Unprocessed – by Kimberly Wilson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: hundreds of pages to say “eat less processed food”. That is, of course, also advisable (and indeed, is advised in the book too), but there’s a lot more going on here too.
Though not a doctor, the author is a psychologist who brings a lot of data to the table, especially when it comes to the neurophysiology at hand, what forgotten micronutrients many people are lacking, and what trends in society worsen these deficiencies in the population at large.
If you only care about the broadest of take-away advice, it is: eat a diet that’s mostly minimally processed plants and some oily fish, watch out for certain deficiencies in particular, and increase dietary intake of them where necessary (with taking supplements as a respectable next-best remedy).
On which note, a point of criticism is that there’s some incorrect information about veganism and brain health; she mentions that DHA is only found in fish (in fact, fish get it from algae, which has it, and is the basis of many vegan omega-3 supplements), and the B12 is found only in animals (also found in yeast, which is not an animal, as well as various bacteria in soil, and farm animals get their B12 from supplements these days anyway, so it is arguable that we could keep things simpler by just cutting out the middlecow).
However, the strength of this book really is in the delivery of understanding about why certain things matter. If you’re told “such-and-such is good for the brain”, you’ll up your intake for 1–60 days, depending on whether you bought a supermarket item or ordered a batch of supplements. And then you’ll forget, until 6–12 months later, and you’ll do it again. On the other hand, if you understand how something is good or bad for the brain, what it does (for good or ill) on a cellular level, the chemistry and neurophysiology at hand, you’ll make new habits for life.
The style is middle-range pop-science; by this we mean there are tables of data and some long words that are difficult to pronounce, but also it’s not just hard science throughout—there’s (as one might expect from an author who is a psychologist) a lot about the psychology and sociology of why many people make poor dietary decisions, and the things governments often do (or omit doing) that affect this adversely—and how we can avoid those traps as individuals (unless we be incarcerated or such).
As an aside, the author is British, so governmental examples are mostly UK-based, but it doesn’t take a lot to mentally measure that against what the governments of, for example, the US or Canada do the same or differently.
Bottom line: there’s a lot of great information about brain health here; the strongest parts are whether the author stays within her field (psychology encompasses such diverse topics as neurophysiology and aspects of sociology, but not microbiology, for example). If you want to learn about the physiology of brain health and enjoy quite a sociopolitical ride along the way, this one’s a good one for that.
Click here to check out Unprocessed, and make the best choices for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Staring At The Sun – by Dr. Irvin Yalom
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note first: there are two editions of this book; the content is the same, but the cover is different. So if in your region it has a bright yellow cover and the subtitle is the excitable “Overcoming The Terror Of Death” rather than the more measured “Being At Peace With Your Own Mortality”, that is why; different regional publishers made different choices.
For most of us, dying is the last thing we want to do. We may fear it; we may ignore it; we may try to beat it—but it’s a constant existential threat whether we want it or not.
This book is about “death anxiety”, either direct (conscious fear of impending death) or sublimated (not necessarily realising what we’re avoiding thinking about it). In its broadest sense, the fear of death can be described as rational. But angst about it probably won’t help, so this book looks to help us overcome that.
The style of the book is largely anecdotal, in which the author uses examples from his therapeutic practice to illustrate ways in which the fear of death can manifest, and ways in which it can be managed healthily.
Subjective criticism: while this author developed existential therapy, many of the ideas in this book lean heavily on the psychodynamic approach derived from Freud, and this reviewer isn’t a fan of that. But nevertheless, many of the examples here are thought-provoking and useful, so it is not too strong a criticism.
Bottom line: there are many ways to manage one’s mortality, and this book brings attention to a range of possibilities.
Click here to check out Staring At The Sun, and manage your mortality!
Share This Post
-
The Power of Self-Care – by Dr. Sunil Kumar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is mostly not about: bubble baths and scented candles. We say “mostly”, because stress management is an important aspect given worthy treatment in this book, but there is more emphasis on evidence-based interventions and thus Dr. Kumar is readier to prescribe nature walks and meditation, than product-based pampering sessions.
As is made clear in the subtitle “Transforming Heart Health with Lifestyle Medicine”, the focus is on heart health throughout, but as 10almonds readers know, “what’s good for your heart is good for your brain” is a truism that indeed holds true here too.
Dr. Kumar also gives nutritional tweaks to optimize heart health, and includes a selection of heart-healthy recipes, too. And exercise? Yes, customizable exercise plans, even. And a plan for getting sleep into order if perchance it has got a bit out of hand (most people get less sleep than necessary for maintenance of good health), and he even delves into “social prescribing”, that is to say, making sure that one’s social connectedness does not get neglected—without letting it, conversely, take over too much of one’s life (done badly, social connectedness can be a big source of unmanaged stress).
Perhaps the most value of this book comes from its 10-week self-care plan (again, with a focus on heart health), basically taking the reader by the hand for long enough that, after those 10 weeks, habits should be quite well-ingrained.
A strong idea throughout is that the things we take up should be sustainable, because well, a heart is for life, not just for a weekend retreat.
Bottom line: if you’d like to improve your heart health in a way that feels like self-care rather than an undue amount of work, then this is the book for you.
Share This Post
-
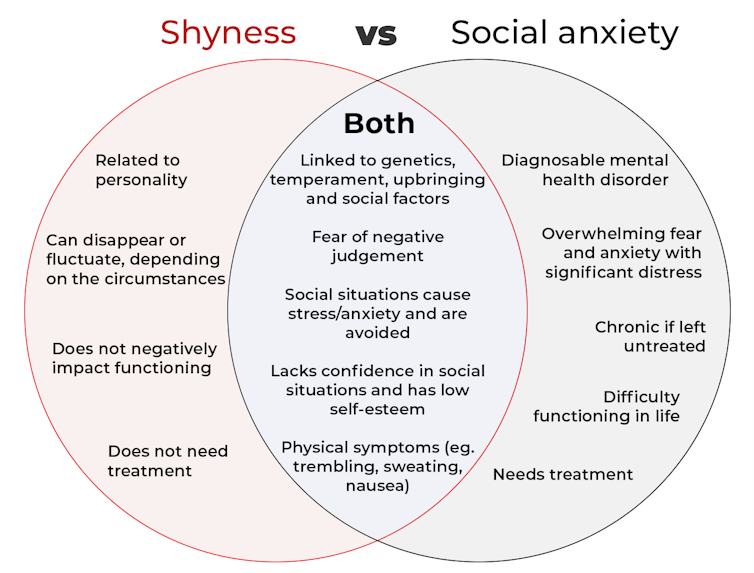
What’s the difference between shyness and social anxiety?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
The terms “shyness” and “social anxiety” are often used interchangeably because they both involve feeling uncomfortable in social situations.
However, feeling shy, or having a shy personality, is not the same as experiencing social anxiety (short for “social anxiety disorder”).
Here are some of the similarities and differences, and what the distinction means.
pathdoc/Shutterstock How are they similar?
It can be normal to feel nervous or even stressed in new social situations or when interacting with new people. And everyone differs in how comfortable they feel when interacting with others.
For people who are shy or socially anxious, social situations can be very uncomfortable, stressful or even threatening. There can be a strong desire to avoid these situations.
People who are shy or socially anxious may respond with “flight” (by withdrawing from the situation or avoiding it entirely), “freeze” (by detaching themselves or feeling disconnected from their body), or “fawn” (by trying to appease or placate others).
A complex interaction of biological and environmental factors is also thought to influence the development of shyness and social anxiety.
For example, both shy children and adults with social anxiety have neural circuits that respond strongly to stressful social situations, such as being excluded or left out.
People who are shy or socially anxious commonly report physical symptoms of stress in certain situations, or even when anticipating them. These include sweating, blushing, trembling, an increased heart rate or hyperventilation.
How are they different?
Social anxiety is a diagnosable mental health condition and is an example of an anxiety disorder.
For people who struggle with social anxiety, social situations – including social interactions, being observed and performing in front of others – trigger intense fear or anxiety about being judged, criticised or rejected.
To be diagnosed with social anxiety disorder, social anxiety needs to be persistent (lasting more than six months) and have a significant negative impact on important areas of life such as work, school, relationships, and identity or sense of self.
Many adults with social anxiety report feeling shy, timid and lacking in confidence when they were a child. However, not all shy children go on to develop social anxiety. Also, feeling shy does not necessarily mean a person meets the criteria for social anxiety disorder.
People vary in how shy or outgoing they are, depending on where they are, who they are with and how comfortable they feel in the situation. This is particularly true for children, who sometimes appear reserved and shy with strangers and peers, and outgoing with known and trusted adults.
Individual differences in temperament, personality traits, early childhood experiences, family upbringing and environment, and parenting style, can also influence the extent to which people feel shy across social situations.
Not all shy children go on to develop social anxiety. 249 Anurak/Shutterstock However, people with social anxiety have overwhelming fears about embarrassing themselves or being negatively judged by others; they experience these fears consistently and across multiple social situations.
The intensity of this fear or anxiety often leads people to avoid situations. If avoiding a situation is not possible, they may engage in safety behaviours, such as looking at their phone, wearing sunglasses or rehearsing conversation topics.
The effect social anxiety can have on a person’s life can be far-reaching. It may include low self-esteem, breakdown of friendships or romantic relationships, difficulties pursuing and progressing in a career, and dropping out of study.
The impact this has on a person’s ability to lead a meaningful and fulfilling life, and the distress this causes, differentiates social anxiety from shyness.
Children can show similar signs or symptoms of social anxiety to adults. But they may also feel upset and teary, irritable, have temper tantrums, cling to their parents, or refuse to speak in certain situations.
If left untreated, social anxiety can set children and young people up for a future of missed opportunities, so early intervention is key. With professional and parental support, patience and guidance, children can be taught strategies to overcome social anxiety.
Why does the distinction matter?
Social anxiety disorder is a mental health condition that persists for people who do not receive adequate support or treatment.
Without treatment, it can lead to difficulties in education and at work, and in developing meaningful relationships.
Receiving a diagnosis of social anxiety disorder can be validating for some people as it recognises the level of distress and that its impact is more intense than shyness.
A diagnosis can also be an important first step in accessing appropriate, evidence-based treatment.
Different people have different support needs. However, clinical practice guidelines recommend cognitive-behavioural therapy (a kind of psychological therapy that teaches people practical coping skills). This is often used with exposure therapy (a kind of psychological therapy that helps people face their fears by breaking them down into a series of step-by-step activities). This combination is effective in-person, online and in brief treatments.
Treatment is available online as well as in-person. ImYanis/Shutterstock For more support or further reading
Online resources about social anxiety include:
- This Way Up’s online program for managing excessive shyness and fear of social situations
- Beyond Blue’s resources on social anxiety
- a guide to looking after yourself if you have social anxiety, from the Western Australian health department
- social anxiety online program for children and teens from the University of Queensland
- inroads, a self-guided online program for young adults who drink alcohol to manage their anxiety.
We thank the Black Dog Institute Lived Experience Advisory Network members for providing feedback and input for this article and our research.
Kayla Steele, Postdoctoral research fellow and clinical psychologist, UNSW Sydney and Jill Newby, Professor, NHMRC Emerging Leader & Clinical Psychologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Top 10 Unhealthy Foods: How Many Do You Eat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The items on this list won’t come as a shocking surprise to you, but it can be a good opportunity to do a quick tally and see how many of these have snuck into your diet:
The things that take away health instead of adding it
Without further ado, they are…
- Alcohol: not only is it high in empty calories, but also it’s bad for pretty much everything, especially increasing the risks of liver disease, high blood pressure, and stroke.
- Processed snacks: low in nutrition; contain unhealthy fats, refined sugars, and artificial additives that often aren’t great.
- Potato chips: get their own category for being especially high in fat, sodium, and empty calories; contribute to heart disease and weight gain.
- Processed cheese: some kinds of cheese are gut-healthy in moderation, but this isn’t. Instead, it’s just loaded with saturated fats, sodium, and sugars, and is pretty much heart disease in a slice.
- Donuts: deep-fried, sugary, and made with refined flour; cause blood sugar spikes and crashes, and what’s bad for your blood sugars is bad for almost everything else.
- French fries & similar deep-fried foods: high in saturated fats and sodium; contribute to obesity and heart issues, are not great for blood sugars either.
- White bread: made with refined flour; cause blood sugar spikes and metabolic woes.
- Sodas: high in sugar or artificial sweeteners; can easily lead to weight gain, diabetes, and tooth decay.
- Processed meats: high in calories and salt; strongly associated with heart disease and cancer.
- Hot dogs & fast food burgers: get their own category for being the absolute worst of the above-mentioned processed meats.
This writer scored: no / rarely / no / no / no / rarely / rarely / rarely / no / no
How about you?
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Securely Attached –
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of books on attachment theory are quite difficult to read. They’re often either too clinical with too much jargon that can feel like incomprehensible psychobabble, or else too wishy-washy and it starts to sound like a horoscope for psychology enthusiasts.
This one does it better.
The author gives us a clear overview and outline of attachment theory, with minimal jargon and/but clearly defined terms, and—which is a boon for anyone struggling to remember which general attachment pattern is which—color-codes everything consistently along the way. This is one reason that we recommend getting a print copy of the book, not the e-book.
The other reason to invest in the print copy rather than the e-book is the option to use parts of it as a workbook directly—though if preferred, one can simply take the prompts and use them, without writing in the book, of course.
It’s hard to say what the greatest value of this book is because there are two very strong candidates:
- Super-clear and easy explanation of Attachment Theory, in a way that actually makes sense and will stick
- Excellent actually helpful advice on improving how we use the knowledge that we now have of our own attachment patterns and those of others
Bottom line: if you’d like to better understand Attachment Theory and apply it to your life, but have been put off by other presentations of it, this is the most user-friendly, no-BS version that this reviewer has seen.
Click here to check out Securely Attached, and upgrade your relationship(s)!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Carrot vs Kale – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrot to kale, we picked the kale.
Why?
These are both known as carotene-containing heavyweights, but kale emerges victorious:
In terms of macros, carrot has more carbs while kale has more protein and fiber. An easy win there for kale.
When it comes to vitamins, both are great! But, carrots contain more of vitamins A, B5, and choline, whereas kale contains more of vitamins B1, B2, B3, B6, B9, C, E, and K. And while carrot’s strongest point is vitamin A, a cup of carrots contains around 10x the recommended daily dose of vitamin A, whereas a cup of kale contains “only” 6x the recommended daily dose of vitamin A. So, did we really need the extra in carrots? Probably not. In any case, kale already won on overall vitamin coverage, by a long way.
In the category of minerals, kale again sweeps. On the one hand, carrots contain more sodium. On the other hand, kale contains a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Not a tricky choice!
But don’t be fooled: carrots really are a nutritional powerhouse and a great food. Kale is just better—nutritionally speaking, in any case. If you’re making a carrot cake, please don’t try substituting kale; it will not work 😉
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: