listed as “community benefit” on hospital systems’ 990 tax forms: creating jobs; building energy-efficient facilities; hiring minority- or women-owned contractors; upgrading parks with lighting and comfortable seating; creating healing gardens and spas for patients.
All good works, to be sure, but health care?
What’s more, to justify engaging in for-profit business while maintaining their not-for-profit status, hospitals must connect the business revenue to that mission. Otherwise, they pay an unrelated business income tax.
“Their CEOs — many from the corporate world — spout drivel and turn somersaults to make the case,” said Lawton Burns, a management professor at the University of Pennsylvania’s Wharton School. “They do a lot of profitable stuff — they’re very clever and entrepreneurial.”
The truth is that a number of not-for-profit hospitals have become wealthy diversified business organizations. The most visible manifestation of that is outsize executive compensation at many of the country’s big health systems. Seven of the 10 most highly paid nonprofit CEOs in the United States run hospitals and are paid millions, sometimes tens of millions, of dollars annually. The CEOs of the Gates and Ford foundations make far less, just a bit over $1 million.
When challenged about the generous pay packages — as they often are — hospitals respond that running a hospital is a complicated business, that pharmaceutical and insurance execs make much more. Also, board compensation committees determine the payout, considering salaries at comparable institutions as well as the hospital’s financial performance.
One obvious reason for the regulatory tolerance is that hospital systems are major employers — the largest in many states (including Massachusetts, Pennsylvania, Minnesota, Arizona, and Delaware). They are big-time lobbying forces and major donors in Washington and in state capitals.
But some patients have had enough: In a suit brought by a local school board, a judge last year declared that four Pennsylvania hospitals in the Tower Health system had to pay property taxes because its executive pay was “eye popping” and it demonstrated “profit motives through actions such as charging management fees from its hospitals.”
A 2020 Government Accountability Office report chided the IRS for its lack of vigilance in reviewing nonprofit hospitals’ community benefit and recommended ways to “improve IRS oversight.” A follow-up GAO report to Congress in 2023 said, “IRS officials told us that the agency had not revoked a hospital’s tax-exempt status for failing to provide sufficient community benefits in the previous 10 years” and recommended that Congress lay out more specific standards. The IRS declined to comment for this column.
Attorneys general, who regulate charity at the state level, could also get involved. But, in practice, “there is zero accountability,” West said. “Most nonprofits live in fear of the AG. Not hospitals.”
Today’s big hospital systems do miraculous, lifesaving stuff. But they are not channeling Mother Teresa. Maybe it’s time to end the community benefit charade for those that exploit it, and have these big businesses pay at least some tax. Communities could then use those dollars in ways that directly benefit residents’ health.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Older Americans Say They Feel Trapped in Medicare Advantage Plans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2016, Richard Timmins went to a free informational seminar to learn more about Medicare coverage.
“I listened to the insurance agent and, basically, he really promoted Medicare Advantage,” Timmins said. The agent described less expensive and broader coverage offered by the plans, which are funded largely by the government but administered by private insurance companies.
For Timmins, who is now 76, it made economic sense then to sign up. And his decision was great, for a while.
Then, three years ago, he noticed a lesion on his right earlobe.
“I have a family history of melanoma. And so, I was kind of tuned in to that and thinking about that,” Timmins said of the growth, which doctors later diagnosed as malignant melanoma. “It started to grow and started to become rather painful.”
Timmins, though, discovered that his enrollment in a Premera Blue Cross Medicare Advantage plan would mean a limited network of doctors and the potential need for preapproval, or prior authorization, from the insurer before getting care. The experience, he said, made getting care more difficult, and now he wants to switch back to traditional, government-administered Medicare.
But he can’t. And he’s not alone.
“I have very little control over my actual medical care,” he said, adding that he now advises friends not to sign up for the private plans. “I think that people are not understanding what Medicare Advantage is all about.”
Enrollment in Medicare Advantage plans has grown substantially in the past few decades, enticing more than half of all eligible people, primarily those 65 or older, with low premium costs and perks like dental and vision insurance. And as the private plans’ share of the Medicare patient pie has ballooned to 30.8 million people, so too have concerns about the insurers’ aggressive sales tactics and misleading coverage claims.
Enrollees, like Timmins, who sign on when they are healthy can find themselves trapped as they grow older and sicker.
“It’s one of those things that people might like them on the front end because of their low to zero premiums and if they are getting a couple of these extra benefits — the vision, dental, that kind of thing,” said Christine Huberty, a lead benefit specialist supervising attorney for the Greater Wisconsin Agency on Aging Resources.
“But it’s when they actually need to use it for these bigger issues,” Huberty said, “that’s when people realize, ‘Oh no, this isn’t going to help me at all.’”
Medicare pays private insurers a fixed amount per Medicare Advantage enrollee and in many cases also pays out bonuses, which the insurers can use to provide supplemental benefits. Huberty said those extra benefits work as an incentive to “get people to join the plan” but that the plans then “restrict the access to so many services and coverage for the bigger stuff.”
David Meyers, assistant professor of health services, policy, and practice at the Brown University School of Public Health, analyzed a decade of Medicare Advantage enrollment and found that about 50% of beneficiaries — rural and urban — left their contract by the end of five years. Most of those enrollees switched to another Medicare Advantage plan rather than traditional Medicare.
In the study, Meyers and his co-authors muse that switching plans could be a positive sign of a free marketplace but that it could also signal “unmeasured discontent” with Medicare Advantage.
“The problem is that once you get into Medicare Advantage, if you have a couple of chronic conditions and you want to leave Medicare Advantage, even if Medicare Advantage isn’t meeting your needs, you might not have any ability to switch back to traditional Medicare,” Meyers said.
Traditional Medicare can be too expensive for beneficiaries switching back from Medicare Advantage, he said. In traditional Medicare, enrollees pay a monthly premium and, after reaching a deductible, in most cases are expected to pay 20% of the cost of each nonhospital service or item they use. And there is no limit on how much an enrollee may have to pay as part of that 20% coinsurance if they end up using a lot of care, Meyers said.
To limit what they spend out-of-pocket, traditional Medicare enrollees typically sign up for supplemental insurance, such as employer coverage or a private Medigap policy. If they are low-income, Medicaid may provide that supplemental coverage.
But, Meyers said, there’s a catch: While beneficiaries who enrolled first in traditional Medicare are guaranteed to qualify for a Medigap policy without pricing based on their medical history, Medigap insurers can deny coverage to beneficiaries transferring from Medicare Advantage plans or base their prices on medical underwriting.
Only four states — Connecticut, Maine, Massachusetts, and New York — prohibit insurers from denying a Medigap policy if the enrollee has preexisting conditions such as diabetes or heart disease.
Paul Ginsburg is a former commissioner on the Medicare Payment Advisory Commission, also known as MedPAC. It’s a legislative branch agency that advises Congress on the Medicare program. He said the inability of enrollees to easily switch between Medicare Advantage and traditional Medicare during open enrollment periods is “a real concern in our system; it shouldn’t be that way.”
The federal government offers specific enrollment periods every year for switching plans. During Medicare’s open enrollment period, from Oct. 15 to Dec. 7, enrollees can switch out of their private plans to traditional, government-administered Medicare.
Medicare Advantage enrollees can also switch plans or transfer to traditional Medicare during another open enrollment period, from Jan. 1 to March 31.
“There are a lot of people that say, ‘Hey, I’d love to come back, but I can’t get Medigap anymore, or I’ll have to just pay a lot more,’” said Ginsburg, who is now a professor of health policy at the University of Southern California.
Timmins is one of those people. The retired veterinarian lives in a rural community on Whidbey Island just north of Seattle. It’s a rugged, idyllic landscape and a popular place for second homes, hiking, and the arts. But it’s also a bit remote.
While it’s typically harder to find doctors in rural areas, Timmins said he believes his Premera Blue Cross plan made it more challenging to get care for a variety of reasons, including the difficulty of finding and getting in to see specialists.
Nearly half of Medicare Advantage plan directories contained inaccurate information on what providers were available, according to the most recent federal review. Beginning in 2024, new or expanding Medicare Advantage plans must demonstrate compliance with federal network expectations or their applications could be denied.
Amanda Lansford, a Premera Blue Cross spokesperson, declined to comment on Timmins’ case. She said the plan meets federal network adequacy requirements as well as travel time and distance standards “to ensure members are not experiencing undue burdens when seeking care.”
Traditional Medicare allows beneficiaries to go to nearly any doctor or hospital in the U.S., and in most cases enrollees do not need approval to get services.
Timmins, who recently finished immunotherapy, said he doesn’t think he would be approved for a Medigap policy, “because of my health issue.” And if he were to get into one, Timmins said, it would likely be too expensive.
For now, Timmins said, he is staying with his Medicare Advantage plan.
“I’m getting older. More stuff is going to happen.”
There is also a chance, Timmins said, that his cancer could resurface: “I’m very aware of my mortality.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: