The Imperfect Nutritionist – by Jennifer Medhurst
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The idea of the “imperfect nutritionist” is to note that we’re all different with slightly different needs and sometimes very different preferences (or circumstances!) and having a truly perfect diet is probably a fool’s errand. Should we just give up, then? Not at all:
What we can do, Medhust argues, is find what’s best for us, realistically.
It’s better to have an 80% perfect diet 80% of the time, than to have a totally perfect diet for four and a half meals before running out of steam (and ingredients).
As for the “seven principles” mentioned in the title… we’re not going to keep those a mystery; they are:
- Focusing on wholefood
- Being diverse
- Knowing your fats
- Including fermented, prebiotic and probiotic foods
- Reducing refined carbohydrates
- Being aware of liquids
- Eating mindfully
The first part of the book is a treatise on how to implement those principles in your diet generally; the second part of the book is a recipe collection—70 recipes, with “these ingredients will almost certainly be available at your local supermarket” as a baseline. No instances of “the secret to being a good chef is knowing how to source fresh ingredients; ask your local greengrocer where to find spring-harvested perambulatory truffle-cones” here!
Basically, it focusses on adding healthy foods per your personal preferences and circumstances, and building these up into a repertoire of meals that will keep you and your family happy and healthy.
Pick Up Your Copy Of The Imperfect Nutritionist From Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Bitter Truth About Coffee (or is it?)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Bitter Truth About Coffee (or is it?)
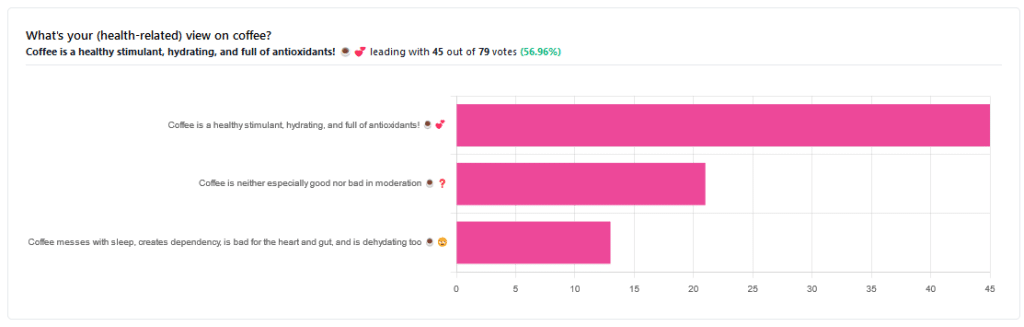
Yesterday, we asked you for your (health-related) views on coffee. The results were clear: if we assume the responses to be representative, we’re a large group of coffee-enthusiasts!
One subscriber who voted for “Coffee is a healthy stimulant, hydrating, and full of antioxidants” wrote:
❝Not so sure about how hydrating it is! Like most food and drink, moderation is key. More than 2 or 3 cups make me buzz! Just too much.❞
And that fine point brings us to our first potential myth:
Coffee is dehydrating: True or False?
False. With caveats…
Coffee, in whatever form we drink it, is wet. This may not come as a startling revelation, but it’s an important starting point. It’s mostly water. Water itself is not dehydrating.
Caffeine, however, is a diuretic—meaning you will tend to pee more. It achieves its diuretic effect by increasing blood flow to your kidneys, which prompts them to release more water through urination.
See: Effect of caffeine on bladder function in patients with overactive bladder symptoms
How much caffeine is required to have a diuretic effect? About 4.5 mg/kg.
What this means in practical terms: if you weigh 70kg (a little over 150lbs), 4.5×70 gives us 315.
315mg is about how much caffeine might be in six shots of espresso. We say “might” because while dosage calculations are an exact science, the actual amount in your shot of espresso can vary depending on many factors, including:
- The kind of coffee bean
- How and when it was roasted
- How and when it was ground
- The water used to make the espresso
- The pressure and temperature of the water
…and that’s all without looking at the most obvious factor: “is the coffee decaffeinated?”
If it doesn’t contain caffeine, it’s not diuretic. Decaffeinated coffee does usually contain tiny amounts of caffeine still, but with nearer 3mg than 300mg, it’s orders of magnitude away from having a diuretic effect.
If it does contain caffeine, then the next question becomes: “and how much water?”
For example, an Americano (espresso, with hot water added to make it a long drink) will be more hydrating than a ristretto (espresso, stopped halfway through pushing, meaning it is shorter and stronger than a normal espresso).
A subscriber who voted for “Coffee messes with sleep, creates dependency, is bad for the heart and gut, and is dehydrating too” wrote:
❝Coffee causes tachycardia for me so staying away is best. People with colon cancer are urged to stay away from coffee completely.❞
These are great points! It brings us to our next potential myth:
Coffee is bad for the heart: True or False?
False… For most people.
Some people, like our subscriber above, have an adverse reaction to caffeine, such as tachycardia. An important reason (beyond basic decency) for anyone providing coffee to honor requests for decaff.
For most people, caffeine is “heart neutral”. It doesn’t provide direct benefits or cause direct harm, provided it is enjoyed in moderation.
See also: Can you overdose on caffeine?
Some quick extra notes…
That’s all we have time for in myth-busting, but it’s worth noting before we close that coffee has a lot of health benefits; we didn’t cover them today because they’re not contentious, but they are interesting nevertheless:
- Coffee is the world’s biggest source of antioxidants
- 65% reduced risk of Alzheimer’s for coffee-drinkers
- 67% reduced risk of type 2 diabetes for coffee-drinkers
- 43% reduced risk of liver cancer for coffee-drinkers
- 53% reduced suicide risk for coffee-drinkers
Enjoy!
Share This Post
-
Mental Health Courts Can Struggle to Fulfill Decades-Old Promise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GAINESVILLE, Ga. — In early December, Donald Brown stood nervously in the Hall County Courthouse, concerned he’d be sent back to jail.
The 55-year-old struggles with depression, addiction, and suicidal thoughts. He worried a judge would terminate him from a special diversion program meant to keep people with mental illness from being incarcerated. He was failing to keep up with the program’s onerous work and community service requirements.
“I’m kind of scared. I feel kind of defeated,” Brown said.
Last year, Brown threatened to take his life with a gun and his family called 911 seeking help, he said. The police arrived, and Brown was arrested and charged with a felony of firearm possession.
After months in jail, Brown was offered access to the Health Empowerment Linkage and Possibilities, or HELP, Court. If he pleaded guilty, he’d be connected to services and avoid prison time. But if he didn’t complete the program, he’d possibly face incarceration.
“It’s almost like coercion,” Brown said. “‘Here, sign these papers and get out of jail.’ I feel like I could have been dealt with a lot better.”
Advocates, attorneys, clinicians, and researchers said courts such as the one Brown is navigating can struggle to live up to their promise. The diversion programs, they said, are often expensive and resource-intensive, and serve fewer than 1% of the more than 2 million people who have a serious mental illness and are booked into U.S. jails each year.
People can feel pressured to take plea deals and enter the courts, seeing the programs as the only route to get care or avoid prison time. The courts are selective, due in part to political pressures on elected judges and prosecutors. Participants must often meet strict requirements that critics say aren’t treatment-focused, such as regular hearings and drug screenings.
And there is a lack of conclusive evidence on whether the courts help participants long-term. Some legal experts, like Lea Johnston, a professor of law at the University of Florida, worry the programs distract from more meaningful investments in mental health resources.
Jails and prisons are not the place for individuals with mental disorders, she said. “But I’m also not sure that mental health court is the solution.”
The country’s first mental health court was established in Broward County, Florida, in 1997, “as a way to promote recovery and mental health wellness and avoid criminalizing mental health problems.” The model was replicated with millions in funding from such federal agencies as the Substance Abuse and Mental Health Services Administration and the Department of Justice.
More than 650 adult and juvenile mental health courts were operational as of 2022, according to the National Treatment Court Resource Center. There’s no set way to run them. Generally, participants receive treatment plans and get linked to services. Judges and mental health clinicians oversee their progress.
Researchers from the center found little evidence that the courts improve participants’ mental health or keep them out of the criminal justice system. “Few studies … assess longer-term impacts” of the programs “beyond one year after program exit,” said a 2022 policy brief on mental health courts.
The courts work best when paired with investments in services such as clinical treatment, recovery programs, and housing and employment opportunities, said Kristen DeVall, the center’s co-director.
“If all of these other supports aren’t invested in, then it’s kind of a wash,” she said.
The courts should be seen as “one intervention in that larger system,” DeVall said, not “the only resource to serve folks with mental health needs” who get caught up in the criminal justice system.
Resource limitations can also increase the pressures to apply for mental health court programs, said Lisa M. Wayne, executive director of the National Association of Criminal Defense Lawyers. People seeking help might not feel they have alternatives.
“It’s not going to be people who can afford mental health intervention. It’s poor people, marginalized folks,” she said.
Other court skeptics wonder about the larger costs of the programs.
In a study of a mental health court in Pennsylvania, Johnston and a University of Florida colleague found participants were sentenced to longer time under government supervision than if they’d gone through the regular criminal justice system.
“The bigger problem is they’re taking attention away from more important solutions that we should be investing in, like community mental health care,” Johnston said.
When Melissa Vergara’s oldest son, Mychael Difrancisco, was arrested on felony gun charges in Queens in May 2021, she thought he would be an ideal candidate for the New York City borough’s mental health court because of his diagnosis of autism spectrum disorder and other behavioral health conditions.
She estimated she spent tens of thousands of dollars to prepare Difrancisco’s case for consideration. Meanwhile, her son sat in jail on Rikers Island, where she said he was assaulted multiple times and had to get half a finger amputated after it was caught in a cell door.
In the end, his case was denied diversion into mental health court. Difrancisco, 22, is serving a prison sentence that could be as long as four years and six months.
“There’s no real urgency to help people with mental health struggles,” Vergara said.
Critics worry such high bars to entry can lead the programs to exclude people who could benefit the most. Some courts don’t allow those accused of violent or sexual crimes to participate. Prosecutors and judges can face pressure from constituents that may lead them to block individuals accused of high-profile offenses.
And judges often aren’t trained to make decisions about participants’ care, said Raji Edayathumangalam, senior policy social worker with New York County Defender Services.
“It’s inappropriate,” she said. “We’re all licensed to practice in our different professions for a reason. I can’t show up to do a hernia operation just because I read about it or sat next to a hernia surgeon.”
Mental health courts can be overly focused on requirements such as drug testing, medication compliance, and completing workbook assignments, rather than progress toward recovery and clinical improvement, Edayathumangalam said.
Completing the programs can leave some participants with clean criminal records. But failing to meet a program’s requirements can trigger penalties — including incarceration.
During a recent hearing in the Clayton County Behavioral Health Accountability Court in suburban Atlanta, one woman left the courtroom in tears when Judge Shana Rooks Malone ordered her to report to jail for a seven-day stay for “being dishonest” about whether she was taking court-required medication.
It was her sixth infraction in the program — previous consequences included written assignments and “bench duty,” in which participants must sit and think about their participation in the program.
“I don’t like to incarcerate,” Malone said. “That particular participant has had some challenges. I’m rooting for her. But all the smaller penalties haven’t worked.”
Still, other participants praised Malone and her program. And, in general, some say such diversion programs provide a much-needed lifeline.
Michael Hobby, 32, of Gainesville was addicted to heroin and fentanyl when he was arrested for drug possession in August 2021. After entry into the HELP Court program, he got sober, started taking medication for anxiety and depression, and built a stable life.
“I didn’t know where to reach out for help,” he said. “I got put in handcuffs, and it saved my life.”
Even as Donald Brown awaited his fate, he said he had started taking medication to manage his depression and has stayed sober because of HELP Court.
“I’ve learned a new way of life. Instead of getting high, I’m learning to feel things now,” he said.
Brown avoided jail that early December day. A hearing to decide his fate could happen in the next few weeks. But even if he’s allowed to remain in the program, Brown said, he’s worried it’s only a matter of time before he falls out of compliance.
“To try to improve myself and get locked up for it is just a kick in the gut,” he said. “I tried really hard.”
KFF Health News senior correspondent Fred Clasen-Kelly contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Walking can prevent low back pain, a new study shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you suffer from low back pain that recurs regularly? If you do, you’re not alone. Roughly 70% of people who recover from an episode of low back pain will experience a new episode in the following year.
The recurrent nature of low back pain is a major contributor to the enormous burden low back pain places on individuals and the health-care system.
In our new study, published today in The Lancet, we found that a program combining walking and education can effectively reduce the recurrence of low back pain.
PeopleImages.com – Yuri A/Shutterstock The WalkBack trial
We randomly assigned 701 adults who had recently recovered from an episode of low back pain to receive an individualised walking program and education (intervention), or to a no treatment group (control).
Participants in the intervention group were guided by physiotherapists across six sessions, over a six-month period. In the first, third and fifth sessions, the physiotherapist helped each participant to develop a personalised and progressive walking program that was realistic and tailored to their specific needs and preferences.
The remaining sessions were short check-ins (typically less than 15 minutes) to monitor progress and troubleshoot any potential barriers to engagement with the walking program. Due to the COVID pandemic, most participants received the entire intervention via telehealth, using video consultations and phone calls.
Low back pain can be debilitating. Karolina Kaboompics/Pexels The program was designed to be manageable, with a target of five walks per week of roughly 30 minutes daily by the end of the six-month program. Participants were also encouraged to continue walking independently after the program.
Importantly, the walking program was combined with education provided by the physiotherapists during the six sessions. This education aimed to give people a better understanding of pain, reduce fear associated with exercise and movement, and give people the confidence to self-manage any minor recurrences if they occurred.
People in the control group received no preventative treatment or education. This reflects what typically occurs after people recover from an episode of low back pain and are discharged from care.
What the results showed
We monitored the participants monthly from the time they were enrolled in the study, for up to three years, to collect information about any new recurrences of low back pain they may have experienced. We also asked participants to report on any costs related to their back pain, including time off work and the use of health-care services.
The intervention reduced the risk of a recurrence of low back pain that limited daily activity by 28%, while the recurrence of low back pain leading participants to seek care from a health professional decreased by 43%.
Participants who received the intervention had a longer average period before they had a recurrence, with a median of 208 days pain-free, compared to 112 days in the control group.
In our study, regular walking appeared to help with low back pain. PeopleImages.com – Yuri A/Shutterstock Overall, we also found this intervention to be cost-effective. The biggest savings came from less work absenteeism and less health service use (such as physiotherapy and massage) among the intervention group.
This trial, like all studies, had some limitations to consider. Although we tried to recruit a wide sample, we found that most participants were female, aged between 43 and 66, and were generally well educated. This may limit the extent to which we can generalise our findings.
Also, in this trial, we used physiotherapists who were up-skilled in health coaching. So we don’t know whether the intervention would achieve the same impact if it were to be delivered by other clinicians.
Walking has multiple benefits
We’ve all heard the saying that “prevention is better than a cure” – and it’s true. But this approach has been largely neglected when it comes to low back pain. Almost all previous studies have focused on treating episodes of pain, not preventing future back pain.
A limited number of small studies have shown that exercise and education can help prevent low back pain. However, most of these studies focused on exercises that are not accessible to everyone due to factors such as high cost, complexity, and the need for supervision from health-care or fitness professionals.
On the other hand, walking is a free, accessible way to exercise, including for people in rural and remote areas with limited access to health care.
Walking has a variety of advantages. Cast Of Thousands/Shutterstock Walking also delivers many other health benefits, including better heart health, improved mood and sleep quality, and reduced risk of several chronic diseases.
While walking is not everyone’s favourite form of exercise, the intervention was well-received by most people in our study. Participants reported that the additional general health benefits contributed to their ongoing motivation to continue the walking program independently.
Why is walking helpful for low back pain?
We don’t know exactly why walking is effective for preventing back pain, but possible reasons could include the combination of gentle movements, loading and strengthening of the spinal structures and muscles. It also could be related to relaxation and stress relief, and the release of “feel-good” endorphins, which block pain signals between your body and brain – essentially turning down the dial on pain.
It’s possible that other accessible and low-cost forms of exercise, such as swimming, may also be effective in preventing back pain, but surprisingly, no studies have investigated this.
Preventing low back pain is not easy. But these findings give us hope that we are getting closer to a solution, one step at a time.
Tash Pocovi, Postdoctoral research fellow, Department of Health Sciences, Macquarie University; Christine Lin, Professor, Institute for Musculoskeletal Health, University of Sydney; Mark Hancock, Professor of Physiotherapy, Macquarie University; Petra Graham, Associate Professor, School of Mathematical and Physical Sciences, Macquarie University, and Simon French, Professor of Musculoskeletal Disorders, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
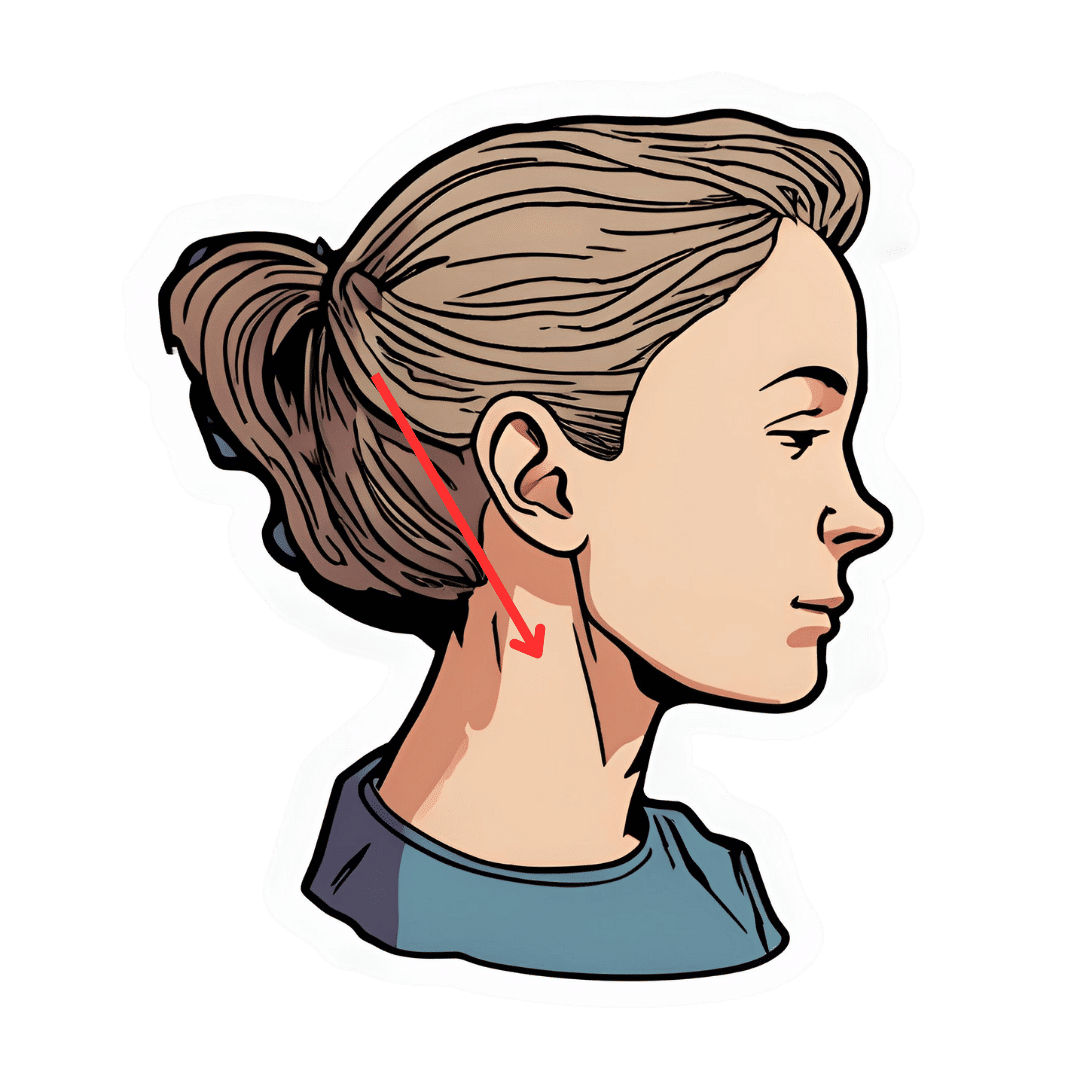
The Vagus Nerve’s Power for Weight Loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Arun Dhir is a university lecturer, a gastrointestinal surgeon, an author, and a yoga and meditation instructor, and he has this to say:
Gut feelings
The vagus nerve is the 10th cranial nerve, also known as “vagus” (“the wanderer”), because it travels from the brain to many other body parts, including the ears, throat, heart, respiratory system, gut, pancreas, liver, and reproductive system. It’s no surprise then, that it plays a key role in brain-gut communication and metabolism regulation.
The vagus nerve is part of the parasympathetic nervous system, responsible for rest, digestion, and counteracting the stress response. Most signals through the vagus nerve travel from the gut to the brain, though there is communication in both directions.
You may be beginning to see how this works and its implications for weight management: the vagus nerve senses metabolites from the liver, pancreas, and small intestine, and regulates insulin production by stimulating beta cells in the pancreas, which is important for avoiding/managing insulin resistance and metabolic syndrome in general.
Dr. Dhir cites a study in which vagus nerve stimulation (originally used for treating epilepsy and depression) was shown to cause unintentional weight loss (6-11%) in patients, revealing a link to weight management. Of course, that is quite a specific sample, so more research is needed to say for sure, but because the principle is very sound and the mechanism of action is clear, it’s not being viewed as a controversial conclusion.
As for how get these benefits, here are seven ways:
- Cold water on the face: submerge your face in cold water in the morning while holding water in your mouth, or cover your face with a cold wet washcloth (while holding your breath please; no need to waterboard yourself!), which activates the “mammalian dive response” in which your body activates the parasympathetic nervous system in order to remain calm and thus survive for longer underwater
- Alternate hot and cold showers: switch between hot and cold water during showers for 10-second intervals; this creates eustress and activates the process of hormesis, improving your overall stress management and reducing any chronic stress response you may otherwise have going on
- Humming and gargling: the vibrations in the throat stimulate the nearby vagus nerve
- Deep breathing (pranayama): yoga breathing exercises, especially combined with somatic exercises such as the sun salutation, can stimulate the vagus nerve
- Intermittent fasting: helps recalibrate the metabolism and indirectly improves vagus nerve function
- Massage and acupressure: stimulates lymphatic channels and the vagus nerve
- Long walks in nature (“forest bathing”): helps trigger relaxation in general
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Vagus Nerve (And How You Can Make Use Of It)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Calorie Myth – by Jonathan Bailor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First we’ll mention: the author is not a doctor, but the book is endorsed by assorted well-known doctors in the field, and the science described is consistent with current scientific consensus (and, for that matter, consistent with what we wrote in our mythbusting feature: Are You A Calorie-Burning Machine?).
It’s often (correctly) said that “not all calories are created equal”, but how should we quantify them? He proposes his “SANE solution”, which is based around the ideas of:
- Satiety: how quickly calories fill us up
- Aggression: how likely calories are to be stored as fat
- Nutrition: how many micronutrients calories bring with them, and how much
- Efficiency: how easily calories are converted
To this end, he recommends a diet high in foods that score well on his “SANE” factors, and provides such things as recipes, meal plans etc to help, as well principles for exercising more usefully in the context of metabolic base rate, and moving (rather than fighting) one’s “set point”, which is usually associated with one’s weight but it really has more to do with metabolic base rate. In fact, Bailor recommends throwing out the bathroom scale and focusing on pursuing good health itself, rather than obsessing over changing one’s relationship with the Earth’s gravitational field.
Yes, it says “lose weight” in the subtitle, but the idea is that this will be a by-product rather than the thing actively pursued. After all, we can control our actions, so that input variable is where we should put our focus, not the output variable of the numbers on the scale which can often be misleading (muscle weighing more than fat, tendency to water weight fluctuations, etc).
The style is a little flashy and salesy for this reviewer’s personal taste (a lot of references to his own businesses and neologisms associated with such), but it doesn’t take away from the quality of the content, and in terms of science, study references come at a rate of about one per page on average.
Bottom line: if you’d like to rethink your relationship with calories, then this book can help give you a much more practical angle.
Click here to check out The Calorie Myth, and take control of your metabolic base rate!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why You Should Diversify Your Nuts!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Time to go nuts for nuts!
Nuts, in popular perception, range from “basically the healthiest food anyone can eat” to “basically high calorie salty snacks”. And, they can be either!
Some notes, then:
- Raw is generally better that not
- Dry roasted is generally better than the kind with added oils
- Added salt is neither necessary nor good
Quick tip: if “roasted salted” are the cheapest or most convenient to buy, you can at least mitigate that by soaking them in warm water for 5 minutes, before rinsing and (if you don’t want wet nuts) drying.
You may be wondering: who does want wet nuts? And the answer is, if for example you’re making a delicious cashew and chickpea balti, the fact you didn’t dry them before throwing them in won’t make a difference.
Now, let’s do a quick run-down; we don’t usually do “listicles” but it seemed a good format here, so we’ve picked a top 5 for nutritional potency:
Almonds
We may have a bias. We accept it. But almonds are also one of the healthiest nuts around, and generally considered by most popular metrics the healthiest.
Not only are they high in protein, healthy fat, fiber, vitamins, and minerals, but they’re even a natural prebiotic that increases the populations of healthy gut bacteria, while simultaneously keeping down the populations of gut pathogens—what more can we ask of a nut?
Read more: Prebiotic effects of almonds and almond skins on intestinal microbiota in healthy adult humans
Pistachios
Not only are these super tasty and fun to eat (and mindful eating is all but guaranteed, as shelling them by hand slows us down and makes us more likely to eat them one at a time rather than by the handful), but also they contain lots of nutrients and are lower in calories than most nuts, so they’re a great option for anyone who’d like to eat more nuts but is doing a calorie-controlled diet and doesn’t want to have half a day’s calories in a tiny dish of nuts.
Walnuts
Popularly associated with brain health (perhaps easy to remember because of their appearance), they really are good for the brain:
Check it out: Beneficial Effects of Walnuts on Cognition and Brain Health
Cashews
A personal favorite of this writer for their versatility in cooking, food prep, or just as a snack, they also do wonders for metabolic health:
Brazil nuts
The most exciting thing about these nuts is that they’re an incredibly potent source of selenium, which is important not just for hair/skin/nails as popularly marketed, but also for thyroid hormone production and DNA synthesis.
But don’t eat too many, because selenium is definitely one of those “you can have too much of a good thing” nutrients, and selenium poisoning can make your hair (however beautiful and shiny it got because of the selenium) fall out if you take too much.
Know the numbers: Brazil nuts and selenium—health benefits and risks
Bottom line on nuts:
- Nuts are a great and healthful part of almost anyone’s diet
- Obviously, if you have a nut allergy, then we’re sorry; this one won’t have helped you so much
- Almonds are one of the most healthful nuts out there
- Brazil nuts are incredibly potent, to the point where moderation is recommended
- A handful of mixed nuts per day is a very respectable option—when it comes to food and health, diversity is almost always good!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: