The Inflamed Mind – by Dr. Edward Bullmore
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, let’s note that this book was published in 2018, so the “radical new” approach is more like “tried and tested and validated” now.
Of course, inflammation in the brain is also linked to Alzheimer’s, Parkinson’s, and other neurodegenerative disorders, but that’s not the main topic here.
Dr. Bullmore, a medical doctor, psychiatrist, and neuroscientist with half the alphabet after his name, knows his stuff. We don’t usually include author bio information here, but it’s also relevant that he has published more than 500 scientific papers and is one of the most highly cited scientists worldwide in neuroscience and psychiatry.
What he explores in this book, with a lot of hard science made clear for the lay reader, is the mechanisms of action of depression treatments that aren’t just SSRIs, and why anti-inflammatory approaches can work for people with “treatment-resistant depression”.
The book was also quite prescient in its various declarations of things he expects to happen in the field in the next five years, because they’ve happened now, five years later.
Bottom line: if you’d like to understand how the mind and body affect each other in the cases of inflammation and depression, with a view to lessening either or both of those things, this is a book for you.
Click here to check out The Inflamed Mind, and take good care of yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
53 Studies Later: The Best Way to Improve VO2 Max
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
VO2 max measures maximum oxygen usage during intense exercise and reflects overall health and performance. To have a high VO2 max, efficient functioning of lungs, heart, red blood cells, muscles, and mitochondria is crucial. So, how to get those?
Let’s HIIT it!
High-Intensity Interval Training (HIIT) outperforms moderate-intensity exercise, by a long way. Further, based on the data from the 53 studies mentioned in the title, we can know which of the protocols tested work best, and they are:
- 15×15 Interval Training: 15 seconds sprint (90–95% max heart rate) + 15 seconds active rest (70% max heart rate), repeated 47 times.
- 4×4 Interval Training: 4 minutes sprint (90–95% max heart rate) + 3 minutes active rest (70% max heart rate), repeated 4 times.
Whichever you choose, it is best to then do that 3x per week.
Note that “sprint” can mean any maximum-effort cardio exercise; it doesn’t have to be running specifically. Cycling or swimming, for example, are fine options too, as is jumping rope.
For more on each of these, plus how the science got there, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Do HIIT (Without Wrecking Your Body)
Take care!
Share This Post
-
The Only Exercise You Need To Strengthen Every Hip Muscle (Ages 50+)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One exercise, no equipment, and easy to do without even getting changed:
You may be on the fence about this one
Standing on one leg is great, of course, and then…
Basic exercise:
- Imagine stepping over an electric fence side to side.
- Lift each leg high but slowly to engage hip muscles.
- Adjust the height and speed based on ease/difficulty.
Variations:
- Step over an imaginary side fence.
- Step over an imaginary front fence.
- Step sideways in the opposite direction.
- Step backward to complete a square.
- Ensure both legs are worked evenly.
As a bonus, it also improves balance!
For more on all this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How Tight Are Your Hips? Test (And Fix!) With This
Take care!
Share This Post
-
Dr. Kim Foster’s Method For Balancing Hormones Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not just sex hormones, but also hormones like cortisol (the stress hormone), and thyroid hormones (for metabolism regulation) too! The body is most of the time self-regulating when it comes to hormones, but there are things that we can do to help our body look after us correctly.
In short, if we give our body what it needs, it will (usually, barring serious illness!) give us what we need.
Dr. Foster recommends…
Foods:
- Healthy fats (especially avocados and nuts)
- Lean proteins (especially poultry, fish, and legumes)
- Fruits & vegetables (especially colorful ones)
- Probiotics (especially fermented foods like sauerkraut, kimchi, etc)
- Magnesium-rich foods (especially dark leafy greens, nuts, and yes, dark chocolate)
Teas:
- Camomile tea (especially beneficial against cortisol overproduction)
- Nettle tea (especially beneficial for estrogen production)
- Peppermint tea (especially beneficial for gut health, thus indirect hormone benefits)
Stress reduction:
- Breathing exercises (especially mindfulness exercises)
- Yoga (especially combining exercise with stretches)
- Spending time in nature (especially green spaces)
Dr. Foster explains more about all of these things, along with more illustrative examples, so if you can, do enjoy her video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to read more about this topic?
You might like our main feature: What Does “Balance Your Hormones” Even Mean?
Enjoy!
Share This Post
Related Posts
-
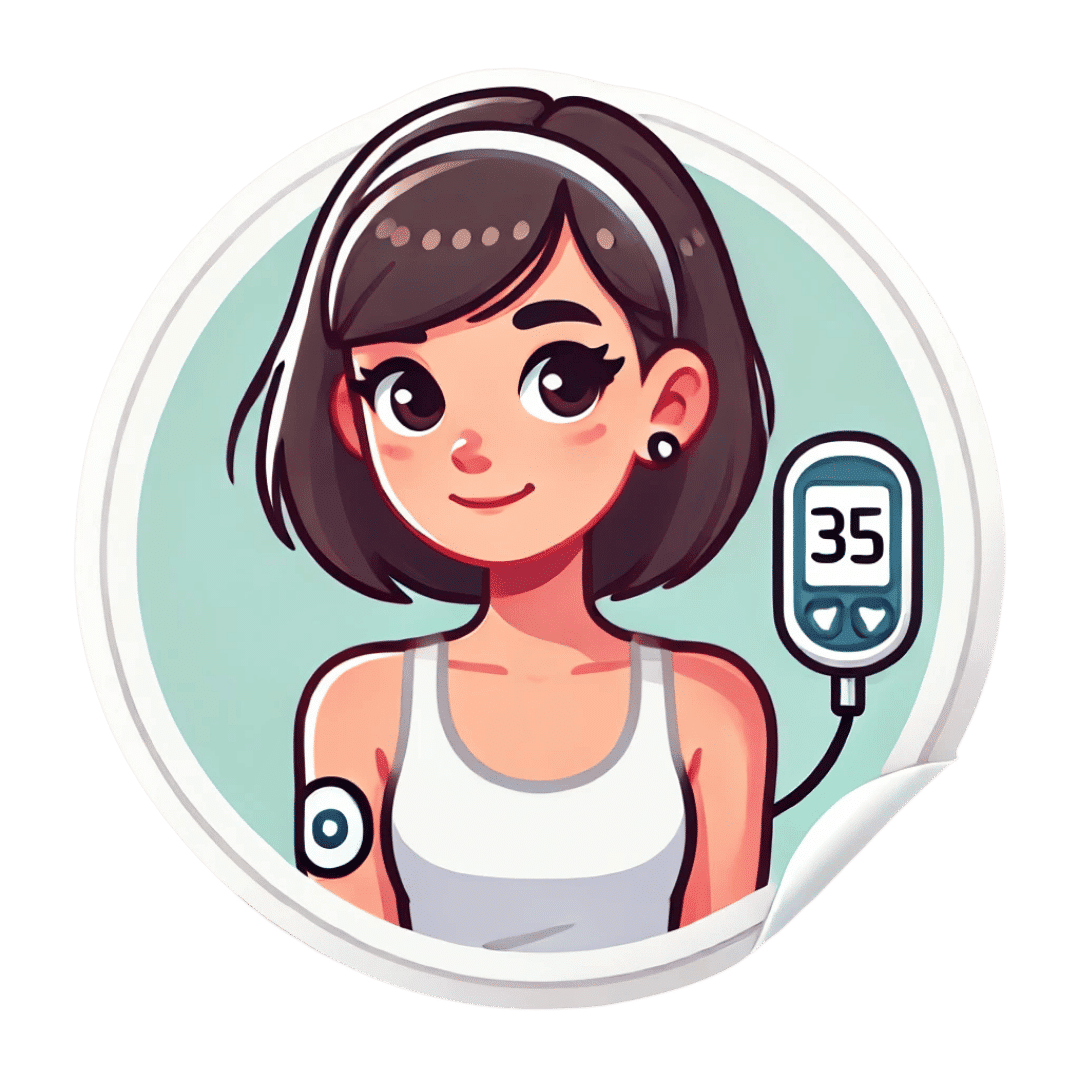
Continuous Glucose Monitors Without Diabetes: Pros & Cons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The “Glucose Goddess”, biochemist Jessie Inchauspé, gives us the low-down:
Knowledge is power (but watch out)
A continuous glucose monitor (CGM) is a device that continually monitors glucose levels, without the need to stab one’s finger every few hours to test blood.
It was designed for diabetics, especially for those with Type 1 Diabetes, where around-the-clock monitoring is necessary for appropriate insulin dosing.
For non-diabetics, they can be a good way of learning what our body’s response to various foods and activities is like, the better to be able to tweak our habits to avoid undue glucose spikes (which are harmful for our pancreas, liver, heart, brain, kidneys, and more).
How it works: there’s a sensor that sits on the arm (or elsewhere, but the arm is a popular placement) with a little probe that goes under the skin. It’s applied using a device that inserts it automatically using a needle (you only need to press a button, you don’t need to guide the needle yourself); the needle then retracts, leaving the soft, flexible probe in place. Having been attached, that sensor can now stay in place for 2 weeks (usually; depends on brand, but for example FreeStyle Libre, the most popular brand, the sensors last 2 weeks), and yes, it’s fine to bathe/shower/etc with it. When you want an update from your CGM, you scan it with your phone (or you can buy a dedicated reader, but that is more expensive and unnecessary), and it uploads the data since your last scan.
Pros: it’s convenient and gives a lot of data, so even if you only use it for a short period of time (for example, a month) you can get a very good idea of what affects your blood sugar levels and how. Also, because of the constant nature of the monitoring, it helps avoid accidental sample bias of the kind that can occur with manual testing, by testing a little too soon or too late, and missing a spike/dip.
Cons: it can be expensive, depending on where you live and what options are available for you locally, so you might not want to do it long-term (since that would require buying two sensors per month). It’s also, for all its wealth of data, slightly less accurate than fingerprick testing—that’s because it takes an interstitial reading instead of directly from the blood. For this reason, if you test both ways, you may find a discrepancy of about 3mg/dL. Given that the healthy range is about 70–140mg/dL, a discrepancy of 3mg/dL is probably not going to be important, but it is a thing to mention can (and probably will) happen.
Patterns to bear in mind (with any kind of blood sugar monitoring):
- Dawn phenomenon: a natural glucose rise upon waking.
- Exercise-induced spikes (normal due to energy demands).
- Fat in meals slowing glucose absorption.
- Different foods can sometimes cause a double-wave after dinner (because glucose from different foods is absorbed differently, and/or different foods affect insulin response independent of glucose)
- Steep, rapid spikes that are more harmful than gradual, sustained increases.
- Vitamin C spikes: temporary chemical interference with the sensor, not actual glucose rises.
- Nighttime glucose dips (often false readings caused by sleeping position).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Biohack Your Way to Healthy Skin – by Jennifer Sun
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, an aesthetician with a biotech background, explains about the overlap of skin health and skin beauty, making it better from the inside first (diet and other lifestyle factors), and then tweaking things as desired from the outside.
We previous reviewed another book of hers, “Unleashing Your Best Skin”, and this time the focus is on things you can do at home—not requiring expensive salon treatments (the other book covers both approaches; this one simply skips the clinic work and instead has a lot more detail in the at-home category).
As for what she covers, it comes in categories:
- Gadgets to consider investing in, how to pick good ones, and what gadgets to avoid
- Basic skincare knowledge and practice; here we’re talking cleaners, tonics, moisturizers, and so forth
- Best topical and oral ingredients for the skin (and in contrast, ingredients to be wary of)
- Nutrition for skincare; not just “your skin needs these ingredients”, but also…
- Gut health for skincare, which gets a whole chapter just for that
- Biohacking hormones for skincare, including in the cases of various common hormone imbalances (e.g. menopause, PCOS, etc) and other complications not generally thought of in terms of skincare, such as diabetes and hypo-/hyperthyroidism.
- Circulatory health for skincare (blood and lymph)
- Mental health techniques for skincare (including improving sleep, managing stress, supplements to consider, etc).
As with her other book that we reviewed, the book is broadly aimed at women, and the section on sex-hormonal considerations is completely aimed at women, but as for the rest of the book, there’s no pressing reason why this book couldn’t benefit men too. It also addresses considerations when it comes to darker skintones, something that a lot of similar books overlook.
The style is directly instructional, albeit light and conversational in tone, and still with 20+ pages of scientific references to show that she does indeed know her stuff.
Bottom line: if you’d like to improve your skin health, and/but aren’t a fan of going to the salon, then this book will be an invaluable resource.
Click here to check out Biohack Your Way To Healthy Skin, and biohack your way to healthy skin!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ice Baths: To Dip Or Not To Dip?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
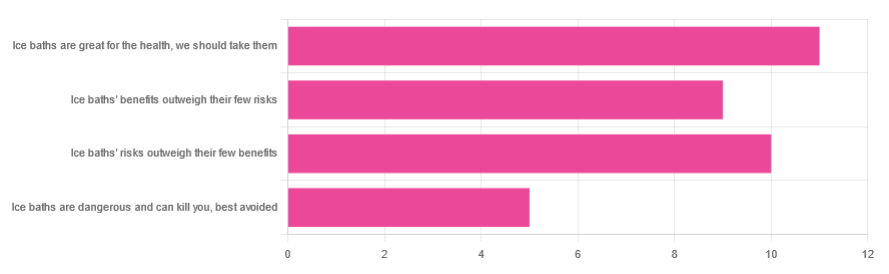
We asked you for your (health-related) view of ice baths, and got the above-depicted, below-described, set of responses:
- About 31% said “ice baths are great for the health; we should take them”
- About 29% said “ice baths’ risks outweigh their few benefits”
- About 26% said “ice baths’ benefits outweigh their few risks”
- About 14% said “ice baths are dangerous and can kill you; best avoided”
So what does the science say?
Freezing water is very dangerous: True or False?
True! Water close to freezing point is indeed very dangerous, and can most certainly kill you.
Fun fact, though: many such people are still saveable with timely medical intervention, in part because the same hypothermia that is killing them also slows down the process* of death
Source (and science) for both parts of that:
Cold water immersion: sudden death and prolonged survival
*and biologically speaking, death is a process, not an event, by the way. But we don’t have room for that today!
(unless you die in some sudden violent way, such as a powerful explosion that destroys your brain instantly; then it’s an event)
Ice baths are thus also very dangerous: True or False?
False! Assuming that they are undertaken responsibly and you have no chronic diseases that make it more dangerous for you.
What does “undertaken responsibly” mean?
Firstly, the temperature should not be near freezing. It should be 10–15℃, which for Americans is 50–59℉.
You can get a bath thermometer to check this, by the way. Here’s an example product on Amazon.
Secondly, your ice bath should last no more than 10–15 minutes. This is not a place to go to sleep.
What chronic diseases would make it dangerous?
Do check with your doctor if you have any doubts, as no list we make can be exhaustive and we don’t know your personal medical history, but the main culprits are:
- Cardiovascular disease
- Hypertension
- Diabetes (any type)
The first two are for heart attack risk; the latter is because diabetes can affect core temperature regulation.
Ice baths are good for the heart: True or False?
True or False depending on how they’re done, and your health before starting.
For most people, undertaking ice baths responsibly, repeated ice bath use causes the cardiovascular system to adapt to better maintain homeostasis when subjected to thermal shock (i.e. sudden rapid changes in temperature).
For example: Respiratory and cardiovascular responses to cold stress following repeated cold water immersion
And because that was a small study, here’s a big research review with a lot of data; just scroll to where it has the heading“Specific thermoregulative adaptations to regular exposure to cold air and/or cold water exposure“ for many examples and much discussion:
Health effects of voluntary exposure to cold water: a continuing subject of debate
Ice baths are good against inflammation: True or False?
True! Here’s one example:
Uric acid and glutathione levels (important markers of chronic inflammation) are also significantly affected:
Uric acid and glutathione levels during short-term whole body cold exposure
Want to know more?
That’s all we have room for today, but check out our previous “Expert Insights” main feature looking at Wim Hof’s work in cryotherapy:
A Cold Shower A Day Keeps The Doctor Away?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: