Sweet Cinnamon vs Regular Cinnamon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sweet cinnamon to regular cinnamon, we picked the sweet.
Why?
In this case, it’s not close. One of them is health-giving and the other is poisonous (but still widely sold in supermarkets, especially in the US and Canada, because it is cheaper).
It’s worth noting that “regular cinnamon” is a bit of a misnomer, since sweet cinnamon is also called “true cinnamon”. The other cinnamon’s name is formally “cassia cinnamon”, but marketers don’t tend to call it that, preferring to calling it simply “cinnamon” and hope consumers won’t ask questions about what kind, because it’s cheaper.
Note: this too is especially true in the US and Canada, where for whatever reason sweet cinnamon seems to be more difficult to obtain than in the rest of the world.
In short, both cinnamons contain cinnamaldehyde and coumarin, but:
- Sweet/True cinnamon contains only trace amounts of coumarin
- Regular/Cassia cinnamon contains about 250x more coumarin
Coumarin is heptatotoxic, meaning it poisons the liver, and the recommended safe amount is 0.1mg/kg, so it’s easy to go over that with just a couple of teaspoons of cassia cinnamon.
You might be wondering: how can they get away with selling something that poisons the liver? In which case, see also: the alcohol aisle. Selling toxic things is very common; it just gets normalized a lot.
Cinnamaldehyde is responsible for cinnamon’s healthier properties, and is found in reasonable amounts in both cinnamons. There is about 50% more of it in the regular/cassia than in the sweet/true, but that doesn’t come close to offsetting the potential harm of its higher coumarin content.
Want to learn more?
You may like to read:
- A Tale Of Two Cinnamons ← this one has more of the science of coumarin toxicity, as well as discussing (and evidencing) cinnamaldehyde’s many healthful properties against inflammation, cancer, heart disease, neurodegeneration, etc
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cold Medicines & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold Medicines & Heart Health
In the wake of many decongestants disappearing from a lot of shelves after a common active ingredient being declared useless*, you may find yourself considering alternative decongestants at this time of year.
*In case you missed it:
It doesn’t seem to be dangerous, by the way, just also not effective:
FDA Panel Says Common OTC Decongestant, Phenylephrine, Is Useless
Good for your nose, bad for your heart?
With products based on phenylephrine out of the running, products based on pseudoephedrine, a competing drug, are enjoying a surge in popularity.
Good news: pseudoephedrine works!
Bad news: pseudoephedrine works because it is a vasoconstrictor, and that vasoconstriction reduces nasal swelling. That same vasoconstriction also raises overall blood pressure, potentially dangerously, depending on an assortment of other conditions you might have.
Further reading: Can decongestants spike your blood pressure? What to know about hypertension and cold medicine
Who’s at risk?
The warning label, unread by many, reads:
❝Do not use this product if you have heart disease, high blood pressure, thyroid disease, diabetes, or difficulty in urination due to enlargement of the prostate gland, unless directed by a doctor❞
Source: Harvard Health | Don’t let decongestants squeeze your heart
What are the other options?
The same source as above recommends antihistamines as an option to be considered, citing:
❝Antihistamines such as […] cetirizine (Zyrtec) and loratadine (Claritin) can help with a stuffy nose and are safe for the heart.❞
But we’d be remiss not to mention drug-free options too, for example:
- Saline rinse with a neti pot or similar
- Use of a humidifier in your house/room
- Steam inhalation, with or without eucalyptus etc
See also: Inhaled Eucalyptus’s Immunomodulatory and Antimicrobial Effects
Take care!
Share This Post
-
Anti-Inflammatory Diet 101 (What to Eat to Fight Inflammation)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic inflammation is a cause and/or exacerbating factor in very many diseases. Arthritis, diabetes, and heart disease are probably top of the list, but there are lots more where they came from. And, it’s good to avoid those things. So, how to eat to avoid inflammation?
Let food be thy medicine
The key things to keep in mind, the “guiding principles” are to prioritize whole, minimally-processed foods, and enjoy foods with plenty of antioxidants. Getting a healthy balance of omega fatty acids is also important, which for most people means getting more omega-3 and less omega-6.
Shopping list (foods to prioritize) includes:
- fruits and vegetables in a variety of colors (e.g. berries, leafy greens, beats)
- whole grains, going for the most fiber-rich options (e.g. quinoa, brown rice, oats)
- healthy fats (e.g. avocados, nuts, seeds)
- fatty fish (e.g. salmon, mackerel, sardines) ← don’t worry about this if you’re vegetarian/vegan though, as the previous category can already cover it
- herbs and spices (e.g. turmeric, garlic, ginger)
Noping list (foods to avoid) includes:
- refined carbohydrates
- highly processed and/or fried foods
- red meats and/or processed meats (yes, that does mean that organic grass-fed farmers’ pinky-promise-certified holistically-raised beef is also off the menu)
- dairy products, especially if unfermented
For more information on each of these, plus advice on transitioning away from an inflammatory diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How to Prevent (or Reduce) Inflammation
Take care!
Share This Post
-
Sunflower Seeds vs Sesame Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower seeds to sesame seeds, we picked the sunflower.
Why?
In moderation, both are very healthy. We say “in moderation” because they’re both about 50% fat and such fats, while vital for life, are generally best enjoyed in small portions. Of that fat, sunflower has the slightly better fat profile; they’re both mostly poly- and monounsaturated fats, but sunflower has 10% saturated fat while sesame has 15%. Aside from fats, sunflower has slightly more protein and sesame has slightly more carbs. While sesame has slightly more fiber, because of the carb profile sunflower still has the lower glycemic index. All in all, a moderate win for sunflower in the macros category.
You may be wondering, with all that discussion of fats, what they’re like for omega-3, and sesame seeds have more omega-3, though sunflower seeds contain it too. Still, a point in sesame’s favor here.
When it comes to vitamins, sunflower has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, and choline, while sesame is not higher in any vitamins.
In the category of minerals, sunflower has more phosphorus, potassium, and selenium, while sesame has more calcium, copper, iron, and zinc. This is nominally a marginal win for sesame, but it should be noted that sunflower is still very rich in copper, iron, and zinc too (but not calcium).
Adding up the categories makes for a moderate win for sunflower seeds, but as ever, enjoy both; diversity is best!
Want to learn more?
You might like to read:
Sunflower Seeds vs Pumpkin Seeds – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Avocado vs Jackfruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to jackfruit, we picked the avocado.
Why?
In terms of macros, avocado is higher in fats (famously healthy ones, including a good dose of omega-3), fiber (nearly 5x more), and protein (despite jackfruit being more often used as a meaty element in recipes, avocado has slightly more). Meanwhile, jackfruit is about 3x higher in carbs. All in all, a clear win for avocado.
Looking at vitamins, avocado has more of vitamins A, B2, B3, B5, B7, B9, E, K, and choline, while jackfruit has more of vitamins B1, B6, and C. Another win for avocado in this category.
In the category of minerals, avocado has more copper, iron, manganese, phosphorus, potassium, selenium, and zinc, while jackfruit has more calcium. One more win for avocado.
Adding up the sections makes for an easy overall win for avocado, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
Jackfruit vs Durian – Which is Healthier? ← including some fun durian facts (such as how to pick a good one, and what happens if you eat durian and drink alcohol)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ketogenic Diet: Burning Fat Or Burning Out?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
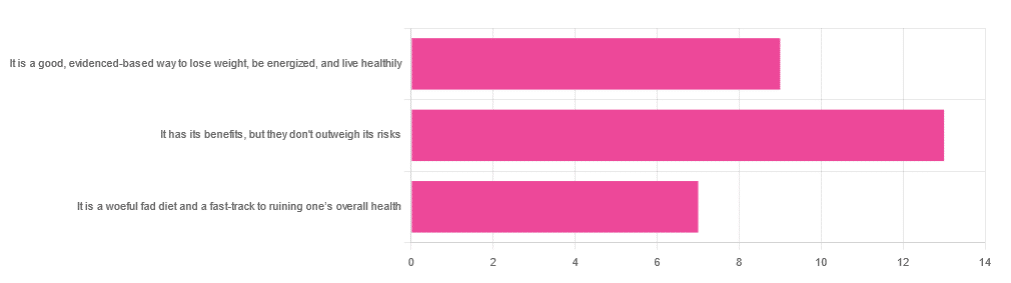
In Wednesday’s newsletter, we asked you for your opinion of the keto diet, and got the above-depicted, below-described set of responses:
- About 45% said “It has its benefits, but they don’t outweigh the risks”
- About 31% said “It is a good, evidence-based way to lose weight, be energized, and live healthily”
- About 24% said “It is a woeful fad diet and a fast-track to ruining one’s overall health”
So what does the science say?
First, what is the ketogenic diet?
There are two different stories here:
- Per science, it’s a medical diet designed to help treat refractory epilepsy in children.
- Per popular lore, it’s an energizing weight loss diet for Instagrammers and YouTubers.
Can it be both? The answer is: yes, but with some serious caveats, which we’ll cover over the course of today’s feature.
The ketogenic diet works by forcing the body to burn fat for energy: True or False?
True! This is why it helps for children with refractory epilepsy. By starving the body (including the brain) of glucose, the liver must convert fat into fatty acids and ketones, which latter the brain (and indeed the rest of the body) can now use for energy instead of glucose, thus avoiding one of the the main triggers of refractory epilepsy in children.
See: The Ketogenic Diet: One Decade Later | Pediatrics
Even the pediatric epilepsy studies, however, conclude it does have unwanted side effects, such as kidney stones, constipation, high cholesterol, and acidosis:
Source: Dietary Therapies for Epilepsy
The ketogenic diet is good for weight loss: True or False?
True! Insofar as it does cause weight loss, often rapidly. Of course, so do diarrhea and vomiting, but these are not usually held to be healthy methods of weight loss. As for keto, a team of researchers recently concluded:
❝As obesity rates in the populace keep rising, dietary fads such as the ketogenic diet are gaining traction.
Although they could help with weight loss, this study had a notable observation of severe hypercholesterolemia and increased risk of atherosclerotic cardiovascular disease among the ketogenic diet participants.❞
~ Dr. Shadan Khdher et al.
On which note…
The ketogenic diet is bad for the heart: True or False?
True! As Dr. Joanna Popiolek-Kalisz concluded recently:
❝In terms of cardiovascular mortality, the low-carb pattern is more beneficial than very low-carbohydrate (including the ketogenic diet). There is still scarce evidence comparing ketogenic to the Mediterranean diet.
Other safety concerns in cardiovascular patients such as adverse events related to ketosis, fat-free mass loss, or potential pharmacological interactions should be also taken into consideration in future research.❞
~ Dr. Joanna Popiolek-Kalisz
Read in full: Ketogenic diet and cardiovascular risk: state of the art review
The ketogenic diet is good for short-term weight loss, but not long-term maintenance: True or False?
True! Again, insofar as it works in the short term. It’s not the healthiest way to lose weight and we don’t recommend it, but it did does indeed precipitate short-term weight loss. Those benefits are not typically observed for longer than a short time, though, as the above-linked paper mentions:
❝The ketogenic diet does not fulfill the criteria of a healthy diet. It presents the potential for rapid short-term reduction of body mass, triglycerides level, Hb1Ac, and blood pressure.
Its efficacy for weight loss and the above-mentioned metabolic changes is not significant in long-term observations.❞
~ Ibid.
The ketogenic diet is a good, evidence-based way to lose weight, be energized, and live healthily: True or False?
False, simply, as you may have gathered from the above, but we’ve barely scratched the surface in terms of the risks.
That said, as mentioned, it will induce short-term weight loss, and as for being energized, typically there is a slump-spike-slump in energy:
- At first, the body is running out of glucose, and so naturally feels weak and tired.
- Next, the body enters ketosis, and so feels energized and enlivened ← this is the part where the popular enthusiastic reviews come from
- Then, the body starts experiencing all the longer-term problems associated with lacking carbohydrates and having an overabundance of fat, so becomes gradually more sick and tired.
Because of this, the signs of symptoms of being in ketosis (aside from: measurably increased ketones in blood, breath, and urine) are listed as:
- Bad breath
- Weight loss
- Appetite loss
- Increased focus and energy
- Increased fatigue and irritability
- Digestive issues
- Insomnia
The slump-spike-slump we mentioned is the reason for the seemingly contradictory symptoms of increased energy and increased fatigue—you get one and then the other.
Here’s a small but illustrative study, made clearer by its participants being a demographic whose energy levels are most strongly affected by dietary factors:
The ketogenic diet is a woeful fad diet and a fast-track to ruining one’s overall health: True or False?
True, subjectively in the first part, as it’s a little harsher than we usually go for in tone, though it has been called a fad diet in scientific literature. The latter part (ruining one’s overall health) is observably true.
One major problem is incidental-but-serious, which is that a low-carb diet is typically a de facto low-fiber diet, which is naturally bad for the gut and heart.
Other things are more specific to the keto diet, such as the problems with the kidneys:
However, kidney stones aren’t the worst of the problems:
Is Losing Weight Worth Losing Your Kidney: Keto Diet Resulting in Renal Failure
We’re running out of space and the risks associated with the keto diet are many, but for example even in the short term, it already increases osteoporosis risk:
❝Markers of bone modeling/remodeling were impaired after short-term low-carbohydrate high-fat diet, and only one marker of resorption recovered after acute carbohydrate restoration❞
~ Dr. Ida Heikura et al.
A Short-Term Ketogenic Diet Impairs Markers of Bone Health in Response to Exercise
Want a healthier diet?
We recommend the Mediterranean diet.
See also: Four Ways To Upgrade The Mediterranean
(the above is about keeping to the Mediterranean diet, while tweaking one’s choices within it for a specific extra health focus such as an anti-inflammatory upgrade, a heart-healthy upgrade, a gut-healthy upgrade, and a brain-healthy upgrade)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
90% Of People Skip This Essential Exercise—Are You One Of Them?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Single-leg strengthening is essential for joint health at any age (unless you want to bunny-hop up and down the stairs with both feet at once, for example), yet many people overlook it. This neglect often leads to pain, stiffness, and a higher risk of injury.
Dr. Alyssa Kuhn, arthritis specialist, explains how to do it:
On the rise
In this video, different exercise variations—beginner, intermediate, and advanced—are presented to help you build strength at your own pace:
Beginner: start by using a chair, adding a cushion for support if needed. Sit at the edge and position one foot slightly in front of the other in a staggered stance. Stand up and sit down in a controlled manner, allowing the back leg to bear more weight and work harder than the front leg. Do 8–10 repetitions per side and pay attention to whether one side feels weaker. To build strength, incorporate this movement into daily activities, such as standing up from the couch. Master this variation before progressing, to avoid knee injury.
Intermediate: to make the exercise more challenging, you can either use a lower chair, or extend your front foot further out, shifting more weight to your back leg. Only modify one variable at a time to maintain control. Do 8–10 repetitions per side, ensuring proper form. A common mistake is allowing the back knee to move inward, which can cause knee stress. To prevent this, use a mirror to check your form and keep the knee and ankle aligned during movement.
Advanced: when you’re ready, extend your front leg completely with the heel on the ground and toes up, removing its stability and forcing the back leg to work even harder. Maintain controlled movement while keeping your knee and ankle aligned. Repeat the exercise on both sides, focusing extra effort on the weaker leg to build balanced strength.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
The Secret To Better Squats: Foot, Knee, & Ankle Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: